Back

Poster Session D - Tuesday Morning
Category: IBD
D0376 - Awareness and Perceptions of Colorectal Cancer Risk and Screening in Inflammatory Bowel Disease
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Eleanor Liu, MBChB, MRCP
Northern Care Alliance Trust, NHS
Manchester, England, United Kingdom
Presenting Author(s)
Eleanor K. Liu, MBChB, MRCP1, Aditi Erande, 2, John McLaughlin, BSc, MB ChB, PhD3, Jimmy K. Limdi, MBBS, FACG4
1Northern Care Alliance Trust, NHS, Manchester, England, United Kingdom; 2Metropolis Healthcare, Mumbai, Maharashtra, India; 3University of Manchester, Salford, England, United Kingdom; 4Northern Care Alliance NHS Trust & University of Manchester, Manchester, England, United Kingdom
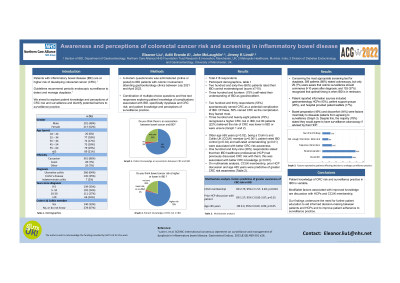
Introduction: Patients with inflammatory bowel disease (IBD) are at higher risk of developing colorectal cancer (CRC). Guidelines recommend periodic endoscopic surveillance to detect and manage dysplasia. We aimed to explore patient knowledge and perceptions of CRC risk and colonoscopic surveillance.
Methods: A 44-item questionnaire was administered to IBD patients with colonic involvement attending gastroenterology clinics between July 2021 and April 2022.
Results: Of 418 respondents, 266 (64%) had ulcerative colitis and 145 (34%) had Crohn’s disease, with 176 (42%) diagnosed for ≥10 years. Two hundred and sixty-five (66%) patients rated their IBD control moderate/good (score ≥7/10), and 314 (75%) self-rated their understanding of IBD as good/excellent. Two hundred and ninety-eight patients (71%) recognised that CRC risk is higher in IBD but 83 (20%) felt the risk of CRC was lower in IBD or were unsure. Age (p=0.02), being a Crohn’s and Colitis UK (CCUK) member (p< 0.001), patient rated IBD control (p=0.04) and self-rated understanding (p=0.01) were associated with better CRC risk awareness. One hundred and forty-nine (36%) respondents stated that their IBD healthcare professional (HCP) had previously discussed CRC risk with them; this was associated with better CRC knowledge (p=0.001). On multivariate analysis CCUK membership (OR 2.75; 95% CI 1.57- 4.83; p< 0.001), prior HCP discussion (OR 1.57; 95% CI 0.85-2.87; p=0.01) and age ≥65 years (OR 0.3; 95% CI 0.09- 0.99; p=0.05) were predictive of greater CRC risk awareness. Concerning the most appropriate screening test for dysplasia, 369 patients (88%) stated colonoscopy, but only 29 (7%) were aware that colonic surveillance should commence 8-10 years after diagnosis; 153 (37%) recognised that optimal timing is when IBD is in remission. Patient reported information sources included gastroenterology HCPs (43%), patient support groups (28%), and patient leaflets (17%). The majority (78%) stated they would agree to have surveillance colonoscopy. Bowel preparation (50%) and discomfort (45%) were factors most likely to dissuade them from agreeing to surveillance.
Discussion: Patient knowledge of CRC risk and surveillance practice in IBD is variable. Modifiable factors associated with improved knowledge are discussion with HCPs and CCUK membership. Our findings underscore the need for better patient education to aid informed decision-making between patients and HCPs and improve adherence to colonoscopic surveillance.
Disclosures:
Eleanor K. Liu, MBChB, MRCP1, Aditi Erande, 2, John McLaughlin, BSc, MB ChB, PhD3, Jimmy K. Limdi, MBBS, FACG4. D0376 - Awareness and Perceptions of Colorectal Cancer Risk and Screening in Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Northern Care Alliance Trust, NHS, Manchester, England, United Kingdom; 2Metropolis Healthcare, Mumbai, Maharashtra, India; 3University of Manchester, Salford, England, United Kingdom; 4Northern Care Alliance NHS Trust & University of Manchester, Manchester, England, United Kingdom
Introduction: Patients with inflammatory bowel disease (IBD) are at higher risk of developing colorectal cancer (CRC). Guidelines recommend periodic endoscopic surveillance to detect and manage dysplasia. We aimed to explore patient knowledge and perceptions of CRC risk and colonoscopic surveillance.
Methods: A 44-item questionnaire was administered to IBD patients with colonic involvement attending gastroenterology clinics between July 2021 and April 2022.
Results: Of 418 respondents, 266 (64%) had ulcerative colitis and 145 (34%) had Crohn’s disease, with 176 (42%) diagnosed for ≥10 years. Two hundred and sixty-five (66%) patients rated their IBD control moderate/good (score ≥7/10), and 314 (75%) self-rated their understanding of IBD as good/excellent. Two hundred and ninety-eight patients (71%) recognised that CRC risk is higher in IBD but 83 (20%) felt the risk of CRC was lower in IBD or were unsure. Age (p=0.02), being a Crohn’s and Colitis UK (CCUK) member (p< 0.001), patient rated IBD control (p=0.04) and self-rated understanding (p=0.01) were associated with better CRC risk awareness. One hundred and forty-nine (36%) respondents stated that their IBD healthcare professional (HCP) had previously discussed CRC risk with them; this was associated with better CRC knowledge (p=0.001). On multivariate analysis CCUK membership (OR 2.75; 95% CI 1.57- 4.83; p< 0.001), prior HCP discussion (OR 1.57; 95% CI 0.85-2.87; p=0.01) and age ≥65 years (OR 0.3; 95% CI 0.09- 0.99; p=0.05) were predictive of greater CRC risk awareness. Concerning the most appropriate screening test for dysplasia, 369 patients (88%) stated colonoscopy, but only 29 (7%) were aware that colonic surveillance should commence 8-10 years after diagnosis; 153 (37%) recognised that optimal timing is when IBD is in remission. Patient reported information sources included gastroenterology HCPs (43%), patient support groups (28%), and patient leaflets (17%). The majority (78%) stated they would agree to have surveillance colonoscopy. Bowel preparation (50%) and discomfort (45%) were factors most likely to dissuade them from agreeing to surveillance.
Discussion: Patient knowledge of CRC risk and surveillance practice in IBD is variable. Modifiable factors associated with improved knowledge are discussion with HCPs and CCUK membership. Our findings underscore the need for better patient education to aid informed decision-making between patients and HCPs and improve adherence to colonoscopic surveillance.
Disclosures:
Eleanor Liu: Galapagos – Grant/Research Support, speaker fees. Janssen – speaker fee.
Aditi Erande indicated no relevant financial relationships.
John McLaughlin indicated no relevant financial relationships.
Jimmy Limdi: Abbvie – Advisory Committee/Board Member, Speakers Bureau. Arena – Advisory Committee/Board Member. Bristol Myers Squibb – Advisory Committee/Board Member. Ferring – Speakers Bureau. Galapagos – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Janssen – Advisory Committee/Board Member, Speakers Bureau. Pfizer – Advisor or Review Panel Member, Speakers Bureau. Takeda – Speakers Bureau.
Eleanor K. Liu, MBChB, MRCP1, Aditi Erande, 2, John McLaughlin, BSc, MB ChB, PhD3, Jimmy K. Limdi, MBBS, FACG4. D0376 - Awareness and Perceptions of Colorectal Cancer Risk and Screening in Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
