Back
Poster Session E - Tuesday Afternoon
E0532 - Remission of Autoimmune Hepatitis Following Autologous Stem Cell Transplantation
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
.jpg)
Zarian Prenatt, DO
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Zarian Prenatt, DO, Brittney Shupp, DO, Lisa Stoll, MD, MPH, Hammad Liaquat, MD, Berhanu Geme, MD
St. Luke's University Health Network, Bethlehem, PA
Introduction: Autoimmune hepatitis (AIH) is a chronic inflammatory liver disease that typically requires lifelong immunosuppression with medications like corticosteroids and azathioprine to prevent fibrosis. We present a patient with type 1 autoimmune hepatitis who achieved biochemical remission following autologous stem cell (SC) transplantation for IgA multiple myeloma.
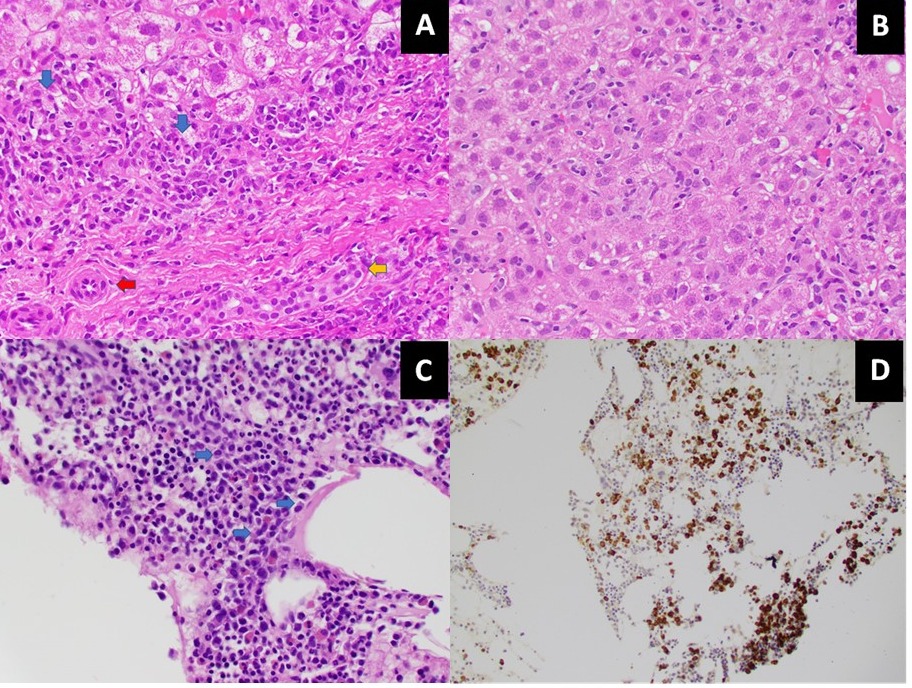
Case Description/Methods: A 67-year-old female with a history of GERD, hypertension, type 2 diabetes, hypothyroidism, and CKD 3 presented in February 2016 with abdominal pain and jaundice. Labs were notable for an AST 1198 U/L, ALT 950 U/L, alkaline phosphatase 244 U/L and total bilirubin 8.09 mg/dL. A hepatitis panel was negative and drug-induced liver injury was ruled out. However, anti-nuclear antibody was found to be positive and anti-smooth muscle antibody IgG was elevated at 191 U. The diagnosis of type 1 AIH was later confirmed by liver biopsy (Image A & B), which revealed chronic active hepatitis with portal lymphoplasmacytic inflammation and stage 2 fibrosis according to the Ludwig-Batts classification. She was started on prednisone and azathioprine. Steroids were able to be withdrawn, but she remained on azathioprine and Ursodiol for multiple years due to recurrent exacerbations. In October 2018, the patient was diagnosed with multiple myeloma confirmed on bone marrow biopsy (Image C & D), which demonstrated IgA kappa restricted plasma cell myeloma. Prednisone, Ursodiol, and azathioprine were all discontinued, and the patient then underwent an autologous SC transplantation in May 2019. She has since been continued on maintenance ixazomib and low dose dexamethasone once weekly but has been monitored off her previous AIH therapies for over 2 years. Now two years following SC transplantation, she remains in biochemical remission and has achieved normalization of her liver enzymes. She currently has her LFT’s monitored every 6 months.
Discussion: Treatment options for AIH remain limited to immunosuppressant medications like corticosteroids and azathioprine, which can lead to substantial adverse side effects. Although limited data exists and additional clinical investigations are required, many have postulated the effects of SC transplantation in patients with AIH given their promising results in animal studies. Therefore, our case encourages further studies investigating the use of stem cells as an alternative treatment for AIH or as a synergistic therapy in patients whose AIH remains uncontrolled.
Disclosures:
Zarian Prenatt, DO, Brittney Shupp, DO, Lisa Stoll, MD, MPH, Hammad Liaquat, MD, Berhanu Geme, MD. E0532 - Remission of Autoimmune Hepatitis Following Autologous Stem Cell Transplantation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
St. Luke's University Health Network, Bethlehem, PA
Introduction: Autoimmune hepatitis (AIH) is a chronic inflammatory liver disease that typically requires lifelong immunosuppression with medications like corticosteroids and azathioprine to prevent fibrosis. We present a patient with type 1 autoimmune hepatitis who achieved biochemical remission following autologous stem cell (SC) transplantation for IgA multiple myeloma.
Case Description/Methods: A 67-year-old female with a history of GERD, hypertension, type 2 diabetes, hypothyroidism, and CKD 3 presented in February 2016 with abdominal pain and jaundice. Labs were notable for an AST 1198 U/L, ALT 950 U/L, alkaline phosphatase 244 U/L and total bilirubin 8.09 mg/dL. A hepatitis panel was negative and drug-induced liver injury was ruled out. However, anti-nuclear antibody was found to be positive and anti-smooth muscle antibody IgG was elevated at 191 U. The diagnosis of type 1 AIH was later confirmed by liver biopsy (Image A & B), which revealed chronic active hepatitis with portal lymphoplasmacytic inflammation and stage 2 fibrosis according to the Ludwig-Batts classification. She was started on prednisone and azathioprine. Steroids were able to be withdrawn, but she remained on azathioprine and Ursodiol for multiple years due to recurrent exacerbations. In October 2018, the patient was diagnosed with multiple myeloma confirmed on bone marrow biopsy (Image C & D), which demonstrated IgA kappa restricted plasma cell myeloma. Prednisone, Ursodiol, and azathioprine were all discontinued, and the patient then underwent an autologous SC transplantation in May 2019. She has since been continued on maintenance ixazomib and low dose dexamethasone once weekly but has been monitored off her previous AIH therapies for over 2 years. Now two years following SC transplantation, she remains in biochemical remission and has achieved normalization of her liver enzymes. She currently has her LFT’s monitored every 6 months.
Discussion: Treatment options for AIH remain limited to immunosuppressant medications like corticosteroids and azathioprine, which can lead to substantial adverse side effects. Although limited data exists and additional clinical investigations are required, many have postulated the effects of SC transplantation in patients with AIH given their promising results in animal studies. Therefore, our case encourages further studies investigating the use of stem cells as an alternative treatment for AIH or as a synergistic therapy in patients whose AIH remains uncontrolled.
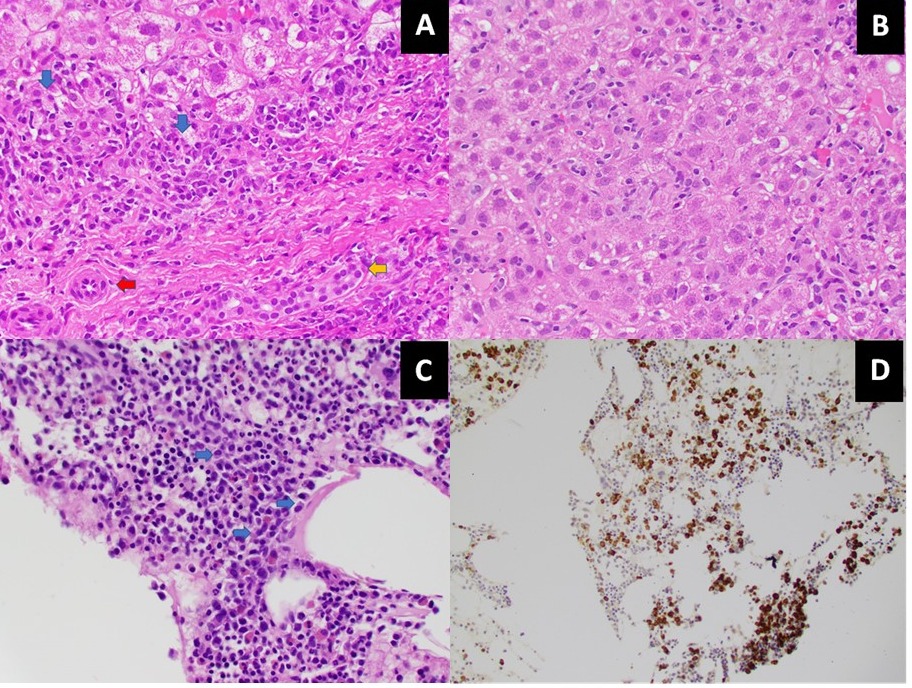
Figure: (A) H&E stain of the liver showing portal tract with artery (red arrow), bile duct (yellow arrow) and interface hepatitis (blue arrow) comprised of numerous plasma cells and scattered lymphocytes. (B) H&E stain of the liver showing lobular inflammation consisting of lymphocytes. (C) H&E stain of the bone marrow showing cellular marrow with numerous plasma cells (blue arrows). (D) Bone marrow, Kappa in situ hybridization reveals Kappa-light chain restricted plasma cell neoplasm.
Disclosures:
Zarian Prenatt indicated no relevant financial relationships.
Brittney Shupp indicated no relevant financial relationships.
Lisa Stoll indicated no relevant financial relationships.
Hammad Liaquat indicated no relevant financial relationships.
Berhanu Geme indicated no relevant financial relationships.
Zarian Prenatt, DO, Brittney Shupp, DO, Lisa Stoll, MD, MPH, Hammad Liaquat, MD, Berhanu Geme, MD. E0532 - Remission of Autoimmune Hepatitis Following Autologous Stem Cell Transplantation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
