Back
Poster Session E - Tuesday Afternoon
E0653 - Imaging-Negative Double Jejunal Intussusception Diagnosed on Laparoscopy With Intraoperative Enteroscopy in a Patient With Peutz-Jeghers Syndrome
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Ella Cohen, BS
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Ella Cohen, BS, Yuying Luo, MD, L. Brian Katz, MD, Alexandros Polydorides, MD, PhD, Nikhil A. Kumta, MD, MS, Bruce E. Sands, MD, MS, FACG, Aimee L. Lucas, MD, MS, FACG
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Peutz-Jeghers syndrome (PJS) is a rare, autosomal dominant syndrome characterized by gastrointestinal polyposis, mucocutaneous pigmentation, and an increased risk of malignancy. Although generally benign, PJ-type polyps can be large and can act as lead points for intussusception. We describe the case of a 25-year-old female with PJS who presented with recurrent abdominal pain in the setting of negative cross-sectional imaging who was found to have a double intussusception on diagnostic laparoscopy with intraoperative enteroscopy.
Case Description/Methods: The patient’s surgical history was notable for five reductions of small bowel intussusception related to PJ-type polyps since age 9.
She initially presented with intermittent abdominal pain six months prior to this admission, at which time seventeen small bowel PJ-type polyps were resected via anterograde small bowel enteroscopy. Her pain persisted despite intervention, and magnetic resonance cholangiopancreatography (MRCP) and magnetic resonance enterography (MRE) four months prior to admission demonstrated two additional polyps in the terminal ileum which were resected via colonoscopy.
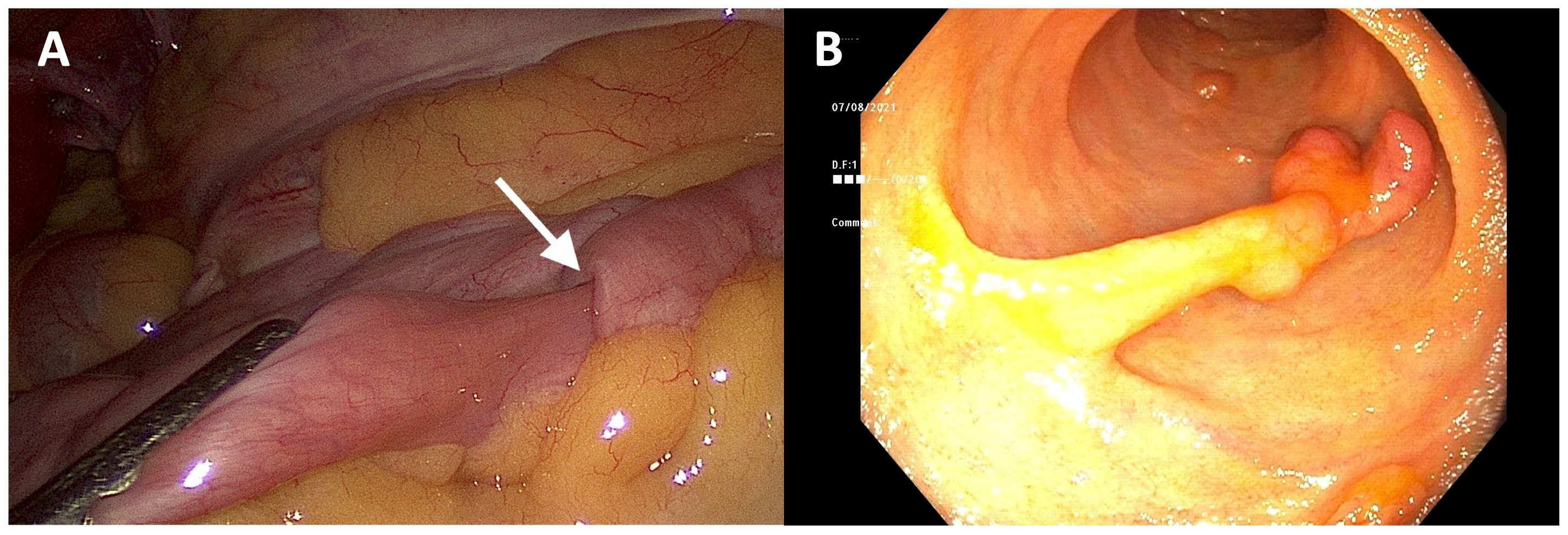
The patient then presented with acutely worsening abdominal pain that she described as similar to her past episodes of intussusception. Although a computed tomography (CT) scan with IV contrast was unremarkable, there was high clinical suspicion for intussusception, so a multidisciplinary decision was made to proceed with diagnostic laparoscopy. Two jejunal intussusceptions related to large polyps were identified and reduced, and one large (25mm) polyp was surgically resected (Figure 1A & 1B). On intraoperative enteroscopy via enterotomy, one smaller (15mm) duodenal polyp and three large (20-25mm) jejunal polyps were removed. The patient was discharged three days postoperatively with resolution of her pain.
Discussion: Patients with PJS require multidisciplinary care given their significantly increased risk of both gastrointestinal and extraintestinal malignancy and complications such as intussusception. While CT is generally the preferred imaging study when evaluating for intussusception in adults, there is limited data on its sensitivity, with estimates ranging from 58-100%. Our case highlights two important points: first, although PJ-type polyps are generally benign, they may grow rapidly; and second, even if imaging is unremarkable, clinicians should still consider intussusception in patients with predisposing risk factors and a compatible clinical picture.
Disclosures:
Ella Cohen, BS, Yuying Luo, MD, L. Brian Katz, MD, Alexandros Polydorides, MD, PhD, Nikhil A. Kumta, MD, MS, Bruce E. Sands, MD, MS, FACG, Aimee L. Lucas, MD, MS, FACG. E0653 - Imaging-Negative Double Jejunal Intussusception Diagnosed on Laparoscopy With Intraoperative Enteroscopy in a Patient With Peutz-Jeghers Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Peutz-Jeghers syndrome (PJS) is a rare, autosomal dominant syndrome characterized by gastrointestinal polyposis, mucocutaneous pigmentation, and an increased risk of malignancy. Although generally benign, PJ-type polyps can be large and can act as lead points for intussusception. We describe the case of a 25-year-old female with PJS who presented with recurrent abdominal pain in the setting of negative cross-sectional imaging who was found to have a double intussusception on diagnostic laparoscopy with intraoperative enteroscopy.
Case Description/Methods: The patient’s surgical history was notable for five reductions of small bowel intussusception related to PJ-type polyps since age 9.
She initially presented with intermittent abdominal pain six months prior to this admission, at which time seventeen small bowel PJ-type polyps were resected via anterograde small bowel enteroscopy. Her pain persisted despite intervention, and magnetic resonance cholangiopancreatography (MRCP) and magnetic resonance enterography (MRE) four months prior to admission demonstrated two additional polyps in the terminal ileum which were resected via colonoscopy.
The patient then presented with acutely worsening abdominal pain that she described as similar to her past episodes of intussusception. Although a computed tomography (CT) scan with IV contrast was unremarkable, there was high clinical suspicion for intussusception, so a multidisciplinary decision was made to proceed with diagnostic laparoscopy. Two jejunal intussusceptions related to large polyps were identified and reduced, and one large (25mm) polyp was surgically resected (Figure 1A & 1B). On intraoperative enteroscopy via enterotomy, one smaller (15mm) duodenal polyp and three large (20-25mm) jejunal polyps were removed. The patient was discharged three days postoperatively with resolution of her pain.
Discussion: Patients with PJS require multidisciplinary care given their significantly increased risk of both gastrointestinal and extraintestinal malignancy and complications such as intussusception. While CT is generally the preferred imaging study when evaluating for intussusception in adults, there is limited data on its sensitivity, with estimates ranging from 58-100%. Our case highlights two important points: first, although PJ-type polyps are generally benign, they may grow rapidly; and second, even if imaging is unremarkable, clinicians should still consider intussusception in patients with predisposing risk factors and a compatible clinical picture.
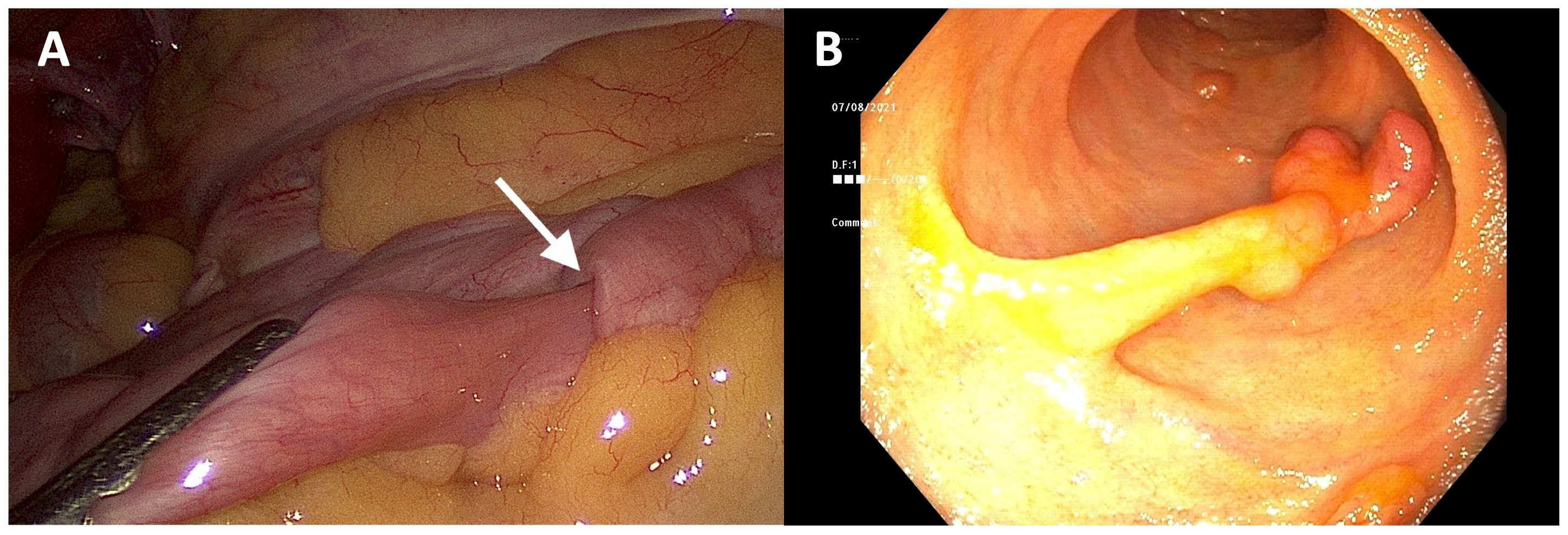
Figure: Figure 1: (A) Laparoscopic view of a small bowel intussusception (arrow) related to a Peutz-Jeghers-type polyp. (B) Endoscopic view of a large hamartomatous Peutz-Jeghers-type polyp.
Disclosures:
Ella Cohen indicated no relevant financial relationships.
Yuying Luo indicated no relevant financial relationships.
L. Brian Katz indicated no relevant financial relationships.
Alexandros Polydorides indicated no relevant financial relationships.
Nikhil Kumta indicated no relevant financial relationships.
Bruce Sands: Abivax – Consultant, Speaking. Amgen – Consultant. Arena Pharmaceuticals – Consultant. Artugen Therapeutics – Consultant. AstraZeneca – Consultant. Bacainn Therapeutics – Consultant. Boehringer-Ingelheim – Consultant. Boston Pharmaceuticals – Consultant. Bristol Myers Squibb – Consultant, speaking, research funding. Calibr – Consultant. Celltrion Healthcare – Consultant. ClostraBio – Consultant. Eli Lilly and Company – Consultant. Entera – Consultant. Evommune – Consultant. Galapagos – Consultant. Genentech – Consultant. Gilead Sciences – Consultant. GlaxoSmithKline – Consultant. Gossamer Bio – Consultant. InDex Pharmaceuticals – Consultant. Innovation Therapeutics – Consultant. Inotrem – Consultant. Ironwood Pharmaceuticals – Consultant. Janssen – Consultant, Grant/Research Support, speaking. Kaleido – Consultant. Kallyope – Consultant. Miro Bio – Consultant. Morphic Therapeutics – Consultant. MRM Health – Consultant. Pfizer – Consultant, speaking. Progenity – Consultant. Prometheus Biosciences – Consultant. Protagonist Therapeutics – Consultant. Q32 Bio – Consultant. Surrozen – Consultant. Takeda – Consultant, Speaking. Teva – Consultant. TLL Pharmaceutical – Consultant. USWM Enterprises – Consultant. VielaBio – Consultant.
Aimee Lucas indicated no relevant financial relationships.
Ella Cohen, BS, Yuying Luo, MD, L. Brian Katz, MD, Alexandros Polydorides, MD, PhD, Nikhil A. Kumta, MD, MS, Bruce E. Sands, MD, MS, FACG, Aimee L. Lucas, MD, MS, FACG. E0653 - Imaging-Negative Double Jejunal Intussusception Diagnosed on Laparoscopy With Intraoperative Enteroscopy in a Patient With Peutz-Jeghers Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
