Back
Poster Session E - Tuesday Afternoon
E0611 - Transoral Gastric Outlet Reduction Used to Successfully Manage a Case of Refractory Dumping Syndrome Presenting With Recurrent Admissions for Falls and Seizures
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Scott Edelson, MD
Brooke Army Medical Center
Fort Sam Houston, TX
Presenting Author(s)
Scott Edelson, MD1, John Quiles, MD2
1Brooke Army Medical Center, Fort Sam Houston, TX; 2San Antonio Military Medical Center, Fort Sam Houston, TX
Introduction: Surgical management of obesity through Roux-en-Y gastric bypass (RNYGB) has been proven to be a successful treatment for obesity and obesity-related comorbidities. Common adverse events following RNYGB include dumping syndrome, weight regain, vitamin deficiency, and marginal ulceration. Dumping syndrome is a postprandial state where rapid gastric emptying and delivery to the small intestine results in a pattern of GI symptoms including fatigue, tachycardia, and syncope, which can lead to seizures and shock secondary to profound hypoglycemia. Initial treatments include dietary modification and administration of glucagon and octreotide. Treatment for refractory cases previously included surgical revision, but data suggesting endoscopic treatment is promising. We present a report of a patient with RNYGB who developed dumping syndrome treated successfully with transoral gastric outlet reduction (eTOR).
Case Description/Methods: A 47-year-old female with a history of RNYGB 10 years prior with a history of post-prandial hypoglycemia managed with Acarbose, Octreotide and Glucagon was admitted after a fall for seizure-like activity. She was found to be profoundly hypoglycemic. She had a history of multiple prior ED visits and hospital admissions for hypoglycemia and recurrent falls despite multiple attempts at optimization of medical management. Following a multi-disciplinary discussion with bariatric surgery, plans were made to undergo eTOR for management of dumping syndrome.
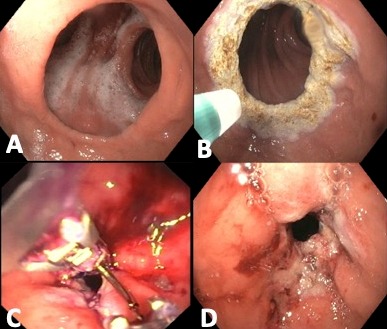
She underwent upper endoscopy which showed a dilated gastrojejunal anastomosis (GJA) measuring approximately 5cm. Argon plasma coagulation at 40 watts and a flow of 0.8L/min to ablate the tissue around the outlet. An Apollo EndoStitch device was then used to place a total of 9 sutures in a double purse-string fashion around the outlet, resulting in a reduction to 9mm. The patient was extubated and returned to the ward.
She was discharged several days later, with stable blood sugar levels. Over the next two weeks, Acarbose, Octreotide and Glucagon were decreased in dose and discontinued. She had not had any additional falls nor ED visits.
Discussion: Patients with dumping syndrome were previously managed by surgical revision, which fell out of favor due to high adverse event rates. This case highlights the ability to use endoscopic full-thickness suturing devices to treat this significant complication of bariatric surgery.
Disclosures:
Scott Edelson, MD1, John Quiles, MD2. E0611 - Transoral Gastric Outlet Reduction Used to Successfully Manage a Case of Refractory Dumping Syndrome Presenting With Recurrent Admissions for Falls and Seizures, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Brooke Army Medical Center, Fort Sam Houston, TX; 2San Antonio Military Medical Center, Fort Sam Houston, TX
Introduction: Surgical management of obesity through Roux-en-Y gastric bypass (RNYGB) has been proven to be a successful treatment for obesity and obesity-related comorbidities. Common adverse events following RNYGB include dumping syndrome, weight regain, vitamin deficiency, and marginal ulceration. Dumping syndrome is a postprandial state where rapid gastric emptying and delivery to the small intestine results in a pattern of GI symptoms including fatigue, tachycardia, and syncope, which can lead to seizures and shock secondary to profound hypoglycemia. Initial treatments include dietary modification and administration of glucagon and octreotide. Treatment for refractory cases previously included surgical revision, but data suggesting endoscopic treatment is promising. We present a report of a patient with RNYGB who developed dumping syndrome treated successfully with transoral gastric outlet reduction (eTOR).
Case Description/Methods: A 47-year-old female with a history of RNYGB 10 years prior with a history of post-prandial hypoglycemia managed with Acarbose, Octreotide and Glucagon was admitted after a fall for seizure-like activity. She was found to be profoundly hypoglycemic. She had a history of multiple prior ED visits and hospital admissions for hypoglycemia and recurrent falls despite multiple attempts at optimization of medical management. Following a multi-disciplinary discussion with bariatric surgery, plans were made to undergo eTOR for management of dumping syndrome.
She underwent upper endoscopy which showed a dilated gastrojejunal anastomosis (GJA) measuring approximately 5cm. Argon plasma coagulation at 40 watts and a flow of 0.8L/min to ablate the tissue around the outlet. An Apollo EndoStitch device was then used to place a total of 9 sutures in a double purse-string fashion around the outlet, resulting in a reduction to 9mm. The patient was extubated and returned to the ward.
She was discharged several days later, with stable blood sugar levels. Over the next two weeks, Acarbose, Octreotide and Glucagon were decreased in dose and discontinued. She had not had any additional falls nor ED visits.
Discussion: Patients with dumping syndrome were previously managed by surgical revision, which fell out of favor due to high adverse event rates. This case highlights the ability to use endoscopic full-thickness suturing devices to treat this significant complication of bariatric surgery.
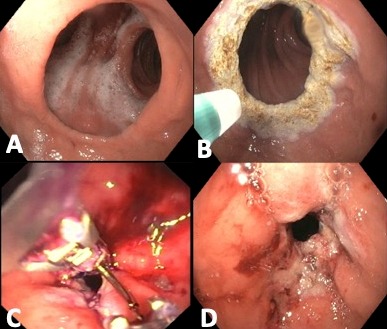
Figure: A. Dilated gastrojejunal anastomosis
B. Ablation of gastrojejunal anastomosis with Argon plasma coagulation
C. Endoscopic placement of sutures around gastrojejunal anastomosis
D. Gastrojejunal anastomosis after reduction
B. Ablation of gastrojejunal anastomosis with Argon plasma coagulation
C. Endoscopic placement of sutures around gastrojejunal anastomosis
D. Gastrojejunal anastomosis after reduction
Disclosures:
Scott Edelson indicated no relevant financial relationships.
John Quiles indicated no relevant financial relationships.
Scott Edelson, MD1, John Quiles, MD2. E0611 - Transoral Gastric Outlet Reduction Used to Successfully Manage a Case of Refractory Dumping Syndrome Presenting With Recurrent Admissions for Falls and Seizures, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
