Back

Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0038 - Non Obstructive Cholangitis with EBV (Epstein Barr Virus) Hepatitis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Mohammad Nabil Rayad, MD
Saint Michael's Medical Center, New York Medical College
Newark, NJ
Presenting Author(s)
Saraswathi Lakkasani, MD1, Scott DiGiacomo, MD, FACG2, Mohammad Nabil Rayad, MD1, Noreen Mirza, MD1
1Saint Michael's Medical Center, New York Medical College, Newark, NJ; 2Saint Michael's Medical Center, Newark, NJ
Introduction: The incidence of EBV causing scleral icterus and cholestasis is less than 5%. In literature, the presence of EBV cholangitis in the absence of underlying cause is unknown. We report a case of EBV associated nonobstructive acute cholangitis.
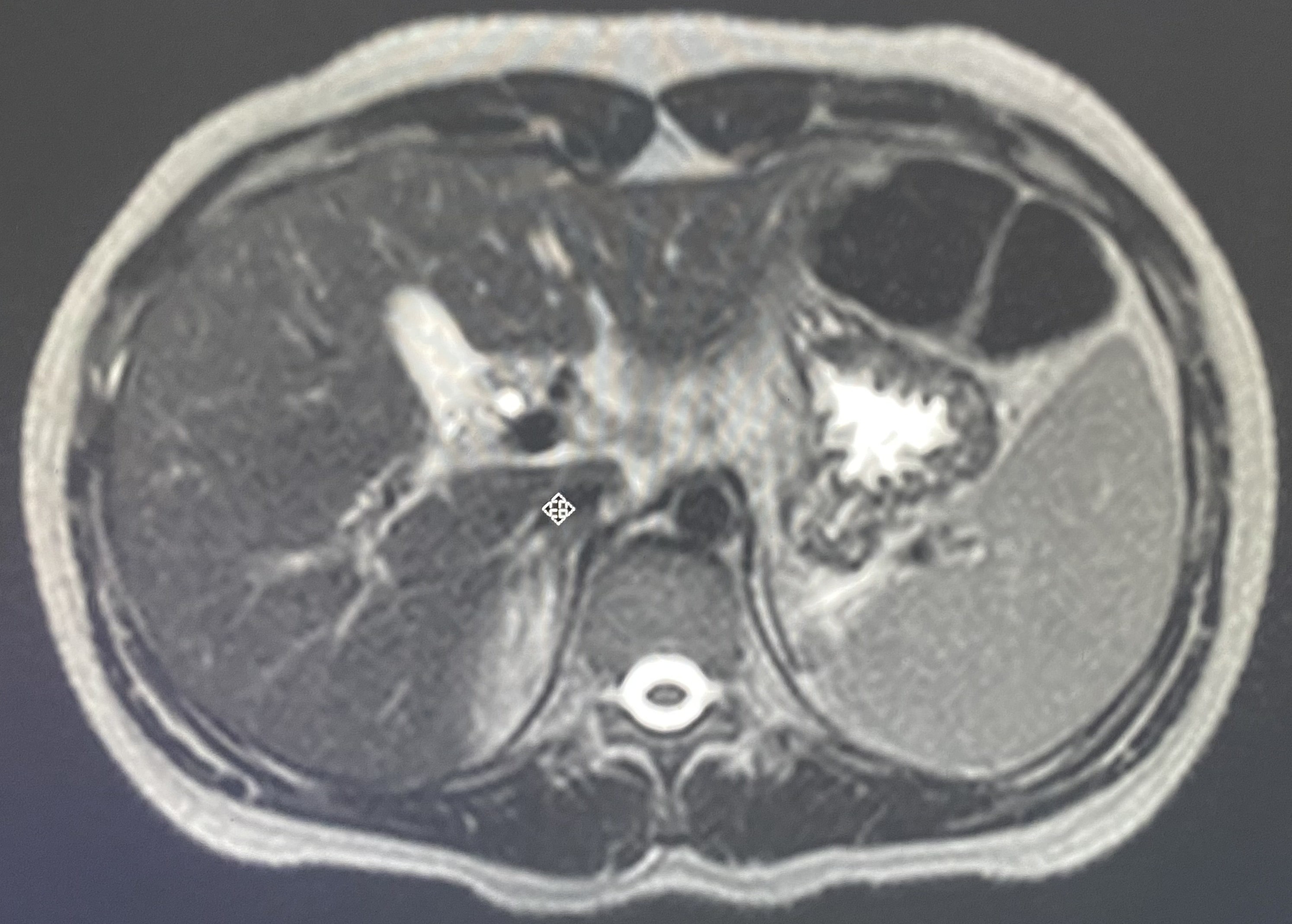
Case Description/Methods: A 21 year old female with history of endometriosis and spina bifida occulta presented with right upper quadrant and epigastric abdominal pain for 4 days. It was non-radiating, colicky with nausea and vomiting. She had fevers and chills with yellow discoloration of her skin, eyes and urine. Vitals were stable. The physical exam was significant for jaundiced skin and scleral icterus with right upper quadrant tenderness and negative Murphy’s sign. On admission, lab results showed hemoglobin of 14.1 g/dl, white blood cell count of 8.5 K cells/ml, and hyperbilirubinemia (5.8). Liver enzymes including aspartate transaminase, alanine transaminase and alkaline phosphatase were elevated at 630, 823 and 355 respectively. Lipase was normal. Abdominal ultrasound showed a severely contracted gallbladder with a thickened wall, and small pericholecystic fluid. MRI revealed inflammation in periportal/peribiliary area, no gallstones and with gallbladder hydrops. The CBD was 5 mm with no intra or extrahepatic biliary dilation.Lab values were only positive for mononucleosis and EBV DNA PCR which showed 2800 copies/mL. No surgical intervention was performed. The patient was treated supportively with analgesics and anti-emetics.
Discussion: We report the first case of primary EBV infection complicated by acute cholangitis. The pathogenesis of EBV associated cholangitis still remains unclear. Our patient imaging showed no stricture or dilatation in the CBD. In 2020, Colbran & Ng reported a case of EBV hepatitis presenting as ascending cholangitis in an immunocompetent patient. Similar to our case, their patient presented with Charcot’s triad; however, our patient had peribiliary inflammatory changes which was not seen in their patient. EBV is capable of decreasing the production of pro-inflammatory cytokines which can interfere with the activity of the bile transport systems and cholestasis could be due to abdominal lymphadenopathy. Thus, for a young patient with acute cholangitis, in the absence of a clear etiology for jaundice, physicians need to be vigilant in ordering EBV workup in order to avoid the overuse of antibiotics, decrease the rate of antibiotic resistance and avoid unnecessary invasive procedures.
Disclosures:
Saraswathi Lakkasani, MD1, Scott DiGiacomo, MD, FACG2, Mohammad Nabil Rayad, MD1, Noreen Mirza, MD1. E0038 - Non Obstructive Cholangitis with EBV (Epstein Barr Virus) Hepatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Saint Michael's Medical Center, New York Medical College, Newark, NJ; 2Saint Michael's Medical Center, Newark, NJ
Introduction: The incidence of EBV causing scleral icterus and cholestasis is less than 5%. In literature, the presence of EBV cholangitis in the absence of underlying cause is unknown. We report a case of EBV associated nonobstructive acute cholangitis.
Case Description/Methods: A 21 year old female with history of endometriosis and spina bifida occulta presented with right upper quadrant and epigastric abdominal pain for 4 days. It was non-radiating, colicky with nausea and vomiting. She had fevers and chills with yellow discoloration of her skin, eyes and urine. Vitals were stable. The physical exam was significant for jaundiced skin and scleral icterus with right upper quadrant tenderness and negative Murphy’s sign. On admission, lab results showed hemoglobin of 14.1 g/dl, white blood cell count of 8.5 K cells/ml, and hyperbilirubinemia (5.8). Liver enzymes including aspartate transaminase, alanine transaminase and alkaline phosphatase were elevated at 630, 823 and 355 respectively. Lipase was normal. Abdominal ultrasound showed a severely contracted gallbladder with a thickened wall, and small pericholecystic fluid. MRI revealed inflammation in periportal/peribiliary area, no gallstones and with gallbladder hydrops. The CBD was 5 mm with no intra or extrahepatic biliary dilation.Lab values were only positive for mononucleosis and EBV DNA PCR which showed 2800 copies/mL. No surgical intervention was performed. The patient was treated supportively with analgesics and anti-emetics.
Discussion: We report the first case of primary EBV infection complicated by acute cholangitis. The pathogenesis of EBV associated cholangitis still remains unclear. Our patient imaging showed no stricture or dilatation in the CBD. In 2020, Colbran & Ng reported a case of EBV hepatitis presenting as ascending cholangitis in an immunocompetent patient. Similar to our case, their patient presented with Charcot’s triad; however, our patient had peribiliary inflammatory changes which was not seen in their patient. EBV is capable of decreasing the production of pro-inflammatory cytokines which can interfere with the activity of the bile transport systems and cholestasis could be due to abdominal lymphadenopathy. Thus, for a young patient with acute cholangitis, in the absence of a clear etiology for jaundice, physicians need to be vigilant in ordering EBV workup in order to avoid the overuse of antibiotics, decrease the rate of antibiotic resistance and avoid unnecessary invasive procedures.
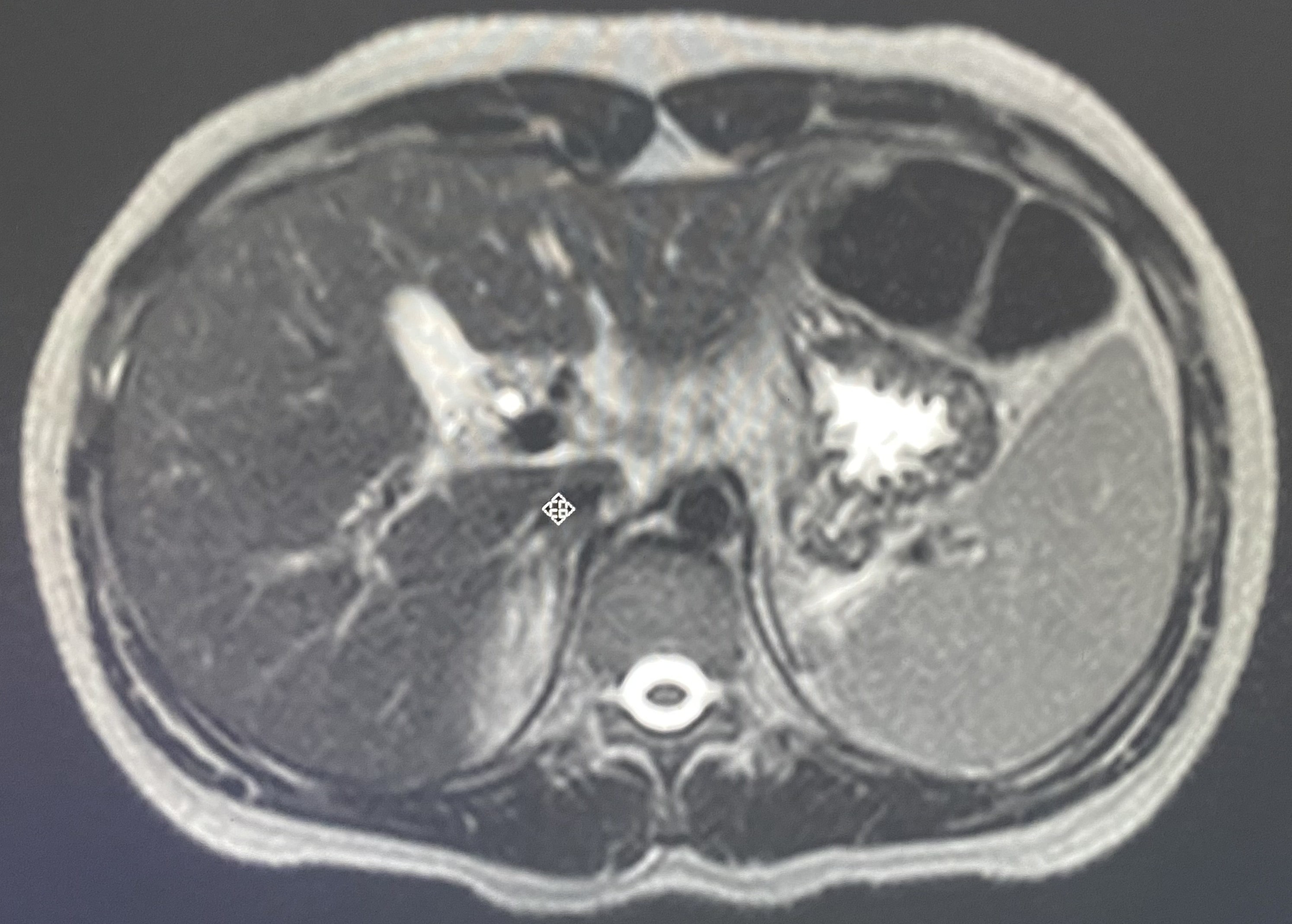
Figure: MRI showing Peribiliary/periportal inflammation
Disclosures:
Saraswathi Lakkasani indicated no relevant financial relationships.
Scott DiGiacomo indicated no relevant financial relationships.
Mohammad Nabil Rayad indicated no relevant financial relationships.
Noreen Mirza indicated no relevant financial relationships.
Saraswathi Lakkasani, MD1, Scott DiGiacomo, MD, FACG2, Mohammad Nabil Rayad, MD1, Noreen Mirza, MD1. E0038 - Non Obstructive Cholangitis with EBV (Epstein Barr Virus) Hepatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
