Back

Poster Session E - Tuesday Afternoon
Category: Stomach
E0699 - Eosinophilic Gastritis as a Differential Diagnosis in the Setting of Chronic Abdominal Pain
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Jarin Prasa, DO
Staten Island University Hospital
Staten Island, New York
Presenting Author(s)
Jarin Prasa, DO, Mira Alsheikh, MD, Joseph Aboujaoude, MD
Staten Island University Hospital, Staten Island, NY
Introduction: Eosinophilic gastritis (EoG) is a rare entity, found in 9 to 28 per 100,000 individuals in the United States. It is characterized by eosinophilic infiltration of the bowel wall, causing symptoms that are nonspecific, leaving EoG often underdiagnosed and clinicians perplexed on the management of their patients.
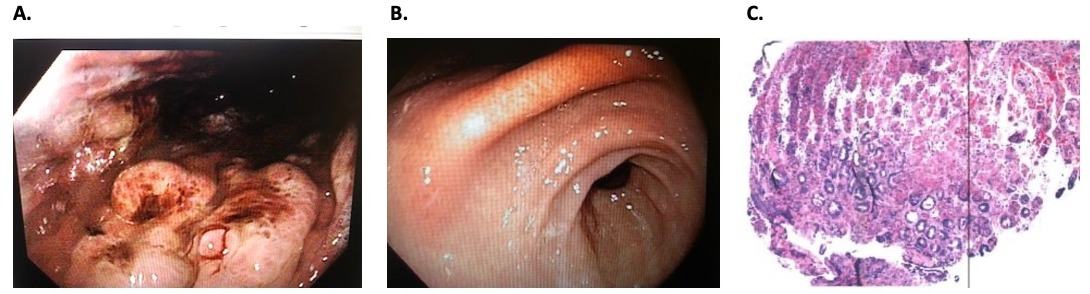
Case Description/Methods: A 43 year old woman with asthma, GERD, and diabetes mellitus, presented with epigastric non radiating abdominal pain. She denied weight loss, nausea, vomiting, diarrhea or constipation. She doesn’t smoke, drink alcohol or use recreational drugs. Her abdomen was soft and tender in epigastric area but otherwise unremarkable. Laboratory workup revealed a normal white blood cell count but with an elevated eosinophil count of 910 per uL. IgE level was also elevated 156 KU/L (normal< 100 KU/L). Abdominal ultrasound revealed cholelithiasis for which she had a cholecystectomy, however, her pain persisted. Subsequent upper endoscopy revealed erythematous gastric folds with diffuse erosions and prominent folds in the proximal body. The pathology from the antrum and body showed prominent infiltration of eosinophils in the lamina propria and the glands, no parasites were identified. Immunostains for CD25 show no evidence of mast cell abnormalities and stains for Helicobacter pylori were negative. The food allergy panel was negative as well as repeated stool tests for ova and parasites. The patient was started on 40mg of prednisone for two weeks and her abdominal pain dramatically improved.
Discussion: EoG is an inflammatory and immune mediated disorder characterized by the infiltration of eosinophils in the gastric mucosa. Clinical manifestations are variable and nonspecific. Laboratory tests are significant for elevated peripheral eosinophil count, and IgE level. Endoscopy is essential for diagnosis, with histology showing more than 30 eosinophils per HPF in at least 5HPFs in the absence of known associated causes of eosinophilia. Steroids are the mainstay of therapy, however, there is a high chance of disease recurrence after discontinuing steroids. Food-elimination diet has been tried with success. For induction and maintenance of remission, limited studies have shown that use of Immunosuppressive drugs, leukotriene inhibitors, and immunomodulators can be used.
When routine workup and treatment for chronic abdominal pain is unrevealing, clinicians should consider EoG when pathological specimens show elevated eosinophils, and consider treatment with steroids.
Disclosures:
Jarin Prasa, DO, Mira Alsheikh, MD, Joseph Aboujaoude, MD. E0699 - Eosinophilic Gastritis as a Differential Diagnosis in the Setting of Chronic Abdominal Pain, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Staten Island University Hospital, Staten Island, NY
Introduction: Eosinophilic gastritis (EoG) is a rare entity, found in 9 to 28 per 100,000 individuals in the United States. It is characterized by eosinophilic infiltration of the bowel wall, causing symptoms that are nonspecific, leaving EoG often underdiagnosed and clinicians perplexed on the management of their patients.
Case Description/Methods: A 43 year old woman with asthma, GERD, and diabetes mellitus, presented with epigastric non radiating abdominal pain. She denied weight loss, nausea, vomiting, diarrhea or constipation. She doesn’t smoke, drink alcohol or use recreational drugs. Her abdomen was soft and tender in epigastric area but otherwise unremarkable. Laboratory workup revealed a normal white blood cell count but with an elevated eosinophil count of 910 per uL. IgE level was also elevated 156 KU/L (normal< 100 KU/L). Abdominal ultrasound revealed cholelithiasis for which she had a cholecystectomy, however, her pain persisted. Subsequent upper endoscopy revealed erythematous gastric folds with diffuse erosions and prominent folds in the proximal body. The pathology from the antrum and body showed prominent infiltration of eosinophils in the lamina propria and the glands, no parasites were identified. Immunostains for CD25 show no evidence of mast cell abnormalities and stains for Helicobacter pylori were negative. The food allergy panel was negative as well as repeated stool tests for ova and parasites. The patient was started on 40mg of prednisone for two weeks and her abdominal pain dramatically improved.
Discussion: EoG is an inflammatory and immune mediated disorder characterized by the infiltration of eosinophils in the gastric mucosa. Clinical manifestations are variable and nonspecific. Laboratory tests are significant for elevated peripheral eosinophil count, and IgE level. Endoscopy is essential for diagnosis, with histology showing more than 30 eosinophils per HPF in at least 5HPFs in the absence of known associated causes of eosinophilia. Steroids are the mainstay of therapy, however, there is a high chance of disease recurrence after discontinuing steroids. Food-elimination diet has been tried with success. For induction and maintenance of remission, limited studies have shown that use of Immunosuppressive drugs, leukotriene inhibitors, and immunomodulators can be used.
When routine workup and treatment for chronic abdominal pain is unrevealing, clinicians should consider EoG when pathological specimens show elevated eosinophils, and consider treatment with steroids.
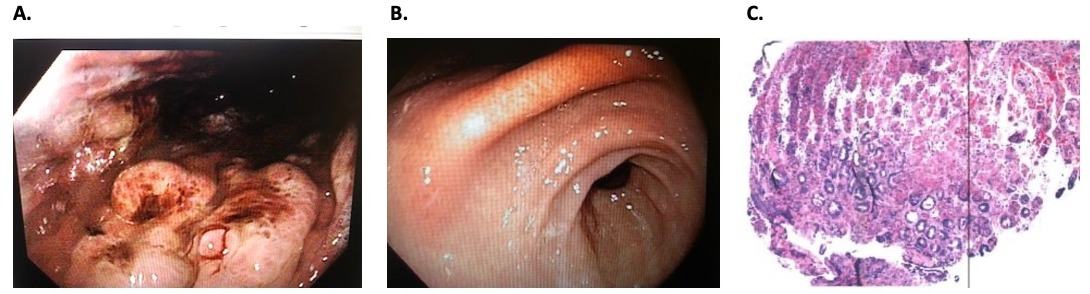
Figure: A. Endoscopic view, Gastric body
B. Endoscopic view, Gastric antrum
C. Histology with prominent intramucosal eosinophils
B. Endoscopic view, Gastric antrum
C. Histology with prominent intramucosal eosinophils
Disclosures:
Jarin Prasa indicated no relevant financial relationships.
Mira Alsheikh indicated no relevant financial relationships.
Joseph Aboujaoude indicated no relevant financial relationships.
Jarin Prasa, DO, Mira Alsheikh, MD, Joseph Aboujaoude, MD. E0699 - Eosinophilic Gastritis as a Differential Diagnosis in the Setting of Chronic Abdominal Pain, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
