Back
Poster Session C - Monday Afternoon
C0731 - An Elusive Diagnosis: Primary Gastric Melanoma With Metastatic Disease Presenting as Occult Gastrointestinal Bleed
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Syed Hamaad Rahman, DO
Methodist Dallas Medical Center
Dallas, TX
Presenting Author(s)
Syed Hamaad Rahman, DO1, Aimen Farooq, MD2, Nihal Ijaz Khan, MBBS3, Abu Hurairah, MD2
1Methodist Dallas Medical Center, Dallas, TX; 2AdventHealth Orlando, Orlando, FL; 3Allama Iqbal Medical College, Sarnia, ON, Canada
Introduction: Mucosal melanomas are rare, accounting for 0.3% of all cancer diagnoses and ~1% of all melanomas. While cutaneous melanomas frequently metastasize to the gastrointestinal (GI) tract, primary GI melanomas, especially gastric, are extremely rare. Mucosal melanomas are more aggressive and have worse prognosis compared to cutaneous melanomas. We report a case of primary gastric melanoma (PGM) presenting as occult blood loss anemia.
Case Description/Methods: A 58 year old male presented with complaints of weakness, fatigue, intermittent black and tarry stools, dizziness, and loss of appetite and weight over the past few months. He also noted enlarging masses in the upper right quadrant of his abdomen and right axillary area. He denied pertinent medical, surgical, and family history. He never had a colonoscopy or esophagogastroduodenoscopy (EGD). Physical exam was notable for a firm, non-tender subcutaneous right upper quadrant abdominal mass and a palpable, non-tender right axillary lymph node. Labs showed severe iron deficiency anemia for which he received 2 units of packed red blood cells.
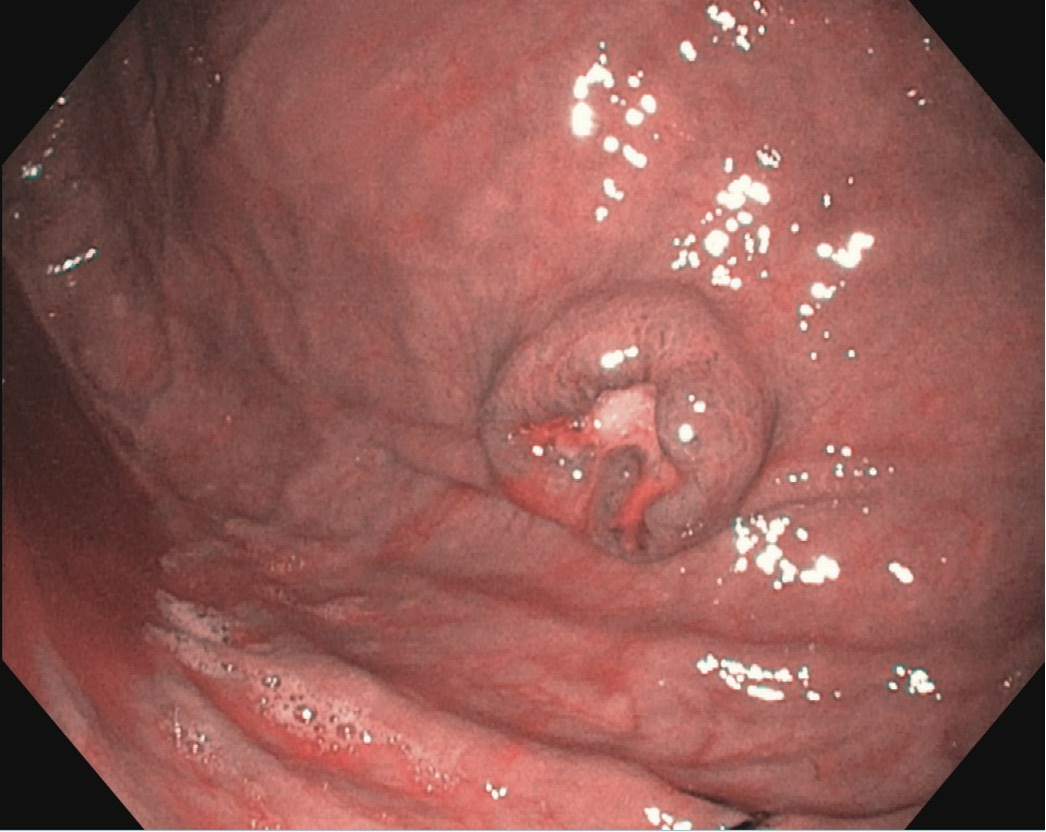
EGD showed a non-bleeding, clean base gastric ulcer with raised borders on the anterior wall of the gastric body. Histopathological analysis showed an aggregate of malignant tumor cells positive for S-100 protein, HMB-45, and Melan-A, consistent with malignant melanoma.
CT of the abdomen and pelvis revealed subcutaneous and intramuscular implants including a dominant lesion in the right upper abdominal wall, periportal and gastrohepatic ligament adenopathy, and small bowel thickening suspicious for carcinomatosis. Abdominal wall mass biopsy was consistent with metastatic melanoma, positive for S-100 protein and Melan-A. Detailed inspection failed to find any potential lesions on the skin, eyes or genitals. He was treated with combination immunotherapy.
Discussion: In addition to being extremely rare, PGMs are exceedingly challenging to diagnose. The lack of specific symptoms and distinct endoscopic findings make it an elusive diagnosis even for the most experienced endoscopists. Lesions sometimes appear pigmented on EGD, however, they are often amelanotic and undistinguishable from other gastric malignancies. Therefore, biopsy with immunohistochemistry analysis is a crucial part of the diagnostic process. Metastasis is the most important prognostic factor, making early detection imperative. Further research is needed to establish diagnostic and management guidelines for this uncommon yet deadly disease.
Disclosures:
Syed Hamaad Rahman, DO1, Aimen Farooq, MD2, Nihal Ijaz Khan, MBBS3, Abu Hurairah, MD2. C0731 - An Elusive Diagnosis: Primary Gastric Melanoma With Metastatic Disease Presenting as Occult Gastrointestinal Bleed, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Methodist Dallas Medical Center, Dallas, TX; 2AdventHealth Orlando, Orlando, FL; 3Allama Iqbal Medical College, Sarnia, ON, Canada
Introduction: Mucosal melanomas are rare, accounting for 0.3% of all cancer diagnoses and ~1% of all melanomas. While cutaneous melanomas frequently metastasize to the gastrointestinal (GI) tract, primary GI melanomas, especially gastric, are extremely rare. Mucosal melanomas are more aggressive and have worse prognosis compared to cutaneous melanomas. We report a case of primary gastric melanoma (PGM) presenting as occult blood loss anemia.
Case Description/Methods: A 58 year old male presented with complaints of weakness, fatigue, intermittent black and tarry stools, dizziness, and loss of appetite and weight over the past few months. He also noted enlarging masses in the upper right quadrant of his abdomen and right axillary area. He denied pertinent medical, surgical, and family history. He never had a colonoscopy or esophagogastroduodenoscopy (EGD). Physical exam was notable for a firm, non-tender subcutaneous right upper quadrant abdominal mass and a palpable, non-tender right axillary lymph node. Labs showed severe iron deficiency anemia for which he received 2 units of packed red blood cells.
EGD showed a non-bleeding, clean base gastric ulcer with raised borders on the anterior wall of the gastric body. Histopathological analysis showed an aggregate of malignant tumor cells positive for S-100 protein, HMB-45, and Melan-A, consistent with malignant melanoma.
CT of the abdomen and pelvis revealed subcutaneous and intramuscular implants including a dominant lesion in the right upper abdominal wall, periportal and gastrohepatic ligament adenopathy, and small bowel thickening suspicious for carcinomatosis. Abdominal wall mass biopsy was consistent with metastatic melanoma, positive for S-100 protein and Melan-A. Detailed inspection failed to find any potential lesions on the skin, eyes or genitals. He was treated with combination immunotherapy.
Discussion: In addition to being extremely rare, PGMs are exceedingly challenging to diagnose. The lack of specific symptoms and distinct endoscopic findings make it an elusive diagnosis even for the most experienced endoscopists. Lesions sometimes appear pigmented on EGD, however, they are often amelanotic and undistinguishable from other gastric malignancies. Therefore, biopsy with immunohistochemistry analysis is a crucial part of the diagnostic process. Metastasis is the most important prognostic factor, making early detection imperative. Further research is needed to establish diagnostic and management guidelines for this uncommon yet deadly disease.
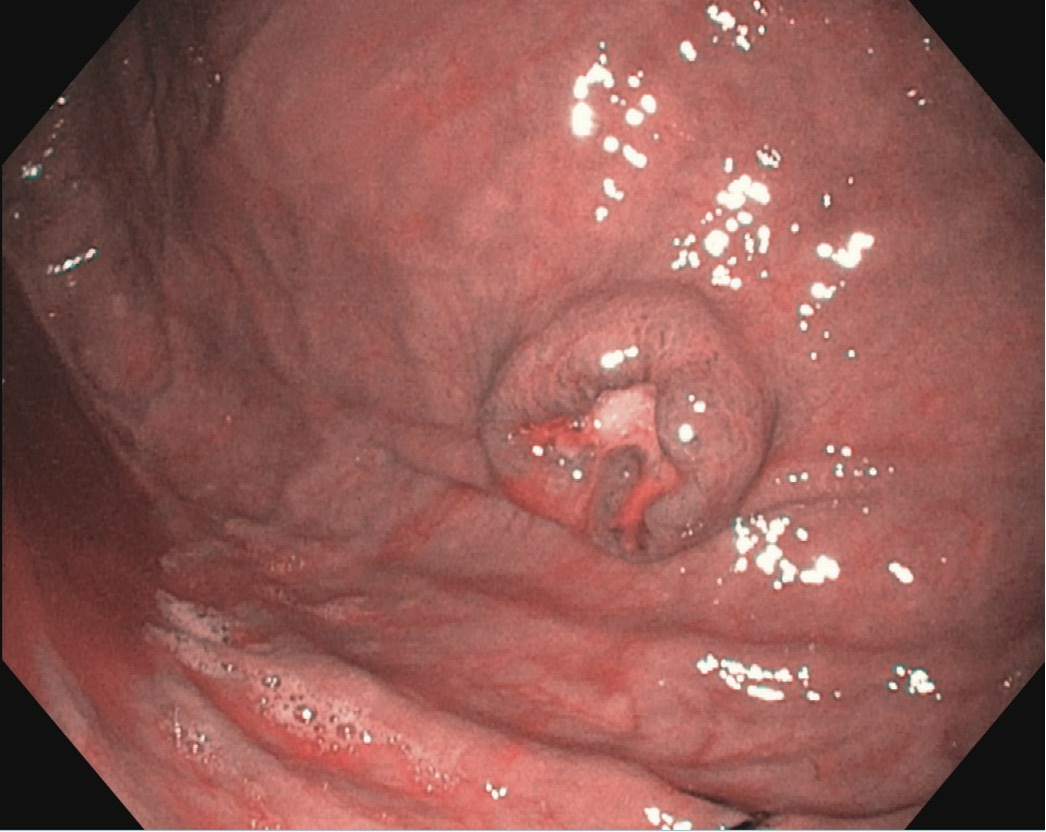
Figure: Non-bleeding ulcer with a clean base on the anterior wall of the gastric body (8 mm, Forrest Class III)
Disclosures:
Syed Hamaad Rahman indicated no relevant financial relationships.
Aimen Farooq indicated no relevant financial relationships.
Nihal Ijaz Khan indicated no relevant financial relationships.
Abu Hurairah indicated no relevant financial relationships.
Syed Hamaad Rahman, DO1, Aimen Farooq, MD2, Nihal Ijaz Khan, MBBS3, Abu Hurairah, MD2. C0731 - An Elusive Diagnosis: Primary Gastric Melanoma With Metastatic Disease Presenting as Occult Gastrointestinal Bleed, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
