Back
Poster Session E - Tuesday Afternoon
E0557 - Seronegative Autoimmune Hepatitis: A Rare Manifestation of COVID-19
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Hwe Won E. Lee, DO
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Hwe Won E. Lee, DO1, Julia Zhang, MD2, Ronak Gandhi, DO3, Alyeesha B. Wilhelm, MD1, Sheharyar K. Merwat, MBBS1, Heather L. Stevenson, MD, PhD1, Julieanna Camarena, DO1
1University of Texas Medical Branch, Galveston, TX; 2UTMB, Galveston, TX; 3University of Texas Medical Branch at Galveston, Galveston, TX
Introduction: Hepatic dysfunction is seen in 14-53% of patients with COVID-19, particularly in those with significant comorbidities. There have been reports of the development of autoimmune hepatitis (AIH) following COVID-19 vaccination and/or infection. AIH is usually associated with circulating autoantibodies but 10-20% of AIH patients are initially seronegative.
We present the first reported episode to our knowledge of a case of seronegative AIH in the setting of concurrent COVID-19 infection.
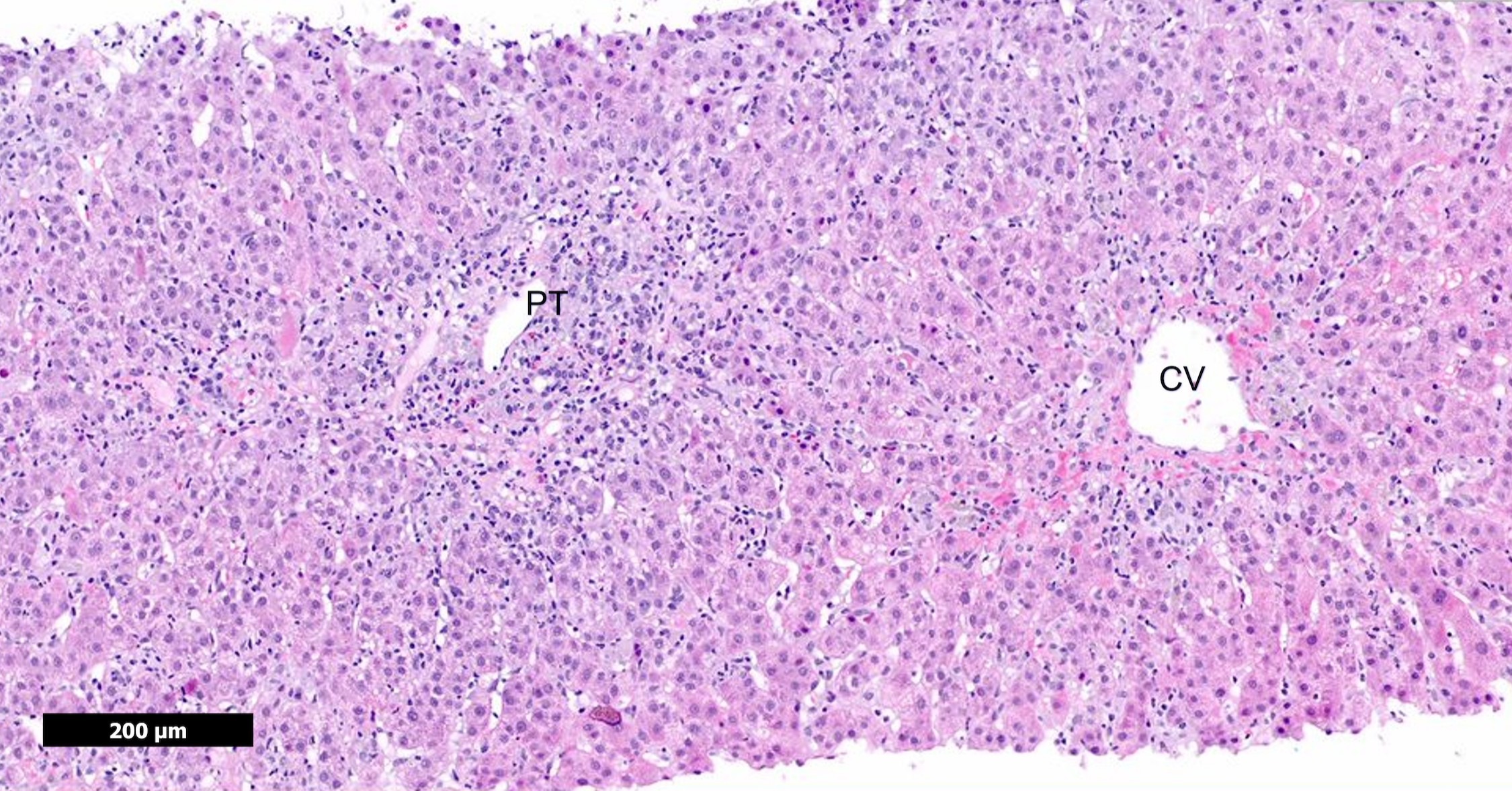
Case Description/Methods: A 39-year-old otherwise healthy female with a family history of mother with rheumatoid arthritis presented with 2 weeks of nausea, diarrhea, abdominal pain, and jaundice. She had significant transaminitis in the 1000s and a conjugated hyperbilirubinemia. Despite previous vaccination and no respiratory symptoms, the patient tested positive for COVID-19. The patient denied taking hepatotoxic agents, and the workup was negative for acute viral hepatitis. The antinuclear, alpha-1-antitrypsin, ceruloplasmin, IgG, anti-smooth muscle, anti-mitochondrial, anti-neutrophil cytoplasmic, and anti-liver/kidney microsomal-1 antibodies were all unremarkable. Imaging was only remarkable for hepatic hemangiomas. Liver biopsy was ultimately performed showing active lymphoplasmacytic hepatitis with prominent regenerative changes and areas of confluent necrosis, consistent with autoimmune hepatitis. The patient’s symptoms and transaminitis improved following initiation of steroids.
Discussion: We present a unique case of AIH as a manifestation of COVID-19 infection despite negative serology. Hepatic injury from COVID-19 is thought to be mediated by multitude of mechanisms including upregulation of ACE2 and DPP4 receptors, which are involved in RAS signaling pathways and regulation of the immune system. Further research is needed to better understand if there is a causal link between COVID-19 and hepatic autoimmune dysfunction and the underlying molecular mechanisms. Identifying autoimmune dysfunction following COVID-19 infection may allow us to recognize and treat these cases early on, leading to better hospitalization outcomes.
Disclosures:
Hwe Won E. Lee, DO1, Julia Zhang, MD2, Ronak Gandhi, DO3, Alyeesha B. Wilhelm, MD1, Sheharyar K. Merwat, MBBS1, Heather L. Stevenson, MD, PhD1, Julieanna Camarena, DO1. E0557 - Seronegative Autoimmune Hepatitis: A Rare Manifestation of COVID-19, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2UTMB, Galveston, TX; 3University of Texas Medical Branch at Galveston, Galveston, TX
Introduction: Hepatic dysfunction is seen in 14-53% of patients with COVID-19, particularly in those with significant comorbidities. There have been reports of the development of autoimmune hepatitis (AIH) following COVID-19 vaccination and/or infection. AIH is usually associated with circulating autoantibodies but 10-20% of AIH patients are initially seronegative.
We present the first reported episode to our knowledge of a case of seronegative AIH in the setting of concurrent COVID-19 infection.
Case Description/Methods: A 39-year-old otherwise healthy female with a family history of mother with rheumatoid arthritis presented with 2 weeks of nausea, diarrhea, abdominal pain, and jaundice. She had significant transaminitis in the 1000s and a conjugated hyperbilirubinemia. Despite previous vaccination and no respiratory symptoms, the patient tested positive for COVID-19. The patient denied taking hepatotoxic agents, and the workup was negative for acute viral hepatitis. The antinuclear, alpha-1-antitrypsin, ceruloplasmin, IgG, anti-smooth muscle, anti-mitochondrial, anti-neutrophil cytoplasmic, and anti-liver/kidney microsomal-1 antibodies were all unremarkable. Imaging was only remarkable for hepatic hemangiomas. Liver biopsy was ultimately performed showing active lymphoplasmacytic hepatitis with prominent regenerative changes and areas of confluent necrosis, consistent with autoimmune hepatitis. The patient’s symptoms and transaminitis improved following initiation of steroids.
Discussion: We present a unique case of AIH as a manifestation of COVID-19 infection despite negative serology. Hepatic injury from COVID-19 is thought to be mediated by multitude of mechanisms including upregulation of ACE2 and DPP4 receptors, which are involved in RAS signaling pathways and regulation of the immune system. Further research is needed to better understand if there is a causal link between COVID-19 and hepatic autoimmune dysfunction and the underlying molecular mechanisms. Identifying autoimmune dysfunction following COVID-19 infection may allow us to recognize and treat these cases early on, leading to better hospitalization outcomes.
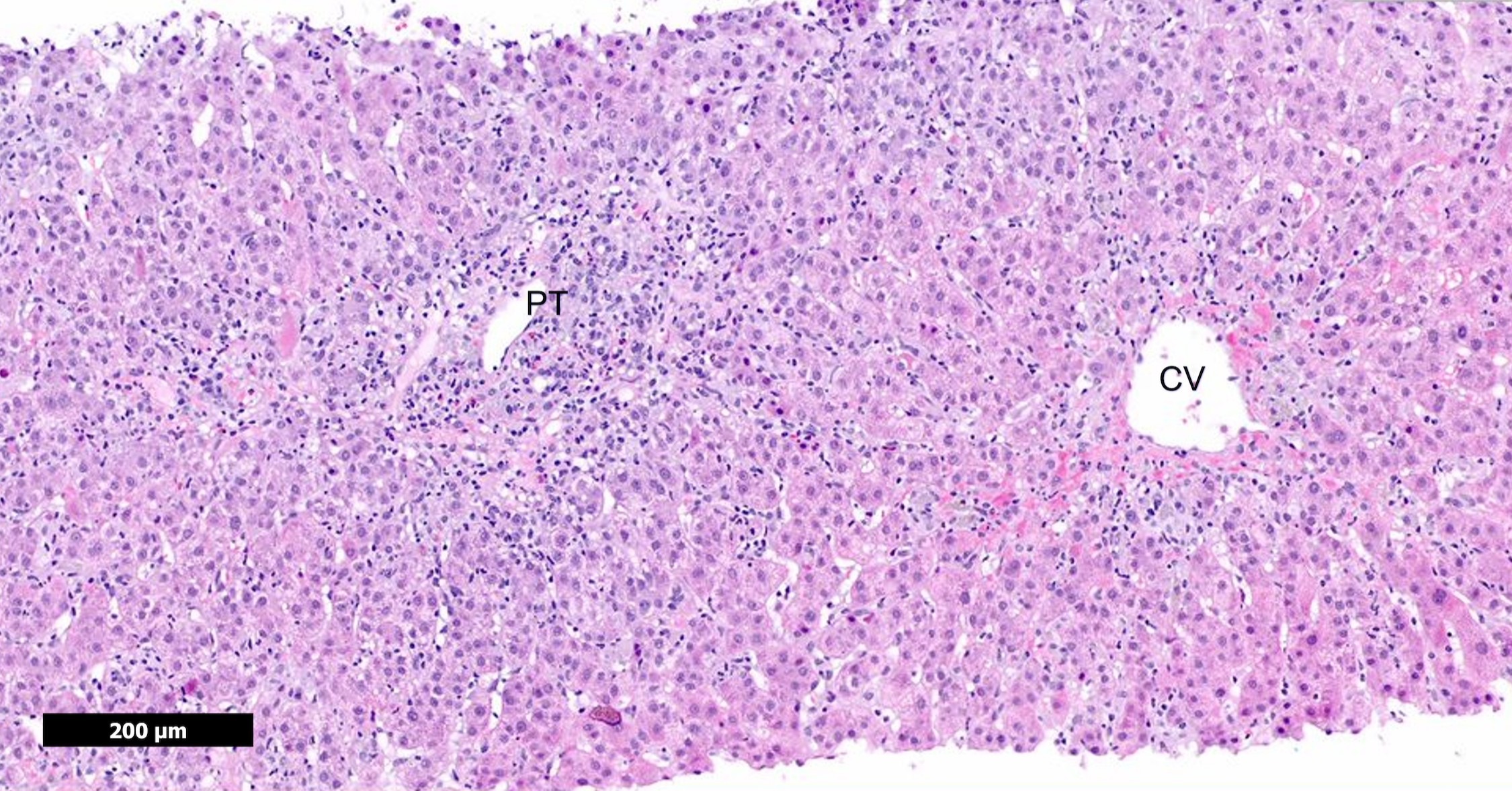
Figure: Figure 1. Liver biopsy showing marked interface activity and areas of confluent necrosis consistent with autoimmune hepatitis (AIH). A representative portal tract (PT) and central vein (CV) are illustrated.
Disclosures:
Hwe Won Lee indicated no relevant financial relationships.
Julia Zhang indicated no relevant financial relationships.
Ronak Gandhi indicated no relevant financial relationships.
Alyeesha Wilhelm indicated no relevant financial relationships.
Sheharyar Merwat indicated no relevant financial relationships.
Heather Stevenson indicated no relevant financial relationships.
Julieanna Camarena indicated no relevant financial relationships.
Hwe Won E. Lee, DO1, Julia Zhang, MD2, Ronak Gandhi, DO3, Alyeesha B. Wilhelm, MD1, Sheharyar K. Merwat, MBBS1, Heather L. Stevenson, MD, PhD1, Julieanna Camarena, DO1. E0557 - Seronegative Autoimmune Hepatitis: A Rare Manifestation of COVID-19, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
