Back

Poster Session A - Sunday Afternoon
Category: Liver
A0544 - Malignancy Diagnosed via Ascites Analysis and EUS-Guided Portal Pressures
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Joseph Simmons, MD
Marshall University Joan C. Edwards School of Medicine
Huntington, WV
Presenting Author(s)
Joseph Simmons, MD, Wesam Frandah, MD, Tejas Joshi, MD
Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Ascites is the pathologic accumulation of fluid within the peritoneum and is classified by underlying etiology. Workup includes measurement of the serum ascites albumin gradient (SAAG) and ascitic protein levels with imaging modalities used as adjuvant tests. Although cirrhosis is the most common cause, other causes can include malignancy, infections, or congestive heart failure. We present a case of EUS-guided portal pressure measurements and liver biopsy being used to differentiate etiology of ascites when lab workup and imaging findings were incongruent.
Case Description/Methods: Patient is a 48-year-old female who presented with new-onset ascites. Abdominal ultrasound showed nodular contour of the liver with ascites suggestive of cirrhosis. Patient denied any alcohol use, drug use, or family history of liver disease. She underwent paracentesis and fluid analysis revealed a SAAG of 0.8, ascitic protein 4.3 gm/dL, and negative culture and cytology. Because of discordance between imaging findings and ascitic fluid analysis, she underwent EUS-guided portal pressure measurements and liver biopsy. EUS of the liver showed sharp borders and homogenous echotexture of the liver. EUS-guided portal pressure gradient was 0, indicating no evidence of portal hypertension and liver biopsy was inconsistent with cirrhosis. Further workup revealed elevated CA-125 and transvaginal ultrasound showed bilaterally complex cystic and solid adnexal masses. She underwent surgical resection and biopsy of a peritoneal wall mass which was consistent with mucin producing adenocarcinoma.
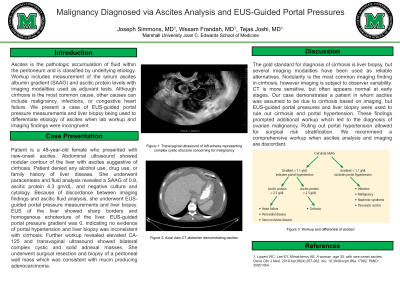
Discussion: The gold standard for diagnosis of cirrhosis is liver biopsy, but several imaging modalities have been used as reliable alternatives. Nodularity is the most common imaging finding in cirrhosis, however imaging is subject to observer variability. CT is more sensitive than ultrasound, but often appears normal at early stages. Our case demonstrates a patient in whom ascites was assumed to be due to cirrhosis based on imaging, but EUS-guided portal pressures and liver biopsy were used to rule out cirrhosis and portal hypertension. These findings prompted additional workup which led to the diagnosis of ovarian malignancy. Ruling out portal hypertension allowed for surgical risk stratification. We recommend a comprehensive workup when ascites analysis and imaging are discordant.
Disclosures:
Joseph Simmons, MD, Wesam Frandah, MD, Tejas Joshi, MD. A0544 - Malignancy Diagnosed via Ascites Analysis and EUS-Guided Portal Pressures, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Ascites is the pathologic accumulation of fluid within the peritoneum and is classified by underlying etiology. Workup includes measurement of the serum ascites albumin gradient (SAAG) and ascitic protein levels with imaging modalities used as adjuvant tests. Although cirrhosis is the most common cause, other causes can include malignancy, infections, or congestive heart failure. We present a case of EUS-guided portal pressure measurements and liver biopsy being used to differentiate etiology of ascites when lab workup and imaging findings were incongruent.
Case Description/Methods: Patient is a 48-year-old female who presented with new-onset ascites. Abdominal ultrasound showed nodular contour of the liver with ascites suggestive of cirrhosis. Patient denied any alcohol use, drug use, or family history of liver disease. She underwent paracentesis and fluid analysis revealed a SAAG of 0.8, ascitic protein 4.3 gm/dL, and negative culture and cytology. Because of discordance between imaging findings and ascitic fluid analysis, she underwent EUS-guided portal pressure measurements and liver biopsy. EUS of the liver showed sharp borders and homogenous echotexture of the liver. EUS-guided portal pressure gradient was 0, indicating no evidence of portal hypertension and liver biopsy was inconsistent with cirrhosis. Further workup revealed elevated CA-125 and transvaginal ultrasound showed bilaterally complex cystic and solid adnexal masses. She underwent surgical resection and biopsy of a peritoneal wall mass which was consistent with mucin producing adenocarcinoma.
Discussion: The gold standard for diagnosis of cirrhosis is liver biopsy, but several imaging modalities have been used as reliable alternatives. Nodularity is the most common imaging finding in cirrhosis, however imaging is subject to observer variability. CT is more sensitive than ultrasound, but often appears normal at early stages. Our case demonstrates a patient in whom ascites was assumed to be due to cirrhosis based on imaging, but EUS-guided portal pressures and liver biopsy were used to rule out cirrhosis and portal hypertension. These findings prompted additional workup which led to the diagnosis of ovarian malignancy. Ruling out portal hypertension allowed for surgical risk stratification. We recommend a comprehensive workup when ascites analysis and imaging are discordant.
Disclosures:
Joseph Simmons indicated no relevant financial relationships.
Wesam Frandah: Endo gastric solution – Consultant. Olympus – Consultant.
Tejas Joshi indicated no relevant financial relationships.
Joseph Simmons, MD, Wesam Frandah, MD, Tejas Joshi, MD. A0544 - Malignancy Diagnosed via Ascites Analysis and EUS-Guided Portal Pressures, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
