Back
Poster Session E - Tuesday Afternoon
E0656 - A Red Herring? Duodenal Vasculitis in the Setting of Post-COVID-19 Infection
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Deepa Kumarjiguda, DO
Geisinger Health System
Danville, PA
Presenting Author(s)
Deepa Kumarjiguda, DO1, Nicholas Talabiska, DO2, Ayusa Sinha, MD3, Nihit Shah, MD1, Amitpal S. Johal, MD4
1Geisinger Health System, Danville, PA; 2Geisinger Medical Center, Philadelphia, PA; 3Geisinger Medical Center, Danville, PA; 4Geisinger, Danville, PA
Introduction: While the respiratory symptoms of coronavirus disease 2019 [COVID-19]) are well-defined, the gastrointestinal implications continue to be explored with increased experience. Herein we describe a unique case illustrating duodenal and cutaneous leukocytoclastic vasculitis (LCV) as a manifestation of COVID-19.
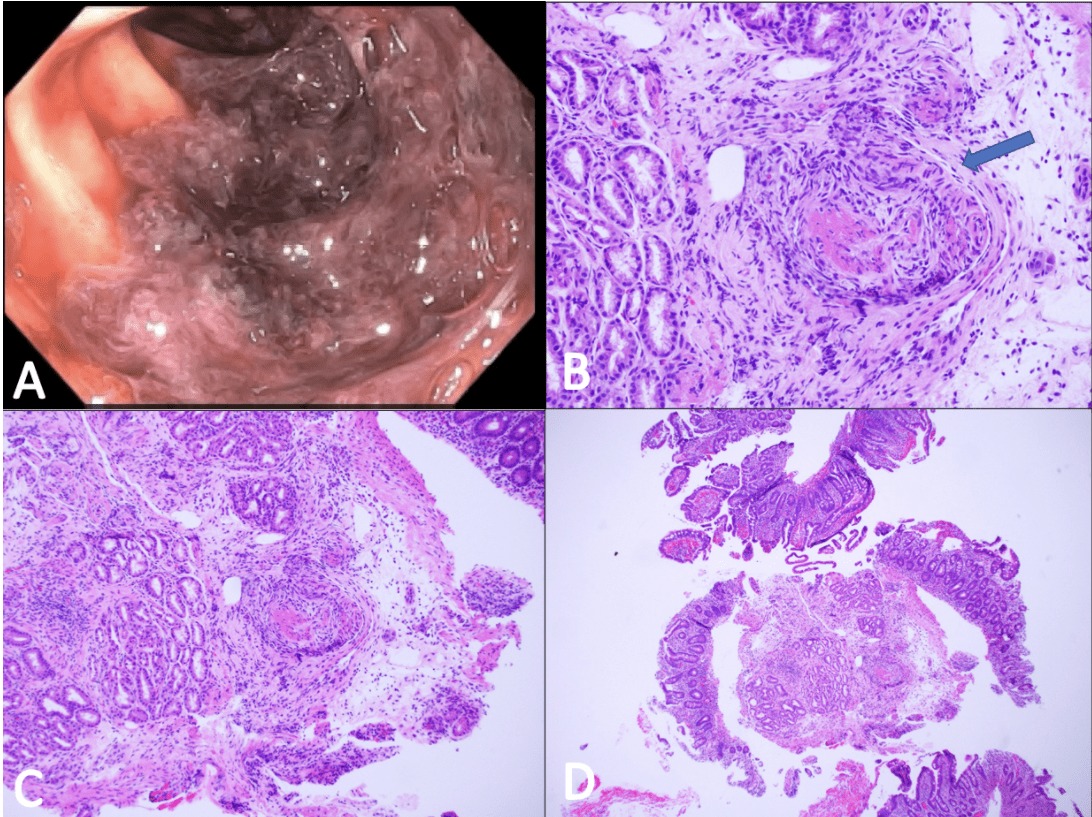
Case Description/Methods: A 55-year-old female with a medical history significant for triple-negative left breast cancer status post mastectomy presented with a two-day history of intermittent epigastric pain associated with nausea and acute anemia. One week prior, the patient was admitted for a GI bleed, initially suspected to be NSAID - induced due to COVID-19 infection. Symptoms resolved without endoscopic intervention and outpatient follow up was arranged. Exam was significant for epigastric tenderness and bilateral lower extremities with a non-tender, non-pruritic maculopapular rash. Labs revealed leukopenia, negative ANA and C-ANCA, low C4 (< 2), and elevated CRP (25). CT imaging demonstrated small bowel thickening, suggestive of enteritis. Endoscopy revealed mucosal changes involving the duodenum and jejunum with fibrinoid-like necrosis and mild inflammatory cell infiltrates, consistent with vasculitis-like changes (Fig. 1A). Dermatological biopsy revealed negative immunofluorescence studies (IgA, IgG, IgM, and C3) in the basement membrane and perivascular regions consistent with LCV, excluding IgA vasculitis (Fig. 1B-D). Cryoglobulin level was not diagnostic for cryoglobulinemia. Angiography studies of her chest, abdomen, and pelvis excluded large- or medium-vessel vasculitis. We suspected symptoms may be due to COVID-19-induced cutaneous and duodenal LCV. Treatment comprised of an oral steroid taper and PPI therapy with a plan for repeat outpatient endoscopy.
Discussion: This presentation of duodenal vasculitis is a suspected consequence of her recent COVID-19 infection. Literature demonstrates postmortem analysis of direct viral mononuclear cell infiltration in the vascular intima and lumen of vessels causing complications such as coagulopathy and vasculitis. COVID-19 may be a possible trigger for an immune complex hypersensitivity reaction. Literature also supports COVID-19 vasculitis with some cases associated with vaccination. The gastrointestinal effects of COVID-19 continue to be explored. COVID-19 vasculitis should be considered on the differential in presentation of abdominal pain, melena and dermatological findings in the setting of recent COVID-19 diagnosis.
Disclosures:
Deepa Kumarjiguda, DO1, Nicholas Talabiska, DO2, Ayusa Sinha, MD3, Nihit Shah, MD1, Amitpal S. Johal, MD4. E0656 - A Red Herring? Duodenal Vasculitis in the Setting of Post-COVID-19 Infection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Geisinger Health System, Danville, PA; 2Geisinger Medical Center, Philadelphia, PA; 3Geisinger Medical Center, Danville, PA; 4Geisinger, Danville, PA
Introduction: While the respiratory symptoms of coronavirus disease 2019 [COVID-19]) are well-defined, the gastrointestinal implications continue to be explored with increased experience. Herein we describe a unique case illustrating duodenal and cutaneous leukocytoclastic vasculitis (LCV) as a manifestation of COVID-19.
Case Description/Methods: A 55-year-old female with a medical history significant for triple-negative left breast cancer status post mastectomy presented with a two-day history of intermittent epigastric pain associated with nausea and acute anemia. One week prior, the patient was admitted for a GI bleed, initially suspected to be NSAID - induced due to COVID-19 infection. Symptoms resolved without endoscopic intervention and outpatient follow up was arranged. Exam was significant for epigastric tenderness and bilateral lower extremities with a non-tender, non-pruritic maculopapular rash. Labs revealed leukopenia, negative ANA and C-ANCA, low C4 (< 2), and elevated CRP (25). CT imaging demonstrated small bowel thickening, suggestive of enteritis. Endoscopy revealed mucosal changes involving the duodenum and jejunum with fibrinoid-like necrosis and mild inflammatory cell infiltrates, consistent with vasculitis-like changes (Fig. 1A). Dermatological biopsy revealed negative immunofluorescence studies (IgA, IgG, IgM, and C3) in the basement membrane and perivascular regions consistent with LCV, excluding IgA vasculitis (Fig. 1B-D). Cryoglobulin level was not diagnostic for cryoglobulinemia. Angiography studies of her chest, abdomen, and pelvis excluded large- or medium-vessel vasculitis. We suspected symptoms may be due to COVID-19-induced cutaneous and duodenal LCV. Treatment comprised of an oral steroid taper and PPI therapy with a plan for repeat outpatient endoscopy.
Discussion: This presentation of duodenal vasculitis is a suspected consequence of her recent COVID-19 infection. Literature demonstrates postmortem analysis of direct viral mononuclear cell infiltration in the vascular intima and lumen of vessels causing complications such as coagulopathy and vasculitis. COVID-19 may be a possible trigger for an immune complex hypersensitivity reaction. Literature also supports COVID-19 vasculitis with some cases associated with vaccination. The gastrointestinal effects of COVID-19 continue to be explored. COVID-19 vasculitis should be considered on the differential in presentation of abdominal pain, melena and dermatological findings in the setting of recent COVID-19 diagnosis.
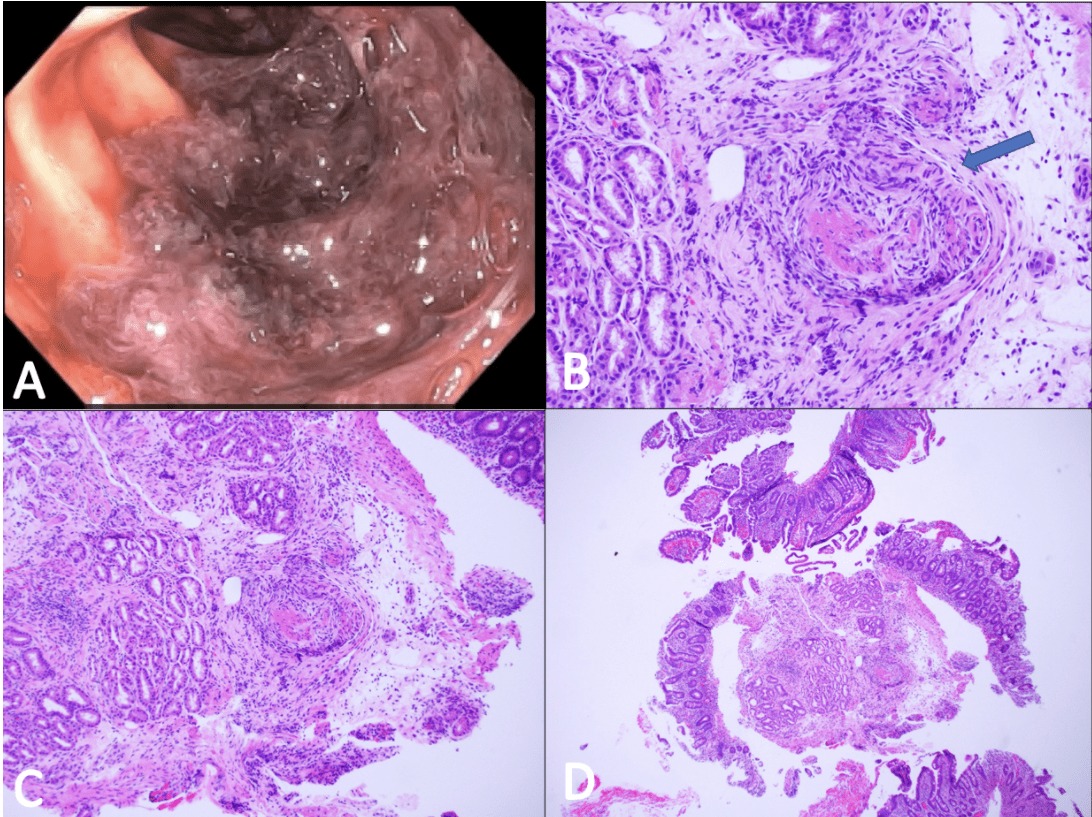
Figure: A. Endoscopic images of the second part of duodenum suggestive of vasculitis.
B. Active duodenitis with hemorrhage and focal changes in blood vessels (blue arrow). There are blood vessels in the submucosa showing fibrinoid like necrosis and mild inflammatory cells infiltrates.
C. There is active and chronic duodenitis with hemorrhage.
D. Further inflammatory cells and fibrinoid like necrosis around blood vessels.
B. Active duodenitis with hemorrhage and focal changes in blood vessels (blue arrow). There are blood vessels in the submucosa showing fibrinoid like necrosis and mild inflammatory cells infiltrates.
C. There is active and chronic duodenitis with hemorrhage.
D. Further inflammatory cells and fibrinoid like necrosis around blood vessels.
Disclosures:
Deepa Kumarjiguda indicated no relevant financial relationships.
Nicholas Talabiska indicated no relevant financial relationships.
Ayusa Sinha indicated no relevant financial relationships.
Nihit Shah indicated no relevant financial relationships.
Amitpal Johal indicated no relevant financial relationships.
Deepa Kumarjiguda, DO1, Nicholas Talabiska, DO2, Ayusa Sinha, MD3, Nihit Shah, MD1, Amitpal S. Johal, MD4. E0656 - A Red Herring? Duodenal Vasculitis in the Setting of Post-COVID-19 Infection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
