Back
Poster Session E - Tuesday Afternoon
E0618 - Pathway to Eliminating Fecal Occult Blood Testing at a Tertiary Care Center
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Priya Abhyankar, MD
University of Kentucky
Lexington, KY
Presenting Author(s)
Priya Abhyankar, MD1, Aaron Brenner, MD2, Kshitij Thakur, MD1, Ryan Beyer, MD1, Marijeta Pekez, MD1
1University of Kentucky, Lexington, KY; 2University of Kentucky College of Medicine, Lexington, KY
Introduction: The United States Preventive Services Task Force (USPSTF) recommends fecal occult blood testing as one method for colorectal cancer screening in average risk people. However, the test is often used inappropriately for other indications in admitted patients, leading to unnecessary procedures, false reassurance, and wasted health care dollars. We performed a retrospective review to determine the indications for inpatient fecal occult blood tests (FOBT) and their impact on clinical outcomes at a tertiary care center.
Methods: Our goal was to characterize the current inpatient FOBT ordering patterns at our tertiary care center. We reviewed all the inpatient FOBT ordered between Jan 2018 and Jan 2021 and characterized them based on the ordering department. Internal Medicine (IM) was the most common ordering department. We then conducted a chart review of every fourth IM patient that had an FOBT ordered during the study period. We identified characteristics such as chief complaint, ordering team, indication, the result of the test, if a patient went on to endoscopy, and hemoglobin at the time of test.
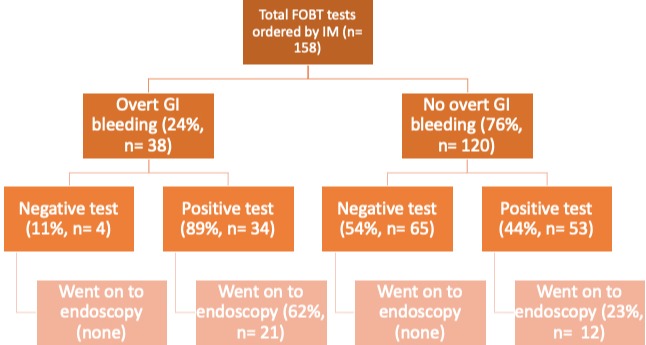
Results: Out of 1446 total orders, IM ordered the most FOBT with 632 tests, followed by family medicine at 369 tests, and cardiology with 135 tests. Among the 158 IM charts reviewed, the most common ordering team was the admission triage team. Ninety percent of tests were ordered by non-teaching teams vs 10% ordered by teaching teams. The IM-ordered tests had a positivity rate of 54% and anemia was the most common indication. The average hemoglobin at time of testing was 8.5 g/dl. Twenty-four percent of patients had signs of overt GI bleeding. In the absence of overt GI bleeding, only 23% of positive FOBT tests led to an inpatient endoscopy (Fig. 1). The proportion of those who underwent endoscopy was higher in those who presented with symptoms of overt GI bleeding than those who did not (56% vs 10%).
Discussion: Our retrospective study highlights that inpatient FOBT are often utilized in the management of anemia in hospitalized patients. Most tests were ordered by non-teaching teams. In the absence of overt bleeding, a positive inpatient FOBT rarely led to endoscopy. Use of FOBT in the inpatient setting is a low value practice. We plan to conduct a further root cause analysis using physician interviews to understand reasoning for inpatient use of this test and design interventions to eliminate inpatient FOBT at our hospital.
Disclosures:
Priya Abhyankar, MD1, Aaron Brenner, MD2, Kshitij Thakur, MD1, Ryan Beyer, MD1, Marijeta Pekez, MD1. E0618 - Pathway to Eliminating Fecal Occult Blood Testing at a Tertiary Care Center, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2University of Kentucky College of Medicine, Lexington, KY
Introduction: The United States Preventive Services Task Force (USPSTF) recommends fecal occult blood testing as one method for colorectal cancer screening in average risk people. However, the test is often used inappropriately for other indications in admitted patients, leading to unnecessary procedures, false reassurance, and wasted health care dollars. We performed a retrospective review to determine the indications for inpatient fecal occult blood tests (FOBT) and their impact on clinical outcomes at a tertiary care center.
Methods: Our goal was to characterize the current inpatient FOBT ordering patterns at our tertiary care center. We reviewed all the inpatient FOBT ordered between Jan 2018 and Jan 2021 and characterized them based on the ordering department. Internal Medicine (IM) was the most common ordering department. We then conducted a chart review of every fourth IM patient that had an FOBT ordered during the study period. We identified characteristics such as chief complaint, ordering team, indication, the result of the test, if a patient went on to endoscopy, and hemoglobin at the time of test.
Results: Out of 1446 total orders, IM ordered the most FOBT with 632 tests, followed by family medicine at 369 tests, and cardiology with 135 tests. Among the 158 IM charts reviewed, the most common ordering team was the admission triage team. Ninety percent of tests were ordered by non-teaching teams vs 10% ordered by teaching teams. The IM-ordered tests had a positivity rate of 54% and anemia was the most common indication. The average hemoglobin at time of testing was 8.5 g/dl. Twenty-four percent of patients had signs of overt GI bleeding. In the absence of overt GI bleeding, only 23% of positive FOBT tests led to an inpatient endoscopy (Fig. 1). The proportion of those who underwent endoscopy was higher in those who presented with symptoms of overt GI bleeding than those who did not (56% vs 10%).
Discussion: Our retrospective study highlights that inpatient FOBT are often utilized in the management of anemia in hospitalized patients. Most tests were ordered by non-teaching teams. In the absence of overt bleeding, a positive inpatient FOBT rarely led to endoscopy. Use of FOBT in the inpatient setting is a low value practice. We plan to conduct a further root cause analysis using physician interviews to understand reasoning for inpatient use of this test and design interventions to eliminate inpatient FOBT at our hospital.
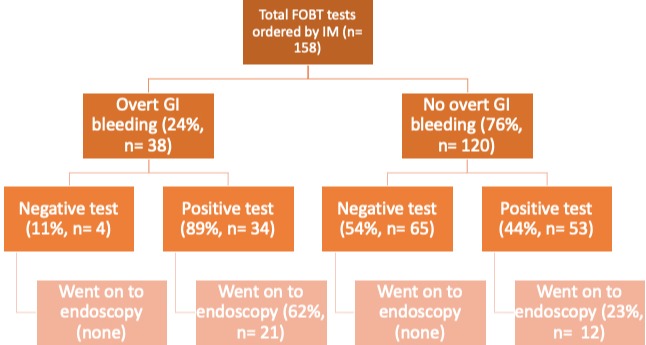
Figure: Figure 1: Flow diagram detailing which patients went on to endoscopy
Disclosures:
Priya Abhyankar indicated no relevant financial relationships.
Aaron Brenner indicated no relevant financial relationships.
Kshitij Thakur indicated no relevant financial relationships.
Ryan Beyer indicated no relevant financial relationships.
Marijeta Pekez indicated no relevant financial relationships.
Priya Abhyankar, MD1, Aaron Brenner, MD2, Kshitij Thakur, MD1, Ryan Beyer, MD1, Marijeta Pekez, MD1. E0618 - Pathway to Eliminating Fecal Occult Blood Testing at a Tertiary Care Center, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

