Back
Poster Session D - Tuesday Morning
D0676 - An Unusual Case of Diarrhea in a Patient With Lupus
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom

Mohammed Rifat Shaik, MBBS
University of Maryland Medical Center Midtown Campus
Baltimore, MD
Presenting Author(s)
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Erika Wheeler, MD3, Yuting Huang, MD, PhD1, Robert T. Chow, MD, MBA1, Jamal A. Mikdashi, MD3
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2Guntur Medical College, Guntur, Andhra Pradesh, India; 3University of Maryland Medical Center, Baltimore, MD
Introduction: The differential diagnosis of diarrhea in the setting of systemic lupus erythematosus (SLE) is broad and includes lupus-related as well as non-lupus-related etiologies. Lupus-related etiologies include but are not limited to mesenteric vasculitis, pseudo-obstruction, protein-losing enteropathy, and pancreatitis. Autoimmune enteropathy (AIE) is rare in adults, with fewer than fifty cases described in the medical literature. We report a case that responded effectively to Belimumab.
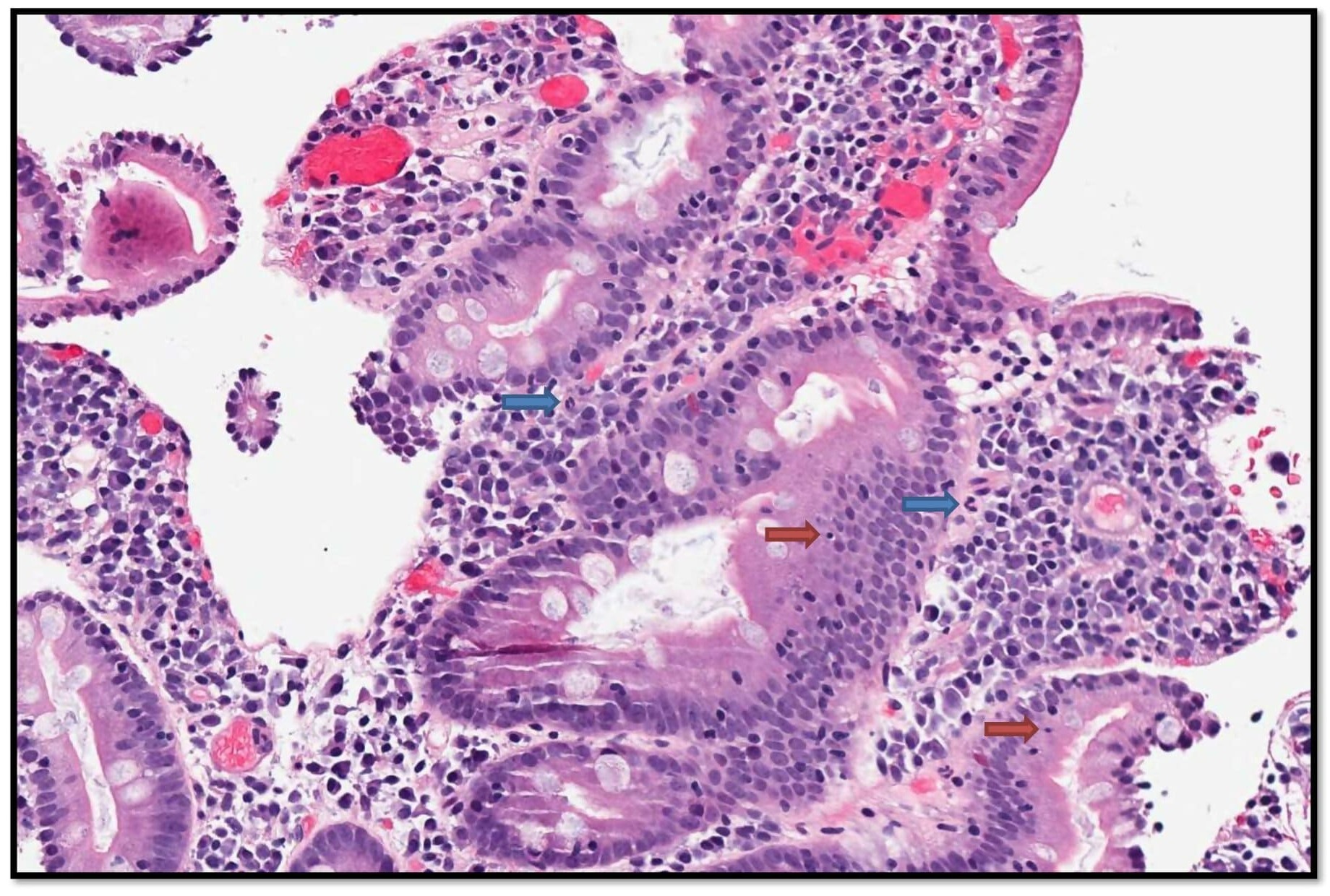
Case Description/Methods: A 31-year-old woman presented with intermittent ongoing diarrhea of six months duration. Workup for infectious causes included stool for ova and parasites, stool cultures, and C. difficile toxin, all of which were negative. Celiac disease antibody testing was negative. CT angiography of the abdomen revealed patent vasculature, devoid of stenosis or occlusion of the celiac artery, superior mesenteric artery, or inferior mesenteric artery. No evidence of inflammatory bowel disease (IBD) or microscopic colitis was seen on biopsies from the colon. Upper gastrointestinal endoscopy was performed. Duodenal biopsy illustrated cryptitis, glandular apoptosis and increased plasma cells in the lamina propria consistent with severe chronic duodenitis (see figure). A diagnosis of autoimmune enteropathy was presumed and she was initiated on treatment with oral steroids. As an outpatient, she was transitioned to Belimumab, a monoclonal antibody that inhibits B cell-activating factor. She remained in sustained remission on follow-up. The response to immunosuppression further supported our diagnosis of AIE.
Discussion: The dearth of adult case reports, and the non-specificity and heterogeneity of clinicopathologic findings make the diagnosis of AIE challenging. Diagnosis requires persistent diarrhea for more than six weeks, malabsorption, distinctive small intestinal histology, and exclusion of alternative causes of villous blunting. The damage is typically confined to the duodenum. Histological patterns can be classified as active chronic duodenitis, celiac disease-like, graft vs host disease-like, and mixed/no predominant pattern. Nutritional optimization and immunosuppression are the cornerstones of treatment. Treatment is often initiated with steroids. Alternative drugs include 6-mercaptopurine, azathioprine, cyclosporine, and tacrolimus. Adalimumab, Vedolizumab, and Ustekinumab have also been successfully used. To our knowledge, this is the first case of AIE successfully treated with Belimumab.
Disclosures:
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Erika Wheeler, MD3, Yuting Huang, MD, PhD1, Robert T. Chow, MD, MBA1, Jamal A. Mikdashi, MD3. D0676 - An Unusual Case of Diarrhea in a Patient With Lupus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2Guntur Medical College, Guntur, Andhra Pradesh, India; 3University of Maryland Medical Center, Baltimore, MD
Introduction: The differential diagnosis of diarrhea in the setting of systemic lupus erythematosus (SLE) is broad and includes lupus-related as well as non-lupus-related etiologies. Lupus-related etiologies include but are not limited to mesenteric vasculitis, pseudo-obstruction, protein-losing enteropathy, and pancreatitis. Autoimmune enteropathy (AIE) is rare in adults, with fewer than fifty cases described in the medical literature. We report a case that responded effectively to Belimumab.
Case Description/Methods: A 31-year-old woman presented with intermittent ongoing diarrhea of six months duration. Workup for infectious causes included stool for ova and parasites, stool cultures, and C. difficile toxin, all of which were negative. Celiac disease antibody testing was negative. CT angiography of the abdomen revealed patent vasculature, devoid of stenosis or occlusion of the celiac artery, superior mesenteric artery, or inferior mesenteric artery. No evidence of inflammatory bowel disease (IBD) or microscopic colitis was seen on biopsies from the colon. Upper gastrointestinal endoscopy was performed. Duodenal biopsy illustrated cryptitis, glandular apoptosis and increased plasma cells in the lamina propria consistent with severe chronic duodenitis (see figure). A diagnosis of autoimmune enteropathy was presumed and she was initiated on treatment with oral steroids. As an outpatient, she was transitioned to Belimumab, a monoclonal antibody that inhibits B cell-activating factor. She remained in sustained remission on follow-up. The response to immunosuppression further supported our diagnosis of AIE.
Discussion: The dearth of adult case reports, and the non-specificity and heterogeneity of clinicopathologic findings make the diagnosis of AIE challenging. Diagnosis requires persistent diarrhea for more than six weeks, malabsorption, distinctive small intestinal histology, and exclusion of alternative causes of villous blunting. The damage is typically confined to the duodenum. Histological patterns can be classified as active chronic duodenitis, celiac disease-like, graft vs host disease-like, and mixed/no predominant pattern. Nutritional optimization and immunosuppression are the cornerstones of treatment. Treatment is often initiated with steroids. Alternative drugs include 6-mercaptopurine, azathioprine, cyclosporine, and tacrolimus. Adalimumab, Vedolizumab, and Ustekinumab have also been successfully used. To our knowledge, this is the first case of AIE successfully treated with Belimumab.
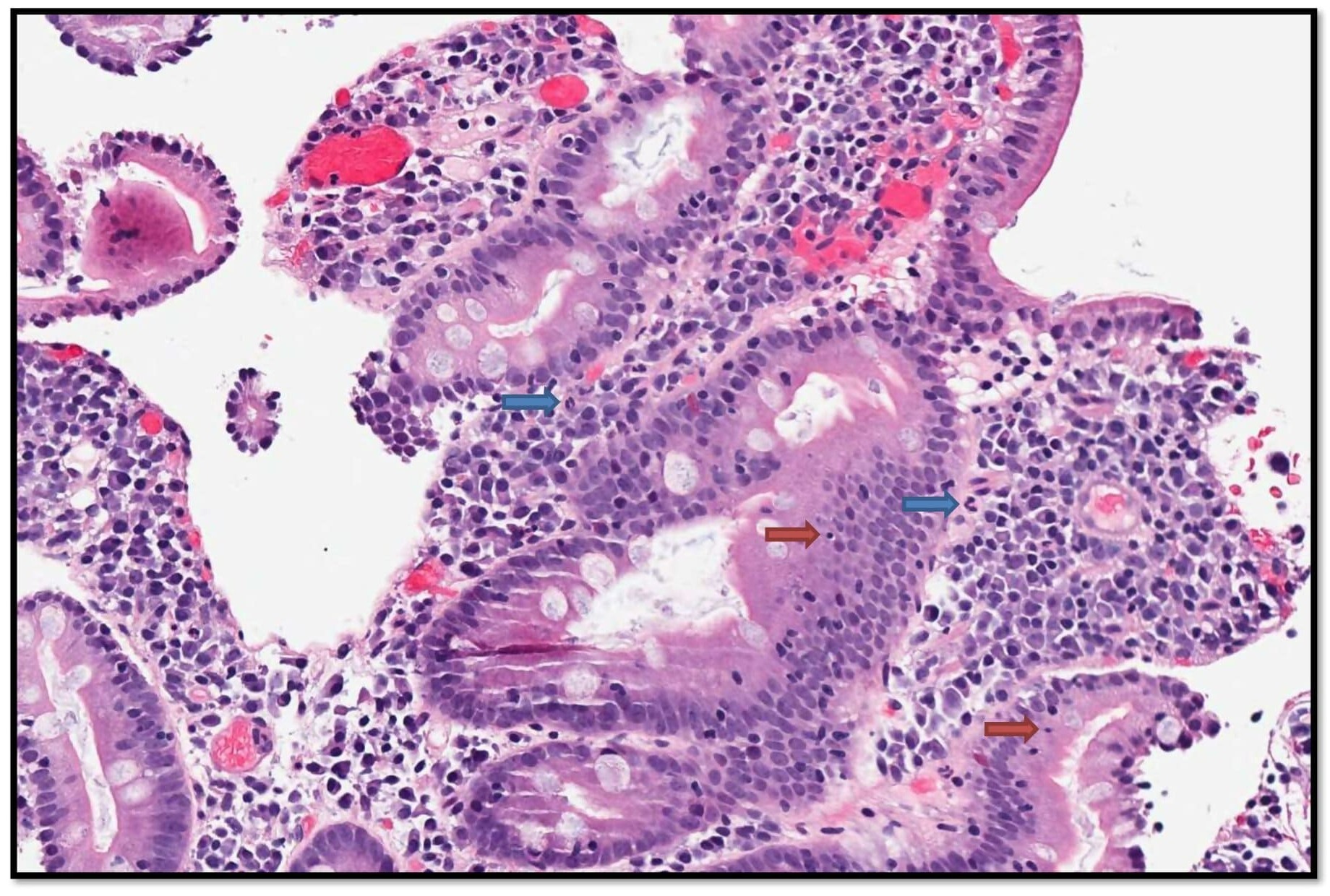
Figure: A higher magnification image of the duodenal biopsy reveals neutrophils (blue arrows) within the lamina propria and apoptotic bodies in the glands, indicating active inflammation and glandular injury. There is also an increase in the plasma cells within the lamina propria, indicating chronicity. This pattern of inflammation is consistent with chronic enteritis. Though this is nonspecific, autoimmune enteropathy is within the differential diagnosis in the appropriate clinical context. (20x)
Disclosures:
Mohammed Rifat Shaik indicated no relevant financial relationships.
Nishat Anjum Shaik indicated no relevant financial relationships.
Erika Wheeler indicated no relevant financial relationships.
Yuting Huang indicated no relevant financial relationships.
Robert Chow indicated no relevant financial relationships.
Jamal Mikdashi indicated no relevant financial relationships.
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Erika Wheeler, MD3, Yuting Huang, MD, PhD1, Robert T. Chow, MD, MBA1, Jamal A. Mikdashi, MD3. D0676 - An Unusual Case of Diarrhea in a Patient With Lupus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
