Back
Poster Session C - Monday Afternoon
C0472 - Splenic Vascular Laceration After Endoscopic Necrosectomy and Cyst-Gastrostomy Placement
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Ameya Deshmukh, DO
Saint Louis University School of Medicine
St. Louis, MO
Presenting Author(s)
Ameya Deshmukh, DO1, Zarir Ahmed, DO2, Michelle Baliss, DO2, Jason Taylor, MD2, Antonio Cheesman, MD2
1Saint Louis University School of Medicine, St. Louis, MO; 2Saint Louis University, St. Louis, MO
Introduction: Endoscopic cyst-gastrostomy and necrosectomy have been shown to be highly effective in the treatment of pancreatic walled of necrosis (WON). However, these procedures can be associated with significant complications including bleeding, infection, and perforation. Herein, we describe a case of upper GI bleeding secondary to erosion of a cyst-gastrostomy stent array into the splenic vasculature.
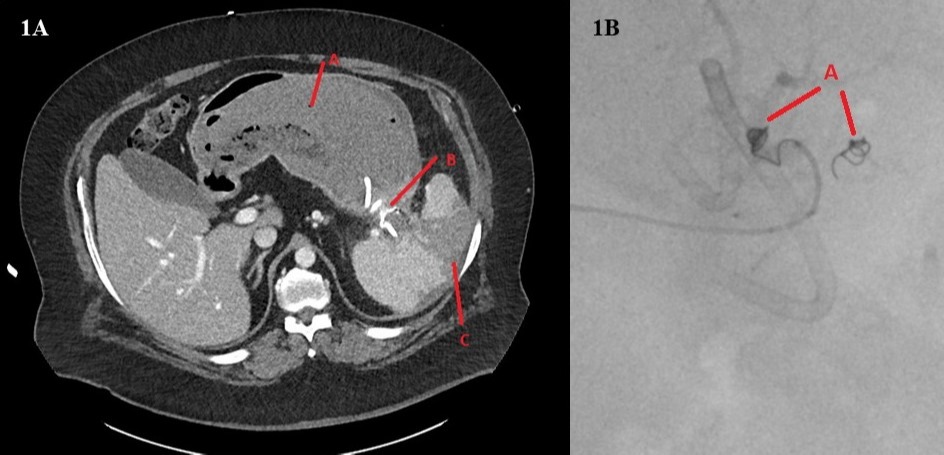
Case Description/Methods: A 45-year-old male with a history of chronic pancreatitis presented to the emergency room with acute-onset hematemesis, melena, and abdominal pain. Two weeks prior, he presented to an outside hospital with abdominal pain and vomiting. He was found to have a 6.7 x 3.4 cm WON collection in the pancreatic tail on MRCP. EUS with FNA revealed necrotic debris and was negative for malignancy. Due to ongoing pain and poor oral intake, he underwent EUS-guided cyst-gastrostomy and necrosectomy 1 week later. A hot 10 x 15 mm lumen apposing metal stent (LAMS) was placed with balloon-dilation of the LAMS. Then, necrosectomy of cyst cavity was done via irrigation and suction with placement of coaxial double pigtail plastic stent.
On presentation to our institution, he was afebrile and hypotensive, with a hemoglobin of 11.7 g/dL from 16.2 g/dL one week prior. Emergent abdominal CT angiogram revealed pigtail stent migration into the splenic arterial branches at the splenic hilum, causing splenic artery injury and large splenic infarct. Interventional radiology performed successful coil embolization of the splenic artery with bleeding cessation. The patient progressed well and was discharged home.
Discussion: While endoscopic cyst-gastrostomy provides safe and effective treatment of pancreatic WON, it still carries the potential for serious complications. Prior literature reveals endoscopic therapy has a 26-33% bleeding rate and a mortality rate of 5.8-11%. Stent migration is a relatively rare complication that occurs in 0.7% of patients. In our case, disruption of the splenic vasculature likely resulted from mechanical injury by the cyst-gastrostomy stent. CT angiography is the best initial diagnostic test with excellent sensitivity and specificity. Treatment usually involves transcatheter embolization or surgery for patients with persistent hemodynamic instability. Splenic vascular injury and infarcts, while infrequent, can still occur as immediate and delayed complications and endoscopists should be vigilant of their occurrence post-procedure.
Disclosures:
Ameya Deshmukh, DO1, Zarir Ahmed, DO2, Michelle Baliss, DO2, Jason Taylor, MD2, Antonio Cheesman, MD2. C0472 - Splenic Vascular Laceration After Endoscopic Necrosectomy and Cyst-Gastrostomy Placement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Saint Louis University School of Medicine, St. Louis, MO; 2Saint Louis University, St. Louis, MO
Introduction: Endoscopic cyst-gastrostomy and necrosectomy have been shown to be highly effective in the treatment of pancreatic walled of necrosis (WON). However, these procedures can be associated with significant complications including bleeding, infection, and perforation. Herein, we describe a case of upper GI bleeding secondary to erosion of a cyst-gastrostomy stent array into the splenic vasculature.
Case Description/Methods: A 45-year-old male with a history of chronic pancreatitis presented to the emergency room with acute-onset hematemesis, melena, and abdominal pain. Two weeks prior, he presented to an outside hospital with abdominal pain and vomiting. He was found to have a 6.7 x 3.4 cm WON collection in the pancreatic tail on MRCP. EUS with FNA revealed necrotic debris and was negative for malignancy. Due to ongoing pain and poor oral intake, he underwent EUS-guided cyst-gastrostomy and necrosectomy 1 week later. A hot 10 x 15 mm lumen apposing metal stent (LAMS) was placed with balloon-dilation of the LAMS. Then, necrosectomy of cyst cavity was done via irrigation and suction with placement of coaxial double pigtail plastic stent.
On presentation to our institution, he was afebrile and hypotensive, with a hemoglobin of 11.7 g/dL from 16.2 g/dL one week prior. Emergent abdominal CT angiogram revealed pigtail stent migration into the splenic arterial branches at the splenic hilum, causing splenic artery injury and large splenic infarct. Interventional radiology performed successful coil embolization of the splenic artery with bleeding cessation. The patient progressed well and was discharged home.
Discussion: While endoscopic cyst-gastrostomy provides safe and effective treatment of pancreatic WON, it still carries the potential for serious complications. Prior literature reveals endoscopic therapy has a 26-33% bleeding rate and a mortality rate of 5.8-11%. Stent migration is a relatively rare complication that occurs in 0.7% of patients. In our case, disruption of the splenic vasculature likely resulted from mechanical injury by the cyst-gastrostomy stent. CT angiography is the best initial diagnostic test with excellent sensitivity and specificity. Treatment usually involves transcatheter embolization or surgery for patients with persistent hemodynamic instability. Splenic vascular injury and infarcts, while infrequent, can still occur as immediate and delayed complications and endoscopists should be vigilant of their occurrence post-procedure.
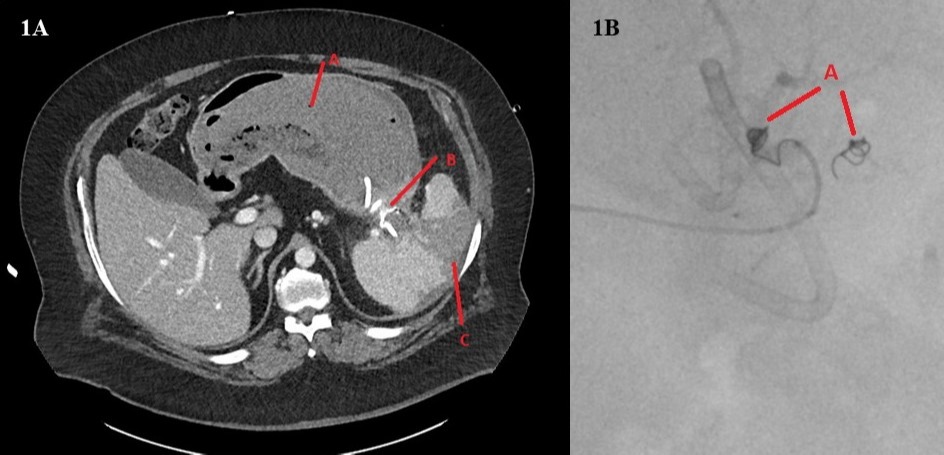
Figure: Figure 1A: Gastric lumen with hemorrhagic material (A). Cyst-gastrostomy connecting stomach and pseudocyst (B). Wedge-shaped splenic infarct (C). Figure 1B: Successful embolization of splenic artery branches with multiple coils (A).
Disclosures:
Ameya Deshmukh indicated no relevant financial relationships.
Zarir Ahmed indicated no relevant financial relationships.
Michelle Baliss indicated no relevant financial relationships.
Jason Taylor indicated no relevant financial relationships.
Antonio Cheesman indicated no relevant financial relationships.
Ameya Deshmukh, DO1, Zarir Ahmed, DO2, Michelle Baliss, DO2, Jason Taylor, MD2, Antonio Cheesman, MD2. C0472 - Splenic Vascular Laceration After Endoscopic Necrosectomy and Cyst-Gastrostomy Placement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
