Back
Poster Session E - Tuesday Afternoon
E0541 - Hepatic Lymphoproliferative Lesions in the Setting of Chronic, Multi-Drug Immunosuppression
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Ivana Radosavljevic, BS
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Ivana Radosavljevic, BS1, Jennifer L. Reed, MD2, Tristan Smith, MD2, Gitanjali Vidyarthi, MD2
1University of South Florida Morsani College of Medicine, Tampa, FL; 2James A. Haley VA Hospital, Tampa, FL
Introduction: Non-Hodgkin’s lymphoma (NHL) is a relatively common cancer, however one that originates in the liver as a primary hepatic lesion is exceedingly rare, making up only 0.016% of NHLs. Understanding the course of this disease is vital to earlier intervention and management. Some researchers have found connections between biologic drugs like TNF-alpha inhibitors and lymphoma, but this association is not well understood or thoroughly documented. Methotrexate has a well-documented association with primary hepatic lymphoma as one of its most serious side effects. The purpose of this case report is to document the course of primary hepatic lymphoproliferative disease in the context of chronic, multi-drug immunosuppression.
Case Description/Methods: This is a 61-year-old African American male with a history of severe rheumatoid arthritis (RA). He was on etanercept/leflunomide therapy from 2001 until 2016. Due to a recurrent scleritis, he was switched to adalimumab in 2016. He was on methotrexate for a year and long-term prednisone therapy since 2011.
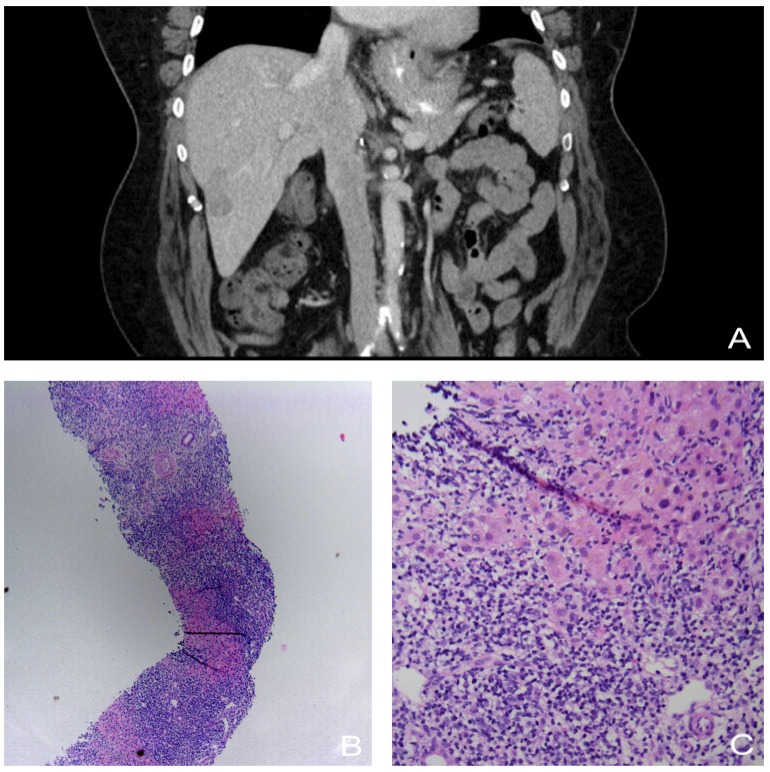
In 2018, an incidental finding on CT imaging showed multiple hypodense lesions in this patient’s liver, as well as splenomegaly. A repeat CT in 2019 redemonstrated the lesions and a follow-up biopsy was suspicious for B cell lymphoproliferative disorder but not confirmatory. A repeat biopsy three months later was non-diagnostic. In 2021, a CT showed scattered, new lesions and old lesions decreased in size. A follow-up biopsy demonstrated atypical lymphoid infiltrates with small lymphoid cells and irregular nuclear contour. Immunohistochemistry stained positive for CD20, mildly positive for LM02 and CD10, and negative for EBER ISH, BCL6, Cyclin D1, and CD23, along with a low Ki67 proliferative index. CEA, AFP, and liver enzyme levels were normal. A month after these results and the discontinuation of adalimumab, a PET scan showed unremarkable findings with no hypermetabolic hepatic lesions.
Discussion: Long-term use of adalimumab is thought to have caused this patient’s lesions while the prednisone simultaneously treated them, explaining the inconclusive biopsies and fluctuating CT findings. Chronically ill patients receiving long term biologic therapy are at greater risk for developing lymphomas, and treating physicians should be hypervigilant and familiar with side-effects and drug-interactions. Further studies are needed to elucidate the influence of these medications on hepatic lymphoproliferative disease processes.
Disclosures:
Ivana Radosavljevic, BS1, Jennifer L. Reed, MD2, Tristan Smith, MD2, Gitanjali Vidyarthi, MD2. E0541 - Hepatic Lymphoproliferative Lesions in the Setting of Chronic, Multi-Drug Immunosuppression, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Tampa, FL; 2James A. Haley VA Hospital, Tampa, FL
Introduction: Non-Hodgkin’s lymphoma (NHL) is a relatively common cancer, however one that originates in the liver as a primary hepatic lesion is exceedingly rare, making up only 0.016% of NHLs. Understanding the course of this disease is vital to earlier intervention and management. Some researchers have found connections between biologic drugs like TNF-alpha inhibitors and lymphoma, but this association is not well understood or thoroughly documented. Methotrexate has a well-documented association with primary hepatic lymphoma as one of its most serious side effects. The purpose of this case report is to document the course of primary hepatic lymphoproliferative disease in the context of chronic, multi-drug immunosuppression.
Case Description/Methods: This is a 61-year-old African American male with a history of severe rheumatoid arthritis (RA). He was on etanercept/leflunomide therapy from 2001 until 2016. Due to a recurrent scleritis, he was switched to adalimumab in 2016. He was on methotrexate for a year and long-term prednisone therapy since 2011.
In 2018, an incidental finding on CT imaging showed multiple hypodense lesions in this patient’s liver, as well as splenomegaly. A repeat CT in 2019 redemonstrated the lesions and a follow-up biopsy was suspicious for B cell lymphoproliferative disorder but not confirmatory. A repeat biopsy three months later was non-diagnostic. In 2021, a CT showed scattered, new lesions and old lesions decreased in size. A follow-up biopsy demonstrated atypical lymphoid infiltrates with small lymphoid cells and irregular nuclear contour. Immunohistochemistry stained positive for CD20, mildly positive for LM02 and CD10, and negative for EBER ISH, BCL6, Cyclin D1, and CD23, along with a low Ki67 proliferative index. CEA, AFP, and liver enzyme levels were normal. A month after these results and the discontinuation of adalimumab, a PET scan showed unremarkable findings with no hypermetabolic hepatic lesions.
Discussion: Long-term use of adalimumab is thought to have caused this patient’s lesions while the prednisone simultaneously treated them, explaining the inconclusive biopsies and fluctuating CT findings. Chronically ill patients receiving long term biologic therapy are at greater risk for developing lymphomas, and treating physicians should be hypervigilant and familiar with side-effects and drug-interactions. Further studies are needed to elucidate the influence of these medications on hepatic lymphoproliferative disease processes.
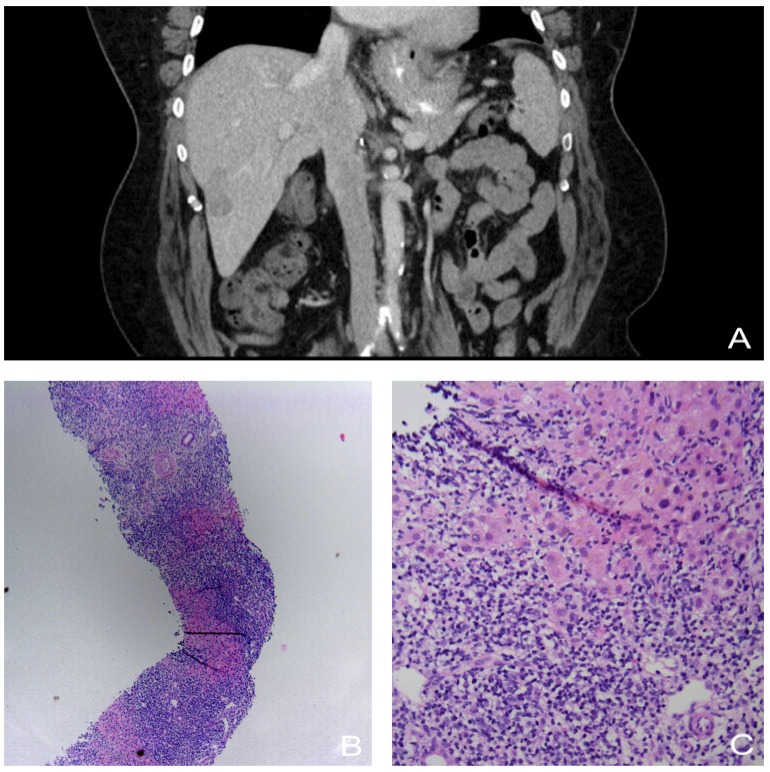
Figure: (A) Liver CT from 2021 depicting an enlarging, hypodense lesion (B) Liver biopsy H&E stain, 4x (C) Liver biopsy H&E stain, 20x
Disclosures:
Ivana Radosavljevic indicated no relevant financial relationships.
Jennifer Reed indicated no relevant financial relationships.
Tristan Smith indicated no relevant financial relationships.
Gitanjali Vidyarthi indicated no relevant financial relationships.
Ivana Radosavljevic, BS1, Jennifer L. Reed, MD2, Tristan Smith, MD2, Gitanjali Vidyarthi, MD2. E0541 - Hepatic Lymphoproliferative Lesions in the Setting of Chronic, Multi-Drug Immunosuppression, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
