Back

Poster Session A - Sunday Afternoon
Category: Liver
A0553 - Palliative Care for Decompensated Cirrhosis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- AM
Austin Matney
University of Kentucky College of Medicine
Lexington, KY
Presenting Author(s)
Austin Matney, 1, Priya Abhyankar, MD1, Kshitij Thakur, MD2
1University of Kentucky College of Medicine, Lexington, KY; 2University of Kentucky, Lexington, KY
Introduction: The total mortality of liver diseases and cirrhosis surpassed 51,000 deaths in 2020. Decompensated cirrhosis is often a terminal illness for patients that do not receive a transplant. Palliative care involvement for decompensated cirrhosis patients improves symptom management and documentation of goals of care. We present a case where palliative care consultation addressed goals of care, poor prognostic understanding, and symptom management in a patient with NASH cirrhosis complicated by refractory ascites.
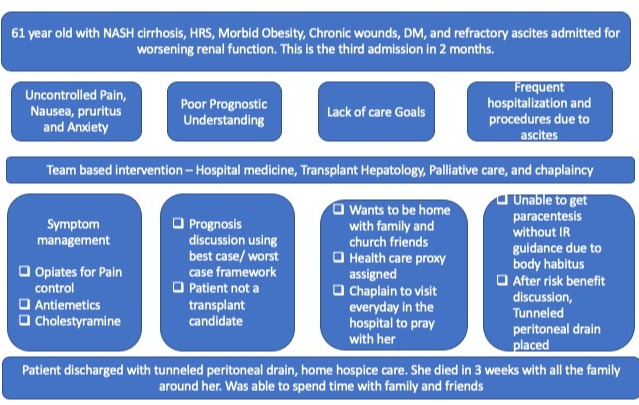
Case Description/Methods: A 61-year-old female with a history of NASH cirrhosis, morbid obesity, chronic wounds, and refractory ascites was admitted for worsening renal function due to suspected hepatorenal syndrome (HRS). She required frequent paracenteses with interventional radiology (IR) due to body habitus. This was her third admission in two months. Transplant hepatology deemed she was not a liver transplant candidate. Her renal function continued to worsen despite HRS treatment. She had no clear goals of care documented and a poor understanding of her prognosis. She was managed by a multidisciplinary team involving hospital medicine, transplant hepatology, nephrology, and palliative care. Palliative care assessed the patient’s unmet needs, including lack of care goals, poor prognostic understanding, and uncontrolled pain. Utilizing the best-case and worst-case framework, a family meeting was held to discuss patient prognosis. This revealed the patient’s desire to return home for her remaining days. Palliative care managed her uncontrolled symptoms and discussed the utility of dialysis. She declined dialysis. Prior to discharge to home hospice, IR placed a palliative tunneled long-term peritoneal drain. She died after spending three weeks at home with family.
Discussion: Palliative care consultation has a positive impact on symptom management and documentation of goals of care, yet it is commonly delayed and only used for end-of-life care in decompensated cirrhosis patients. Barriers to consultation include misperceptions about palliative care, difficulty estimating prognosis, and the allure of transplant. As in our case, these patients may experience frequent procedures, disrupting quality of life. Palliative tunneled long-term abdominal drains can be an effective alternative for drainage of ascites when used in the right setting and patient population, allowing for better symptom management with continuous drainage of small amounts of ascites.
Disclosures:
Austin Matney, 1, Priya Abhyankar, MD1, Kshitij Thakur, MD2. A0553 - Palliative Care for Decompensated Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kentucky College of Medicine, Lexington, KY; 2University of Kentucky, Lexington, KY
Introduction: The total mortality of liver diseases and cirrhosis surpassed 51,000 deaths in 2020. Decompensated cirrhosis is often a terminal illness for patients that do not receive a transplant. Palliative care involvement for decompensated cirrhosis patients improves symptom management and documentation of goals of care. We present a case where palliative care consultation addressed goals of care, poor prognostic understanding, and symptom management in a patient with NASH cirrhosis complicated by refractory ascites.
Case Description/Methods: A 61-year-old female with a history of NASH cirrhosis, morbid obesity, chronic wounds, and refractory ascites was admitted for worsening renal function due to suspected hepatorenal syndrome (HRS). She required frequent paracenteses with interventional radiology (IR) due to body habitus. This was her third admission in two months. Transplant hepatology deemed she was not a liver transplant candidate. Her renal function continued to worsen despite HRS treatment. She had no clear goals of care documented and a poor understanding of her prognosis. She was managed by a multidisciplinary team involving hospital medicine, transplant hepatology, nephrology, and palliative care. Palliative care assessed the patient’s unmet needs, including lack of care goals, poor prognostic understanding, and uncontrolled pain. Utilizing the best-case and worst-case framework, a family meeting was held to discuss patient prognosis. This revealed the patient’s desire to return home for her remaining days. Palliative care managed her uncontrolled symptoms and discussed the utility of dialysis. She declined dialysis. Prior to discharge to home hospice, IR placed a palliative tunneled long-term peritoneal drain. She died after spending three weeks at home with family.
Discussion: Palliative care consultation has a positive impact on symptom management and documentation of goals of care, yet it is commonly delayed and only used for end-of-life care in decompensated cirrhosis patients. Barriers to consultation include misperceptions about palliative care, difficulty estimating prognosis, and the allure of transplant. As in our case, these patients may experience frequent procedures, disrupting quality of life. Palliative tunneled long-term abdominal drains can be an effective alternative for drainage of ascites when used in the right setting and patient population, allowing for better symptom management with continuous drainage of small amounts of ascites.
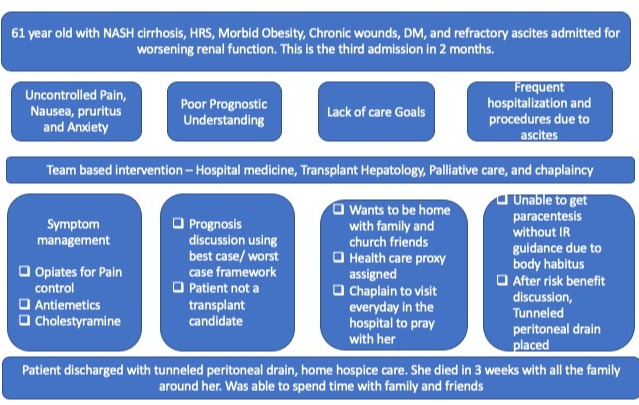
Figure: Hospital Course
Disclosures:
Austin Matney indicated no relevant financial relationships.
Priya Abhyankar indicated no relevant financial relationships.
Kshitij Thakur indicated no relevant financial relationships.
Austin Matney, 1, Priya Abhyankar, MD1, Kshitij Thakur, MD2. A0553 - Palliative Care for Decompensated Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
