Back
Poster Session E - Tuesday Afternoon
E0601 - HBV-Host Junctional Sequences: A Novel Urine Tumor Marker for Recurrent Hepatitis B-Associated Hepatocellular Carcinoma With Low Alpha-Fetoprotein
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Dina Halegoua-DeMarzio, MD
Sidney Kimmel Medical College at Thomas Jefferson University
Philadelphia, PA
Presenting Author(s)
Award: Presidential Poster Award
Dina Halegoua-DeMarzio, MD1, Hei-Won Hann, MD1, Selena Lin, MD2, Peter Block, MD1, Grace Park, BS1, Jesse Civan, MD1, Yu-Lan Kao, BS3, Wei Song, MD, PhD2, Ying-Hsiu Su, PhD3
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2JBS Science Inc., Philadelphia, PA; 3Baruch S. Blumberg Institute, Philadelphia, PA
Introduction: Hepatocellular carcinoma (HCC) is one of the most common and deadly cancers worldwide. A common risk factor for liver cancer is chronic infection with the hepatitis B virus (CHB). HCC screening and surveillance is limited by diagnostic accuracy of current testing modalities. Prior studies suggest the potential of urine-based biomarkers for HBV-associated HCC (HBV-HCC), as DNA fragments from both virus and tumor have been detected in urine from those with CHB and HCC. As most HBV-HCC tumors contain integrated components of the HBV genome, unique HBV-host junctional sequences (HBV-JS) represent a viable molecular signature to identify HCC. This study evaluated a novel urine-based biomarker platform, utilizing HBV-JS DNA as a possible marker of tumor recurrence in patients with HBV-HCC.
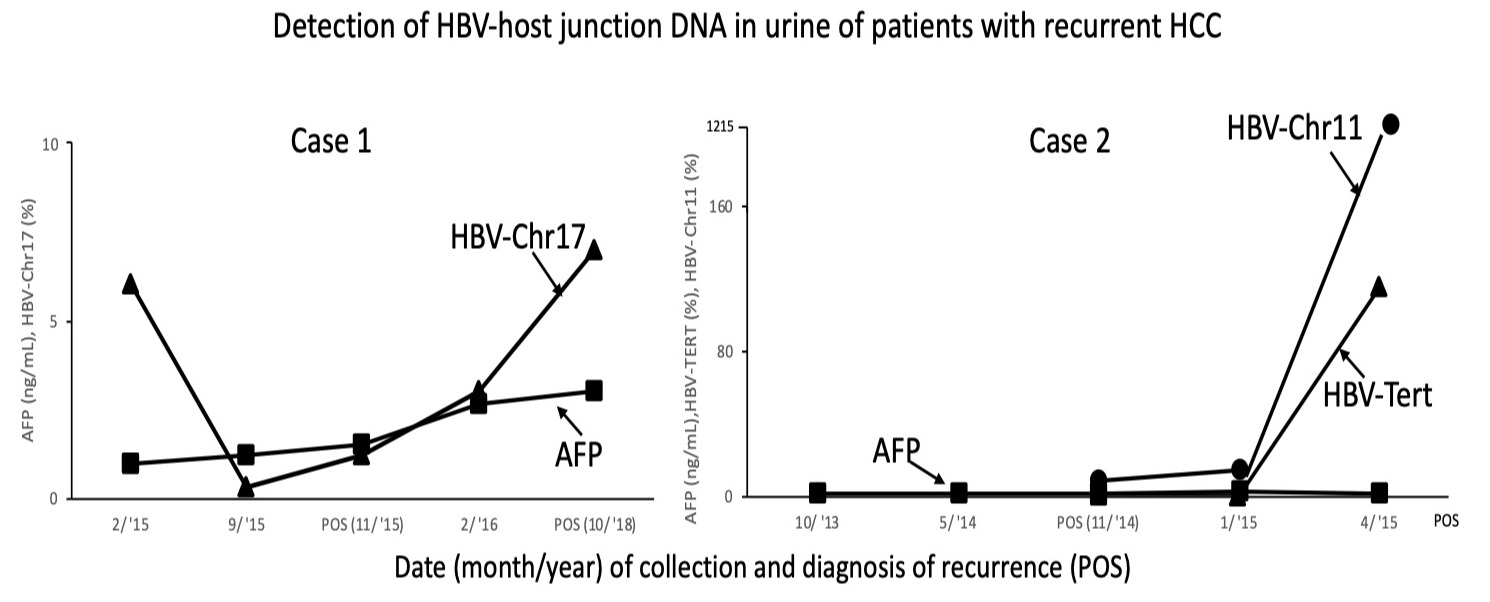
Case Description/Methods: Urine sample from HBV-HCC patients with HCC recurrence confirmed by MRI was obtained. HBV-JS were detected by an HBV-targeted NGS assay (JBS Science Inc., Doylestown, PA) followed by ChimericSeq for junction detection. The most abundant NGS-detected junction sequences were then validated by PCR-Sanger sequencing. Quantitative junction-specific PCR assays were developed to track dynamic changes of HBV-JS in the urine specimens. HBV-JS sequences were detected from 2 cases of HBV-HCC with tumor recurrence (Figure).
Case 1: A 78-year-old female with HBV-related cirrhosis was diagnosed with HCC in 2015. After microwave ablation, follow-up MRI revealed a new LI-RADS 3 lesion 1 year later. Subsequent imaging remained radiographically indeterminate until 2018 when the lesion was classified as definite HCC (LI-RADS 5). While serial AFP levels were negligible and MRI results variable, the unique HBV-JS DNA, HBV-Chr17, steadily increased from initial diagnosis to HCC recurrence.
Case 2: A 74-year-old male with HBV-related cirrhosis was diagnosed with HCC in 2014, which recurred with a LI-RADS 5 lesion after 1 year despite loco-regional therapy. While AFP levels were negligible, two HBV-JS DNA, HBV-Chr11 and HBV-Tert, rapidly increased after initial HCC diagnosis.
Discussion: Unique HBV-JS sequences were detectable in the urine of patients with HBV- HCC. These sequences were detectable at increasing levels prior to diagnosis of recurrence of HCC by MRI imaging or AFP elevation. Together, our data suggest that HBV-JS DNA in urine maybe a further biomarker for the detection of HCC recurrence in patients with HBV-HCC.
Disclosures:
Dina Halegoua-DeMarzio, MD1, Hei-Won Hann, MD1, Selena Lin, MD2, Peter Block, MD1, Grace Park, BS1, Jesse Civan, MD1, Yu-Lan Kao, BS3, Wei Song, MD, PhD2, Ying-Hsiu Su, PhD3. E0601 - HBV-Host Junctional Sequences: A Novel Urine Tumor Marker for Recurrent Hepatitis B-Associated Hepatocellular Carcinoma With Low Alpha-Fetoprotein, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Dina Halegoua-DeMarzio, MD1, Hei-Won Hann, MD1, Selena Lin, MD2, Peter Block, MD1, Grace Park, BS1, Jesse Civan, MD1, Yu-Lan Kao, BS3, Wei Song, MD, PhD2, Ying-Hsiu Su, PhD3
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2JBS Science Inc., Philadelphia, PA; 3Baruch S. Blumberg Institute, Philadelphia, PA
Introduction: Hepatocellular carcinoma (HCC) is one of the most common and deadly cancers worldwide. A common risk factor for liver cancer is chronic infection with the hepatitis B virus (CHB). HCC screening and surveillance is limited by diagnostic accuracy of current testing modalities. Prior studies suggest the potential of urine-based biomarkers for HBV-associated HCC (HBV-HCC), as DNA fragments from both virus and tumor have been detected in urine from those with CHB and HCC. As most HBV-HCC tumors contain integrated components of the HBV genome, unique HBV-host junctional sequences (HBV-JS) represent a viable molecular signature to identify HCC. This study evaluated a novel urine-based biomarker platform, utilizing HBV-JS DNA as a possible marker of tumor recurrence in patients with HBV-HCC.
Case Description/Methods: Urine sample from HBV-HCC patients with HCC recurrence confirmed by MRI was obtained. HBV-JS were detected by an HBV-targeted NGS assay (JBS Science Inc., Doylestown, PA) followed by ChimericSeq for junction detection. The most abundant NGS-detected junction sequences were then validated by PCR-Sanger sequencing. Quantitative junction-specific PCR assays were developed to track dynamic changes of HBV-JS in the urine specimens. HBV-JS sequences were detected from 2 cases of HBV-HCC with tumor recurrence (Figure).
Case 1: A 78-year-old female with HBV-related cirrhosis was diagnosed with HCC in 2015. After microwave ablation, follow-up MRI revealed a new LI-RADS 3 lesion 1 year later. Subsequent imaging remained radiographically indeterminate until 2018 when the lesion was classified as definite HCC (LI-RADS 5). While serial AFP levels were negligible and MRI results variable, the unique HBV-JS DNA, HBV-Chr17, steadily increased from initial diagnosis to HCC recurrence.
Case 2: A 74-year-old male with HBV-related cirrhosis was diagnosed with HCC in 2014, which recurred with a LI-RADS 5 lesion after 1 year despite loco-regional therapy. While AFP levels were negligible, two HBV-JS DNA, HBV-Chr11 and HBV-Tert, rapidly increased after initial HCC diagnosis.
Discussion: Unique HBV-JS sequences were detectable in the urine of patients with HBV- HCC. These sequences were detectable at increasing levels prior to diagnosis of recurrence of HCC by MRI imaging or AFP elevation. Together, our data suggest that HBV-JS DNA in urine maybe a further biomarker for the detection of HCC recurrence in patients with HBV-HCC.
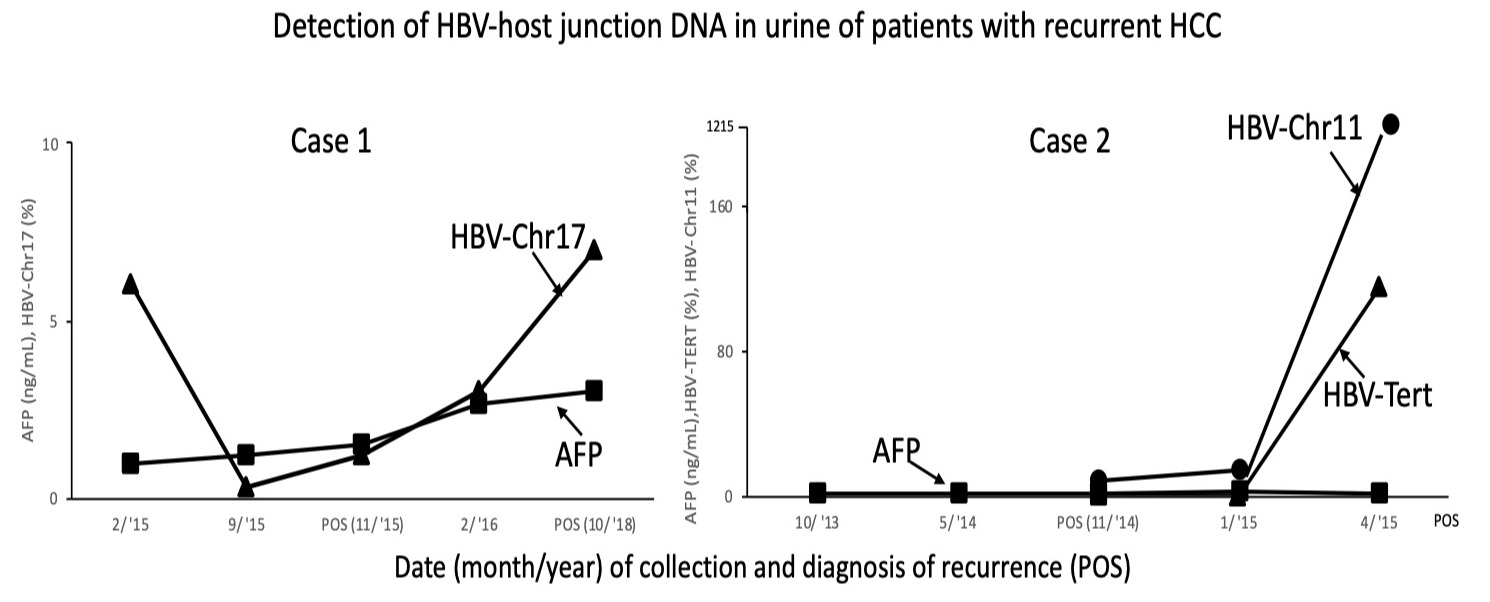
Figure: HBV-host junctional sequences (HBV-JS) were detected from 2 cases of HBV-associated HCC with tumor recurrence
Disclosures:
Dina Halegoua-DeMarzio: Galectin – Grant/Research Support. Intercept – Grant/Research Support. Novo Nordisk – Grant/Research Support. Pfizer – Advisory Committee/Board Member. Viking – Grant/Research Support.
Hei-Won Hann indicated no relevant financial relationships.
Selena Lin indicated no relevant financial relationships.
Peter Block indicated no relevant financial relationships.
Grace Park indicated no relevant financial relationships.
Jesse Civan indicated no relevant financial relationships.
Yu-Lan Kao indicated no relevant financial relationships.
Wei Song indicated no relevant financial relationships.
Ying-Hsiu Su indicated no relevant financial relationships.
Dina Halegoua-DeMarzio, MD1, Hei-Won Hann, MD1, Selena Lin, MD2, Peter Block, MD1, Grace Park, BS1, Jesse Civan, MD1, Yu-Lan Kao, BS3, Wei Song, MD, PhD2, Ying-Hsiu Su, PhD3. E0601 - HBV-Host Junctional Sequences: A Novel Urine Tumor Marker for Recurrent Hepatitis B-Associated Hepatocellular Carcinoma With Low Alpha-Fetoprotein, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

