Back

Poster Session B - Monday Morning
Category: Endoscopy Video Forum
B0186 - Light at the End of the Tunnel: Pipeline to the Jejunum
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Judah Kupferman, MD
Icahn School of Medicine at Mount Sinai, NYC Health + Hospitals/Elmhurst
Elmhurst, NY
Presenting Author(s)
Award: Presidential Poster Award
Judah Kupferman, MD, Vennis Lourdusamy, MD, Anastasia Novikov, MD, Joshua Aron, MD, Aaron Walfish, MD, Raghav Bansal, MD, Joel Baum, MD, Ahmed Al-Khazraji, MD, Bhanu Singh, MD, Krishna Gurram, MD
Icahn School of Medicine at Mount Sinai, NYC Health + Hospitals/Elmhurst, Elmhurst, NY
Introduction: Small intestinal strictures that are distal to the duodenum, particularly the jejunum, are uniquely complicated to manage. Adult endoscopes are often too short or too rigid to reach this region of the small bowel. Furthermore, duodenal stents are not flexible enough and are uncovered. In this case, we were able to place several esophageal stents in the proximal jejunum using a pediatric colonoscope that could not be placed previously.
Case Description/Methods: A 56 year-old woman with hypertension, obstructive lung disease, and a prior ischemic stroke presented to the hospital for four days of postprandial emesis, abdominal distention, epigastric pain, and constipation. She previously underwent appendectomy and hysterectomy, and had no prior endoscopic studies. Computed tomography (CT) was performed demonstrating mural thickening of the distal duodenum and partial occlusion of the small bowel with regional lymphadenopathy, and a large left adrenal mass. Esophagogastroduodenoscopy (EGD) showed an intrinsic severe stenosis in the distal duodenum. After biopsies were taken, the tissue was found to be a primitive neuroectodermal tumor. Because of the presence of mesenteric adhesion and extensive stenosis, it was decided to correct the stricture endoscopically rather than with surgical intervention. Using a pediatric colonoscope and fluoroscopic guidance, three stents were placed sequentially and telescoping each other from the proximal jejunum to the distal duodenum: a fully covered 20 mm x 120 mm esophageal stent, a partially covered 18 mm x 97 mm esophageal stent, and a fully covered 20 mm x 60 mm esophageal stent (Figure 1). There were no immediate complications with the procedure and repeat imaging demonstrated luminal patency. Due to the expansion of the stents through a tight stricture, the abdominal pain and pressure was present despite no evidence of perforation on CT.
Discussion: This demonstrates the feasibility of utilizing multiple esophageal stents to help relieve more distal gastrointestinal obstructions that were not feasible in the past. The covered esophageal stents are extremely useful when there is discontinuity in the lumen of the small bowel to keep the natural flow of food and help prevent surgical interventions.

Disclosures:
Judah Kupferman, MD, Vennis Lourdusamy, MD, Anastasia Novikov, MD, Joshua Aron, MD, Aaron Walfish, MD, Raghav Bansal, MD, Joel Baum, MD, Ahmed Al-Khazraji, MD, Bhanu Singh, MD, Krishna Gurram, MD. B0186 - Light at the End of the Tunnel: Pipeline to the Jejunum, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Judah Kupferman, MD, Vennis Lourdusamy, MD, Anastasia Novikov, MD, Joshua Aron, MD, Aaron Walfish, MD, Raghav Bansal, MD, Joel Baum, MD, Ahmed Al-Khazraji, MD, Bhanu Singh, MD, Krishna Gurram, MD
Icahn School of Medicine at Mount Sinai, NYC Health + Hospitals/Elmhurst, Elmhurst, NY
Introduction: Small intestinal strictures that are distal to the duodenum, particularly the jejunum, are uniquely complicated to manage. Adult endoscopes are often too short or too rigid to reach this region of the small bowel. Furthermore, duodenal stents are not flexible enough and are uncovered. In this case, we were able to place several esophageal stents in the proximal jejunum using a pediatric colonoscope that could not be placed previously.
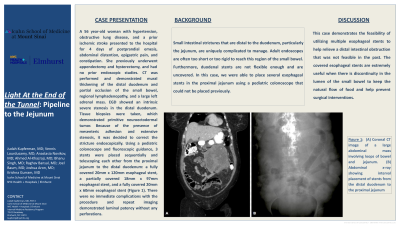
Case Description/Methods: A 56 year-old woman with hypertension, obstructive lung disease, and a prior ischemic stroke presented to the hospital for four days of postprandial emesis, abdominal distention, epigastric pain, and constipation. She previously underwent appendectomy and hysterectomy, and had no prior endoscopic studies. Computed tomography (CT) was performed demonstrating mural thickening of the distal duodenum and partial occlusion of the small bowel with regional lymphadenopathy, and a large left adrenal mass. Esophagogastroduodenoscopy (EGD) showed an intrinsic severe stenosis in the distal duodenum. After biopsies were taken, the tissue was found to be a primitive neuroectodermal tumor. Because of the presence of mesenteric adhesion and extensive stenosis, it was decided to correct the stricture endoscopically rather than with surgical intervention. Using a pediatric colonoscope and fluoroscopic guidance, three stents were placed sequentially and telescoping each other from the proximal jejunum to the distal duodenum: a fully covered 20 mm x 120 mm esophageal stent, a partially covered 18 mm x 97 mm esophageal stent, and a fully covered 20 mm x 60 mm esophageal stent (Figure 1). There were no immediate complications with the procedure and repeat imaging demonstrated luminal patency. Due to the expansion of the stents through a tight stricture, the abdominal pain and pressure was present despite no evidence of perforation on CT.
Discussion: This demonstrates the feasibility of utilizing multiple esophageal stents to help relieve more distal gastrointestinal obstructions that were not feasible in the past. The covered esophageal stents are extremely useful when there is discontinuity in the lumen of the small bowel to keep the natural flow of food and help prevent surgical interventions.

Figure: Figure 1: (A) Coronal CT image of a large abdominal mass involving loops of bowel and jejunum. (B) Abdominal x-ray showing interval placement of stents from the distal duodenum to the proximal jejunum
Disclosures:
Judah Kupferman indicated no relevant financial relationships.
Vennis Lourdusamy indicated no relevant financial relationships.
Anastasia Novikov indicated no relevant financial relationships.
Joshua Aron indicated no relevant financial relationships.
Aaron Walfish indicated no relevant financial relationships.
Raghav Bansal indicated no relevant financial relationships.
Joel Baum indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Bhanu Singh indicated no relevant financial relationships.
Krishna Gurram indicated no relevant financial relationships.
Judah Kupferman, MD, Vennis Lourdusamy, MD, Anastasia Novikov, MD, Joshua Aron, MD, Aaron Walfish, MD, Raghav Bansal, MD, Joel Baum, MD, Ahmed Al-Khazraji, MD, Bhanu Singh, MD, Krishna Gurram, MD. B0186 - Light at the End of the Tunnel: Pipeline to the Jejunum, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

