Back

Poster Session E - Tuesday Afternoon
Category: Stomach
E0720 - Double Pylorus: A Case of Chronic Peptic Ulcer Disease Leading to Formation of a Gastroduodenal Fistula
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Samantha Whitwell, MD
UTHSC
Memphis, TN
Presenting Author(s)
Samantha Whitwell, MD1, Kyle Kreitman, MD2, Peter D. Snell, DO2
1UTHSC, Memphis, TN; 2University of Tennessee Health Science Center, Memphis, TN
Introduction: Double pylorus is a rare condition, either congenital or acquired, that results in a gastroduodenal fistula, forming an additional connection between the antrum of the stomach and the duodenal bulb.
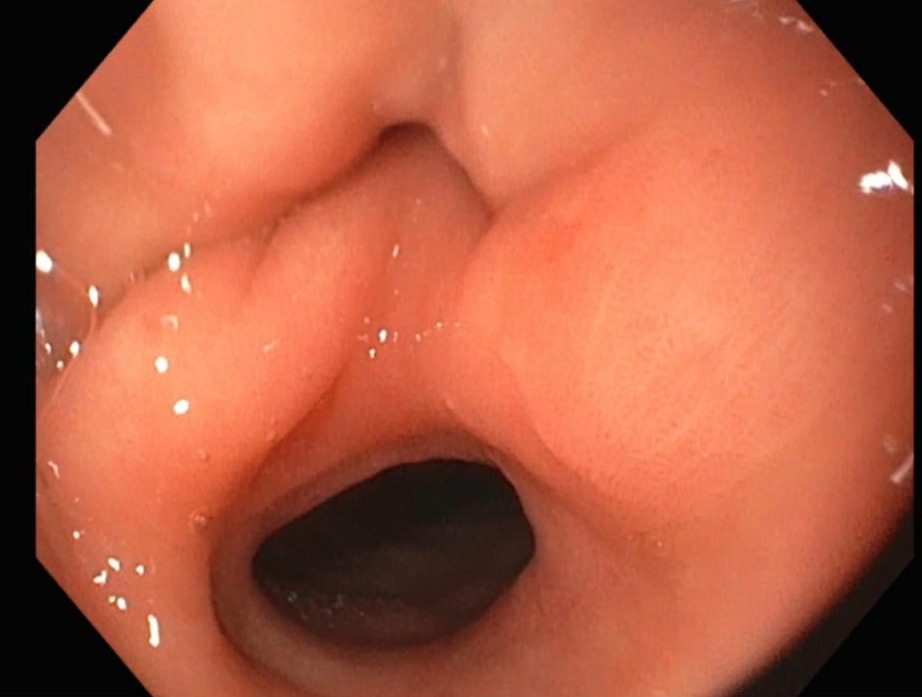
Case Description/Methods: A 75-year-old female with past medical history of cervical cancer (in remission), hypertension, tobacco use, chronic constipation, and peptic ulcer disease (PUD) presented to the emergency department (ED) with diffuse abdominal pain and blood in her stool. Patient reported intermittent black stools with occasional rectal bleeding. She was using non-steroidal anti-inflammatory drugs (NSAIDs) for headaches. In the ED, patient was hypertensive to 170/75, but other vital signs were stable. Her labs showed a hemoglobin of 12.6g/dL (normal 12-16g/dL) without evidence of coagulopathy. Imaging of the abdomen and pelvis did not show any acute findings. Esophagogastroduodenoscopy (EGD) showed two openings to the duodenal bulb, a functional pylorus inferiorly and an accessory channel superiorly (Image A). The two lumens of the duodenum appeared normal without evidence of acute ulceration. Colonoscopy showed a non-bleeding arteriovenous malformation in the proximal ascending colon and internal hemorrhoids, which were likely the cause of her bleeding.
Discussion: Acquired double pylorus (ADP) is usually an incidental finding with a prevalence of approximately 0.001-0.4%, affecting males and females in a 2:1 ratio, respectively. Most cases of ADP are secondary to PUD, often an ulcer in the antrum of the stomach or duodenum penetrating directly into the duodenal bulb. Patients can be asymptomatic with ADP, but some may experience vomiting, epigastric pain, or dyspepsia. Melena may also be present with active ulceration. Initial diagnostic approach to ADP should include EGD, assessing NSAID or corticosteroid use, and H. pylori testing. Treatment involves proton-pump inhibitor administration or other mucosal protective agents, avoidance of NSAIDs and steroids, and eradication of H. pylori. Endoscopic division of the tissue bridge with a sphincterome should be considered if severe symptoms of gastric outlet obstruction persist. In severe cases where perforation, refractory bleeding and/or obstruction occurs, a surgical consultation should be pursued. The accessory pathway will typically remain patent for life, but rarely, the channel will close completely or merge to form a single connection to the duodenal bulb.
Disclosures:
Samantha Whitwell, MD1, Kyle Kreitman, MD2, Peter D. Snell, DO2. E0720 - Double Pylorus: A Case of Chronic Peptic Ulcer Disease Leading to Formation of a Gastroduodenal Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1UTHSC, Memphis, TN; 2University of Tennessee Health Science Center, Memphis, TN
Introduction: Double pylorus is a rare condition, either congenital or acquired, that results in a gastroduodenal fistula, forming an additional connection between the antrum of the stomach and the duodenal bulb.
Case Description/Methods: A 75-year-old female with past medical history of cervical cancer (in remission), hypertension, tobacco use, chronic constipation, and peptic ulcer disease (PUD) presented to the emergency department (ED) with diffuse abdominal pain and blood in her stool. Patient reported intermittent black stools with occasional rectal bleeding. She was using non-steroidal anti-inflammatory drugs (NSAIDs) for headaches. In the ED, patient was hypertensive to 170/75, but other vital signs were stable. Her labs showed a hemoglobin of 12.6g/dL (normal 12-16g/dL) without evidence of coagulopathy. Imaging of the abdomen and pelvis did not show any acute findings. Esophagogastroduodenoscopy (EGD) showed two openings to the duodenal bulb, a functional pylorus inferiorly and an accessory channel superiorly (Image A). The two lumens of the duodenum appeared normal without evidence of acute ulceration. Colonoscopy showed a non-bleeding arteriovenous malformation in the proximal ascending colon and internal hemorrhoids, which were likely the cause of her bleeding.
Discussion: Acquired double pylorus (ADP) is usually an incidental finding with a prevalence of approximately 0.001-0.4%, affecting males and females in a 2:1 ratio, respectively. Most cases of ADP are secondary to PUD, often an ulcer in the antrum of the stomach or duodenum penetrating directly into the duodenal bulb. Patients can be asymptomatic with ADP, but some may experience vomiting, epigastric pain, or dyspepsia. Melena may also be present with active ulceration. Initial diagnostic approach to ADP should include EGD, assessing NSAID or corticosteroid use, and H. pylori testing. Treatment involves proton-pump inhibitor administration or other mucosal protective agents, avoidance of NSAIDs and steroids, and eradication of H. pylori. Endoscopic division of the tissue bridge with a sphincterome should be considered if severe symptoms of gastric outlet obstruction persist. In severe cases where perforation, refractory bleeding and/or obstruction occurs, a surgical consultation should be pursued. The accessory pathway will typically remain patent for life, but rarely, the channel will close completely or merge to form a single connection to the duodenal bulb.
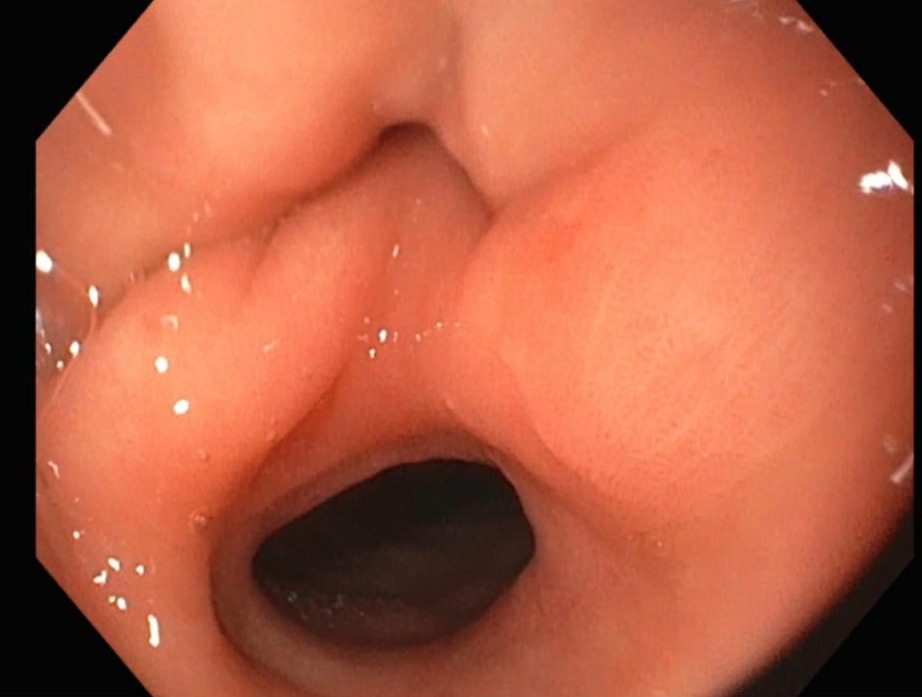
Figure: Image A: Double pylorus on EGD. The accessory channel is observed superiorly, revealing a gastroduodenal fistula.
Disclosures:
Samantha Whitwell indicated no relevant financial relationships.
Kyle Kreitman indicated no relevant financial relationships.
Peter Snell indicated no relevant financial relationships.
Samantha Whitwell, MD1, Kyle Kreitman, MD2, Peter D. Snell, DO2. E0720 - Double Pylorus: A Case of Chronic Peptic Ulcer Disease Leading to Formation of a Gastroduodenal Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
