Back
Poster Session A - Sunday Afternoon
A0699 - Gastric Volvulus in the Setting of Paraesophageal Hernia: Early Recognition of Severity and Timely Management Can Prevent Fatal Complications
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
.jpg)
Usama Sakhawat, MD
United Health Services Hospitals
Johnson City, NY
Presenting Author(s)
Usama Sakhawat, MD1, Khandokar A. Talib, MD2, Mohammad A. Abidi, MD3, M'hamed Turki, MD4, Fahad Malik, MD5, Nazif Chowdhury, MD2
1United Health Services Hospitals, Johnson City, NY; 2United Health Services Hospital, Johnson City, NY; 3United Health Services, Johnson City, NY; 4Marshall University, Johnson City, NY; 5United Health Services- Wilson Hospital, Binghamton, NY
Introduction: A paraesophageal hernia is made of a true hernial sac containing intra abdominal organs. When containing the stomach, gastric volvulus (GV) is one of the most feared complications. Failure to recognize the severity of clinical signs and symptoms on presentation can lead to ischemia, perforation and ultimately death. We are presenting a case where GV proved to be life-threatening.
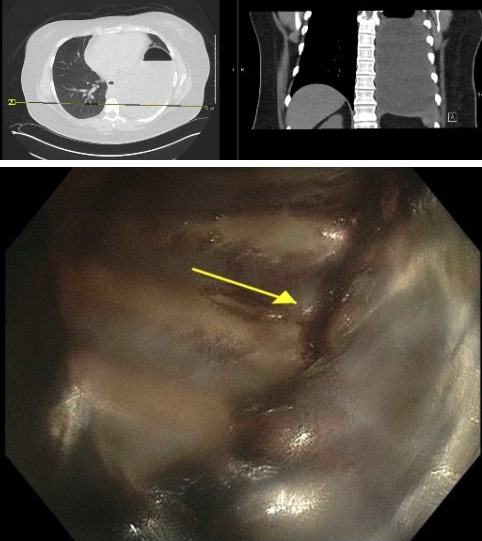
Case Description/Methods: A 37-year-old female with a past medical history of Nissen fundoplication (NF) and worsening gastroesophageal reflux disease came to the ED with the chief complaint of severe epigastric abdominal pain associated with retching, vomiting and obstipation. On admission, the patient was hypoxic and tachycardic. CT scan of the abdomen revealed a large paraesophageal hiatal hernia containing the stomach (Figure1). Considering the suspicion of a GV, the decision was made to endoscopically place a nasogastric tube to decompress the stomach. During the procedure, the thoracic cavity and rib cage was visualized (Figure 2). The procedure was aborted. Following this, the patient became agitated and then unresponsive. Intubation was performed for airway protection. Soon after, the patient went into cardiac arrest and Cardiopulmonary resuscitation (CPR) was initiated. During CPR, the patient was requiring higher pressure of ventilation and decreased breath sounds on auscultation; with suspicion of pneumothorax due to gastric perforation, bilateral chest tubes were placed. Return of spontaneous circulation was achieved after thoracic cavity decompression with chest tube placement. Emergent exploratory laparotomy revealed a 2 cm perforation at the level of the Nissen fundoplication with 80% of the stomach within the thoracic cavity. The defect was repaired and a jejunostomy was created. Unfortunately, the cardiac arrest was complicated with severe anoxic brain injury. After one month of hospital stay, the patient was eventually discharged with a chronic tracheostomy.
Discussion: Borchardt’s triad (acute epigastric pain, retching and failure to pass an NG tube) is highly diagnostic of GV. Gastric volvulus is a late but a rare complication of NF. The mechanism of GV development after NF is thought to be due to adhesions, foreign bodies, gastropexy and gastric herniation through a "transfundoplication" window. A high index of suspicion should be maintained for GV in patients presenting with signs/ symptoms of gastric obstruction. Early recognition of GV is important and surgical treatment should be expedited.
Disclosures:
Usama Sakhawat, MD1, Khandokar A. Talib, MD2, Mohammad A. Abidi, MD3, M'hamed Turki, MD4, Fahad Malik, MD5, Nazif Chowdhury, MD2. A0699 - Gastric Volvulus in the Setting of Paraesophageal Hernia: Early Recognition of Severity and Timely Management Can Prevent Fatal Complications, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1United Health Services Hospitals, Johnson City, NY; 2United Health Services Hospital, Johnson City, NY; 3United Health Services, Johnson City, NY; 4Marshall University, Johnson City, NY; 5United Health Services- Wilson Hospital, Binghamton, NY
Introduction: A paraesophageal hernia is made of a true hernial sac containing intra abdominal organs. When containing the stomach, gastric volvulus (GV) is one of the most feared complications. Failure to recognize the severity of clinical signs and symptoms on presentation can lead to ischemia, perforation and ultimately death. We are presenting a case where GV proved to be life-threatening.
Case Description/Methods: A 37-year-old female with a past medical history of Nissen fundoplication (NF) and worsening gastroesophageal reflux disease came to the ED with the chief complaint of severe epigastric abdominal pain associated with retching, vomiting and obstipation. On admission, the patient was hypoxic and tachycardic. CT scan of the abdomen revealed a large paraesophageal hiatal hernia containing the stomach (Figure1). Considering the suspicion of a GV, the decision was made to endoscopically place a nasogastric tube to decompress the stomach. During the procedure, the thoracic cavity and rib cage was visualized (Figure 2). The procedure was aborted. Following this, the patient became agitated and then unresponsive. Intubation was performed for airway protection. Soon after, the patient went into cardiac arrest and Cardiopulmonary resuscitation (CPR) was initiated. During CPR, the patient was requiring higher pressure of ventilation and decreased breath sounds on auscultation; with suspicion of pneumothorax due to gastric perforation, bilateral chest tubes were placed. Return of spontaneous circulation was achieved after thoracic cavity decompression with chest tube placement. Emergent exploratory laparotomy revealed a 2 cm perforation at the level of the Nissen fundoplication with 80% of the stomach within the thoracic cavity. The defect was repaired and a jejunostomy was created. Unfortunately, the cardiac arrest was complicated with severe anoxic brain injury. After one month of hospital stay, the patient was eventually discharged with a chronic tracheostomy.
Discussion: Borchardt’s triad (acute epigastric pain, retching and failure to pass an NG tube) is highly diagnostic of GV. Gastric volvulus is a late but a rare complication of NF. The mechanism of GV development after NF is thought to be due to adhesions, foreign bodies, gastropexy and gastric herniation through a "transfundoplication" window. A high index of suspicion should be maintained for GV in patients presenting with signs/ symptoms of gastric obstruction. Early recognition of GV is important and surgical treatment should be expedited.
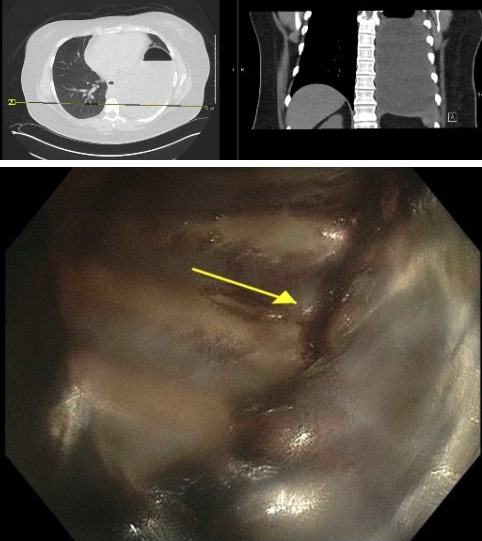
Figure: Figure 1- CT Scan of the abdomen revealed a large paraesophageal hernia containing the stomach.
Figure 2- Thoracic cavity and rib cage visualization on endoscopy.
Figure 2- Thoracic cavity and rib cage visualization on endoscopy.
Disclosures:
Usama Sakhawat indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Mohammad Abidi indicated no relevant financial relationships.
M'hamed Turki indicated no relevant financial relationships.
Fahad Malik indicated no relevant financial relationships.
Nazif Chowdhury indicated no relevant financial relationships.
Usama Sakhawat, MD1, Khandokar A. Talib, MD2, Mohammad A. Abidi, MD3, M'hamed Turki, MD4, Fahad Malik, MD5, Nazif Chowdhury, MD2. A0699 - Gastric Volvulus in the Setting of Paraesophageal Hernia: Early Recognition of Severity and Timely Management Can Prevent Fatal Complications, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
