Back
Poster Session E - Tuesday Afternoon
E0674 - A Rare Case of Large Brunner Gland Hyperplasia
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Justin J. Wagner, DO
Coney Island Hospital
Brooklyn, NY
Presenting Author(s)
Justin J. Wagner, DO, Joshua Diaz, MD, Neera Sinha, MD, John Trillo, MD
Coney Island Hospital, Brooklyn, NY
Introduction: Brunner’s gland hyperplasia (BGH) is a rare, typically benign lesion of the small intestine, averaging 1-2 cm in size, and is usually diagnosed in the fifth or sixth decade of life with equal sexual predilection. It typically presents asymptomatically and is diagnosed incidentally during upper endoscopy, but can sometimes present in the setting of acute gastrointestinal hemorrhage, chronic anemia, or intestinal obstruction.
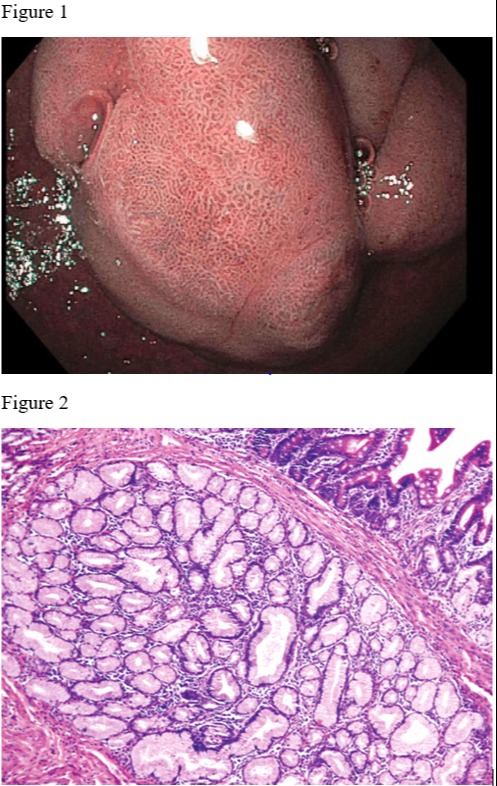
Case Description/Methods: We present a case of BGH that was measured to be 5 cm and diagnosed incidentally during upper endoscopy in the setting of investigating for causes of iron deficiency anemia (IDA) in a 67-year-old- male patient who also had a concomitant Helicobacter pylorus (H. pylori) infection.
Discussion: BGH is caused by hyperplasia of the exocrine glands within the duodenum but its etiology still remains unknown. Brunner’s glands are tubular mucus glands in the mucosa and submucosa of the duodenum that secrete mucus, which alkalinizes chyme from the stomach. Since Brunner’s glands serve the purpose of increasing pH, it is postulated that increased acid secretion could cause these glands to undergo a state of hyperplasia. Other studies have suggested that H. pylori could possibly play an etiological role since most BGH cases are associated with concomitant H. pylori infection.
BGH is typically diagnosed in asymptomatic patients and discovered incidentally on upper endoscopy, but clinical manifestations can consist of gastrointestinal bleeding, IDA, or duodenal obstruction. Diagnosis is made via endoscopic biopsy and histopathological analysis will reveal a lack of encapsulation and dysplasia.
Management guidelines are nonexistent and although BGH is typically a benign lesion, few case reports have identified malignant transformation, which should elicit caution in presuming all lesions to be invariably benign. BGH lesions larger than 2 cm can cause more complications than smaller sizes and removal is recommended regardless if the patient is asymptomatic. Endoscopic polypectomy is typically the first-line treatment with surgical excision reserved for only massive lesions or polypectomy failure.
This case highlights an example of a very large 5 cm, benign, pedunculated BGH lesion incidentally found within the duodenal bulb of a male patient, who presented for the purpose of being worked-up for IDA, and was also found to have a concomitant H. pylori infection, thereby further validating the purported hypothesis of H. pylori as an etiological factor in BGH.
Disclosures:
Justin J. Wagner, DO, Joshua Diaz, MD, Neera Sinha, MD, John Trillo, MD. E0674 - A Rare Case of Large Brunner Gland Hyperplasia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Coney Island Hospital, Brooklyn, NY
Introduction: Brunner’s gland hyperplasia (BGH) is a rare, typically benign lesion of the small intestine, averaging 1-2 cm in size, and is usually diagnosed in the fifth or sixth decade of life with equal sexual predilection. It typically presents asymptomatically and is diagnosed incidentally during upper endoscopy, but can sometimes present in the setting of acute gastrointestinal hemorrhage, chronic anemia, or intestinal obstruction.
Case Description/Methods: We present a case of BGH that was measured to be 5 cm and diagnosed incidentally during upper endoscopy in the setting of investigating for causes of iron deficiency anemia (IDA) in a 67-year-old- male patient who also had a concomitant Helicobacter pylorus (H. pylori) infection.
Discussion: BGH is caused by hyperplasia of the exocrine glands within the duodenum but its etiology still remains unknown. Brunner’s glands are tubular mucus glands in the mucosa and submucosa of the duodenum that secrete mucus, which alkalinizes chyme from the stomach. Since Brunner’s glands serve the purpose of increasing pH, it is postulated that increased acid secretion could cause these glands to undergo a state of hyperplasia. Other studies have suggested that H. pylori could possibly play an etiological role since most BGH cases are associated with concomitant H. pylori infection.
BGH is typically diagnosed in asymptomatic patients and discovered incidentally on upper endoscopy, but clinical manifestations can consist of gastrointestinal bleeding, IDA, or duodenal obstruction. Diagnosis is made via endoscopic biopsy and histopathological analysis will reveal a lack of encapsulation and dysplasia.
Management guidelines are nonexistent and although BGH is typically a benign lesion, few case reports have identified malignant transformation, which should elicit caution in presuming all lesions to be invariably benign. BGH lesions larger than 2 cm can cause more complications than smaller sizes and removal is recommended regardless if the patient is asymptomatic. Endoscopic polypectomy is typically the first-line treatment with surgical excision reserved for only massive lesions or polypectomy failure.
This case highlights an example of a very large 5 cm, benign, pedunculated BGH lesion incidentally found within the duodenal bulb of a male patient, who presented for the purpose of being worked-up for IDA, and was also found to have a concomitant H. pylori infection, thereby further validating the purported hypothesis of H. pylori as an etiological factor in BGH.
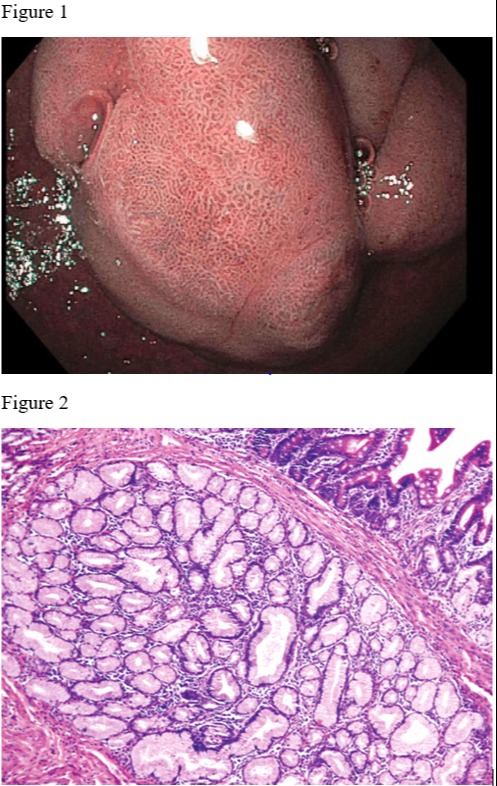
Figure: Figure 1: 5 cm polyp found within the duodenal bulb with biopsy results that revealed Brunner gland hyperplasia.
Figure 2: Example of photomicroscope of Brunner's gland hyperplasia showing hyperplastic lobules of Brunner's glands. Reference: Nandini D. Patel, Angela D. Levy, Anupamjit K. Mehrotra, and Leslie H. Sobin. American Journal of Roentgenology 2006 187:3, 715-722.
Figure 2: Example of photomicroscope of Brunner's gland hyperplasia showing hyperplastic lobules of Brunner's glands. Reference: Nandini D. Patel, Angela D. Levy, Anupamjit K. Mehrotra, and Leslie H. Sobin. American Journal of Roentgenology 2006 187:3, 715-722.
Disclosures:
Justin Wagner indicated no relevant financial relationships.
Joshua Diaz indicated no relevant financial relationships.
Neera Sinha indicated no relevant financial relationships.
John Trillo indicated no relevant financial relationships.
Justin J. Wagner, DO, Joshua Diaz, MD, Neera Sinha, MD, John Trillo, MD. E0674 - A Rare Case of Large Brunner Gland Hyperplasia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
