Back
Poster Session E - Tuesday Afternoon
E0469 - Prophylactic Anticoagulation for Portal Vein Thrombosis in Cirrhosis: A Systematic Review and Meta-Analysis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Matthew Y. Zhao, BS
David Geffen School of Medicine at UCLA
Los Angeles, CA
Presenting Author(s)
Matthew Y. Zhao, BS1, Calvin Yao, MS1, Brittney Ibrahim, 2, Sammy Saab, MD2
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2University of California Los Angeles, Los Angeles, CA
Introduction: Portal vein thrombosis (PVT) results in significant morbidity and mortality in patients with cirrhosis. Data on the safety and efficacy of anticoagulation for PVT prevention is limited, and there remains no consensus in clinical guidelines on the appropriateness of prophylactic anticoagulation for PVT. We performed a systematic review and meta-analysis on outcomes following anticoagulation as PVT prophylaxis in cirrhosis.
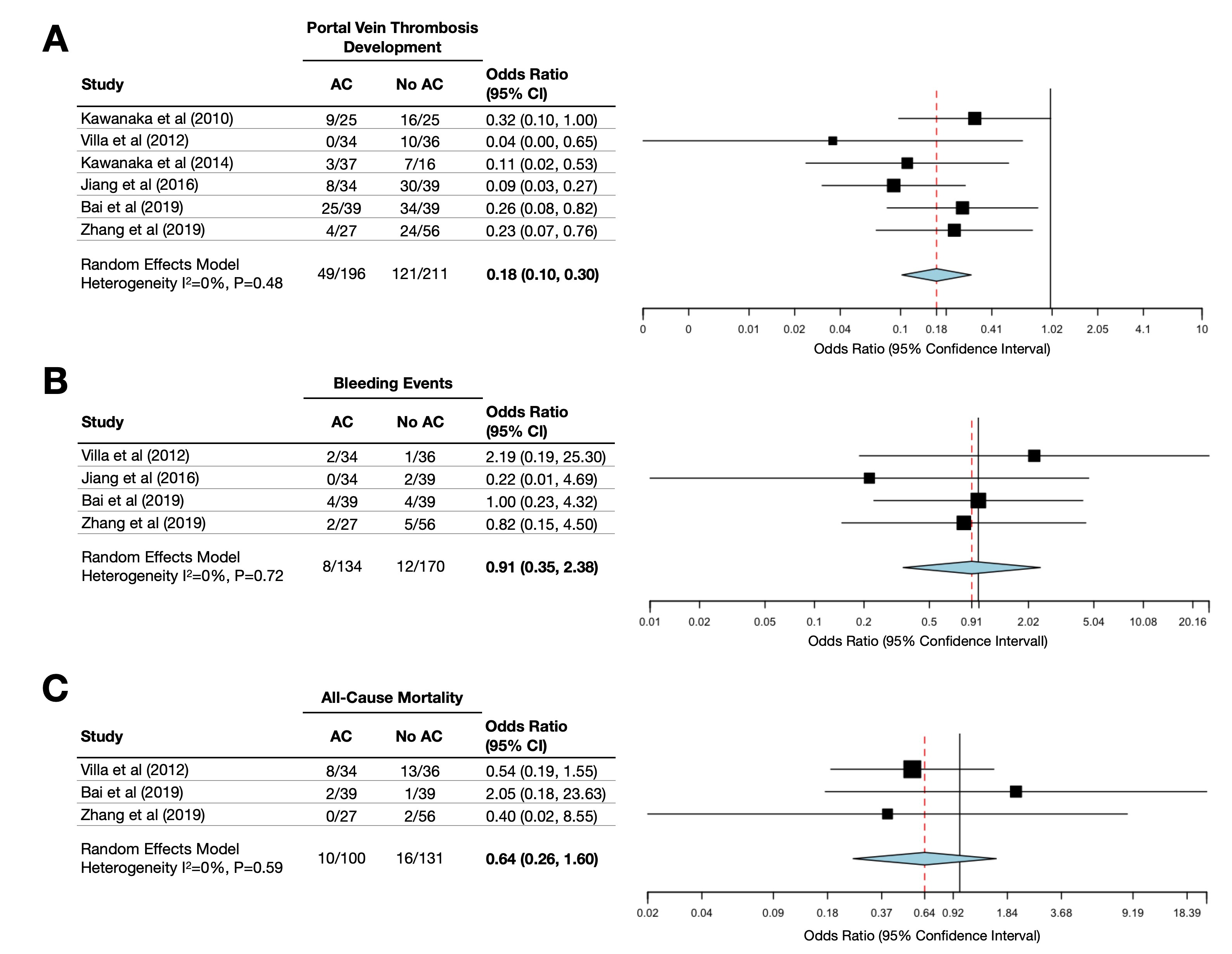
Methods: Pubmed, Embase, and Web of Science were searched from inception to February 13, 2022 for relevant studies. Full length studies comparing anticoagulation to other modalities as prophylaxis against PVT in cirrhosis with at least n=10 patients were included for analysis. Pooled odds ratios (OR) were calculated using a random-effects model for PVT development, bleeding events, and all-cause mortality. Heterogeneity among included studies was assessed using I2 statistics and Cochran Q test. Low heterogeneity was defined as I2 < 50% and Cochran Q p value >0.10. Risk of bias was assessed using the Cochrane risk-of-bias tool for randomized trials (RoB2) and the Risk of Bias in Non-randomized Studies - of Interventions (ROBINS-I) tool.
Results: Our literature search revealed 1,516 records of which 572 duplicates were removed, yielding 944 records for screening. Six studies (n=407) examining prophylactic anticoagulation for PVT were included for analysis, of which two were randomized controlled trials (RCTs) and four were observational studies. Four studies specifically examined prophylactic anticoagulation in patients undergoing laparoscopic splenectomy. Anticoagulation was associated with decreased PVT development (OR 0.18; 95% CI 0.10-0.30) with low heterogeneity (I2=0%; p=0.48), no significant difference in bleeding events (OR 0.91; 95% CI 0.35-2.38) with low heterogeneity (I2=0%; p=0.72), and no significant difference in all-cause mortality (OR 0.64; 95% CI 0.26-1.60) with low heterogeneity (I2=0%; p=0.59).
Discussion: Anticoagulation is effective as prophylaxis against the development of PVT in patients with cirrhosis. Although anticoagulation was associated with lower rates of PVT development, there was no observed difference in bleeding event occurrence or survival. Additional studies will be necessary in order to better characterize the clinical utility of anticoagulation for PVT prevention, and to identify which patients would most benefit from anticoagulation.
Disclosures:
Matthew Y. Zhao, BS1, Calvin Yao, MS1, Brittney Ibrahim, 2, Sammy Saab, MD2. E0469 - Prophylactic Anticoagulation for Portal Vein Thrombosis in Cirrhosis: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2University of California Los Angeles, Los Angeles, CA
Introduction: Portal vein thrombosis (PVT) results in significant morbidity and mortality in patients with cirrhosis. Data on the safety and efficacy of anticoagulation for PVT prevention is limited, and there remains no consensus in clinical guidelines on the appropriateness of prophylactic anticoagulation for PVT. We performed a systematic review and meta-analysis on outcomes following anticoagulation as PVT prophylaxis in cirrhosis.
Methods: Pubmed, Embase, and Web of Science were searched from inception to February 13, 2022 for relevant studies. Full length studies comparing anticoagulation to other modalities as prophylaxis against PVT in cirrhosis with at least n=10 patients were included for analysis. Pooled odds ratios (OR) were calculated using a random-effects model for PVT development, bleeding events, and all-cause mortality. Heterogeneity among included studies was assessed using I2 statistics and Cochran Q test. Low heterogeneity was defined as I2 < 50% and Cochran Q p value >0.10. Risk of bias was assessed using the Cochrane risk-of-bias tool for randomized trials (RoB2) and the Risk of Bias in Non-randomized Studies - of Interventions (ROBINS-I) tool.
Results: Our literature search revealed 1,516 records of which 572 duplicates were removed, yielding 944 records for screening. Six studies (n=407) examining prophylactic anticoagulation for PVT were included for analysis, of which two were randomized controlled trials (RCTs) and four were observational studies. Four studies specifically examined prophylactic anticoagulation in patients undergoing laparoscopic splenectomy. Anticoagulation was associated with decreased PVT development (OR 0.18; 95% CI 0.10-0.30) with low heterogeneity (I2=0%; p=0.48), no significant difference in bleeding events (OR 0.91; 95% CI 0.35-2.38) with low heterogeneity (I2=0%; p=0.72), and no significant difference in all-cause mortality (OR 0.64; 95% CI 0.26-1.60) with low heterogeneity (I2=0%; p=0.59).
Discussion: Anticoagulation is effective as prophylaxis against the development of PVT in patients with cirrhosis. Although anticoagulation was associated with lower rates of PVT development, there was no observed difference in bleeding event occurrence or survival. Additional studies will be necessary in order to better characterize the clinical utility of anticoagulation for PVT prevention, and to identify which patients would most benefit from anticoagulation.
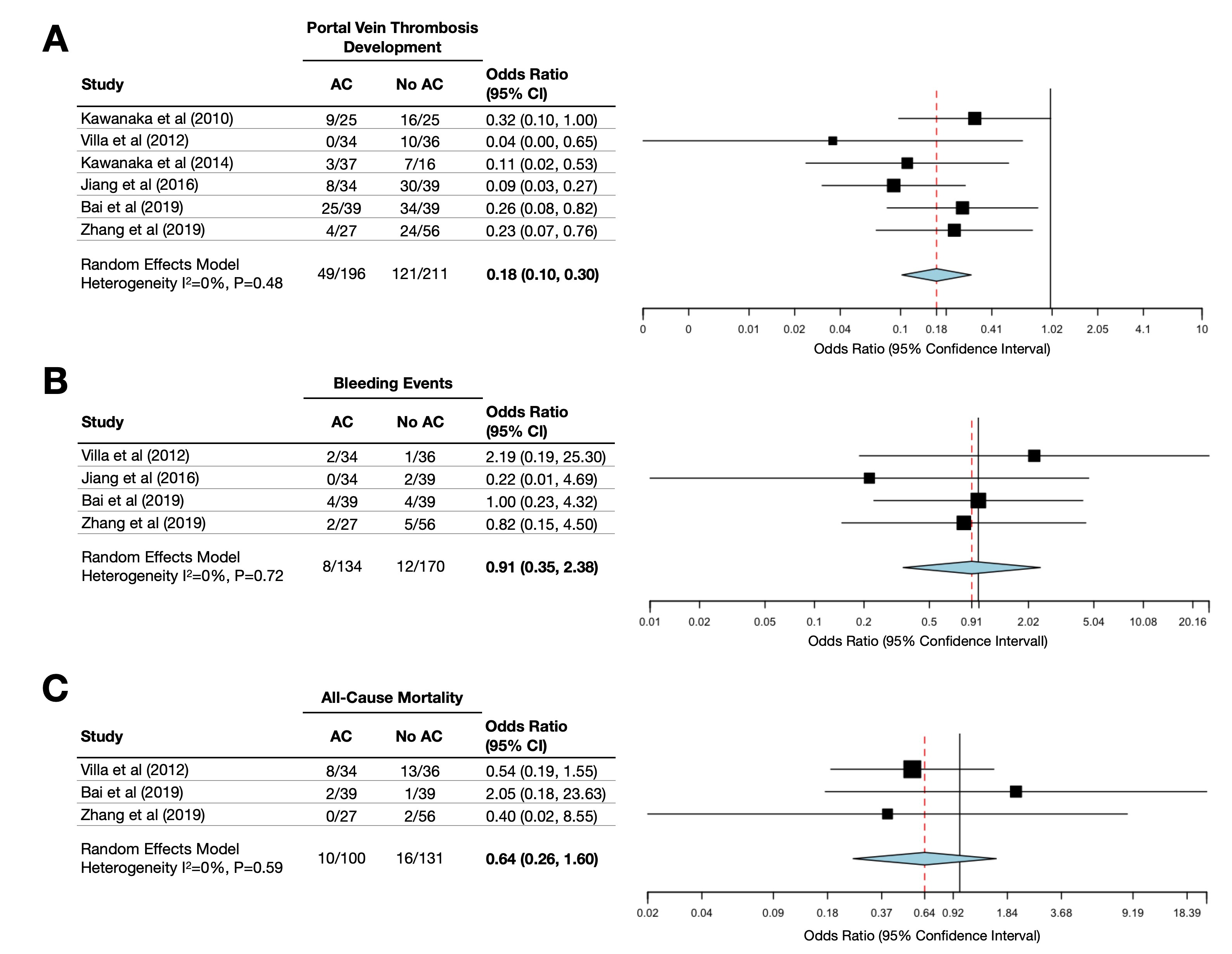
Figure: Forest plots for rate of (A) portal vein thrombosis development, (B) bleeding events, and (C) all-cause mortality following the use of anticoagulation as prophylaxis against portal vein thrombosis in cirrhosis.
Disclosures:
Matthew Zhao indicated no relevant financial relationships.
Calvin Yao indicated no relevant financial relationships.
Brittney Ibrahim indicated no relevant financial relationships.
Sammy Saab indicated no relevant financial relationships.
Matthew Y. Zhao, BS1, Calvin Yao, MS1, Brittney Ibrahim, 2, Sammy Saab, MD2. E0469 - Prophylactic Anticoagulation for Portal Vein Thrombosis in Cirrhosis: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
