Back
Poster Session E - Tuesday Afternoon
E0462 - Symptomatic Ménétrier Disease of the Esophageal Inlet Patch Managed With Endoscopic Submucosal Dissection
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Iris Lu
New York Institute of Technology College of Osteopathic Medicine
Old Westbury, NY
Presenting Author(s)
Iris Lu, 1, Ahmad Al-Taee, MD2, Gregory Haber, MD3
1New York Institute of Technology College of Osteopathic Medicine, Old Westbury, NY; 2NYU Grossman School of Medicine, New York, NY; 3NYU Langone Medical Center, New York, NY
Introduction: Ménétrier disease (MD) is a rare protein-losing hypertrophic gastropathy usually confined to the gastric fundus and body. Involvement of the esophageal inlet patch is extremely rare. We report a case of symptomatic MD involving the inlet patch that was managed with endoscopic submucosal dissection (ESD).
Case Description/Methods: A 27-year-old woman with a history of MD was referred to our clinic for further evaluation of dysphagia and globus sensation. She had a family history of MD and gastric adenocarcinoma in her maternal grandmother who passed away at the age of 56. Outside upper endoscopy (EGD) revealed two proximal esophageal lesions, biopsies of which revealed gastric heterotopia.
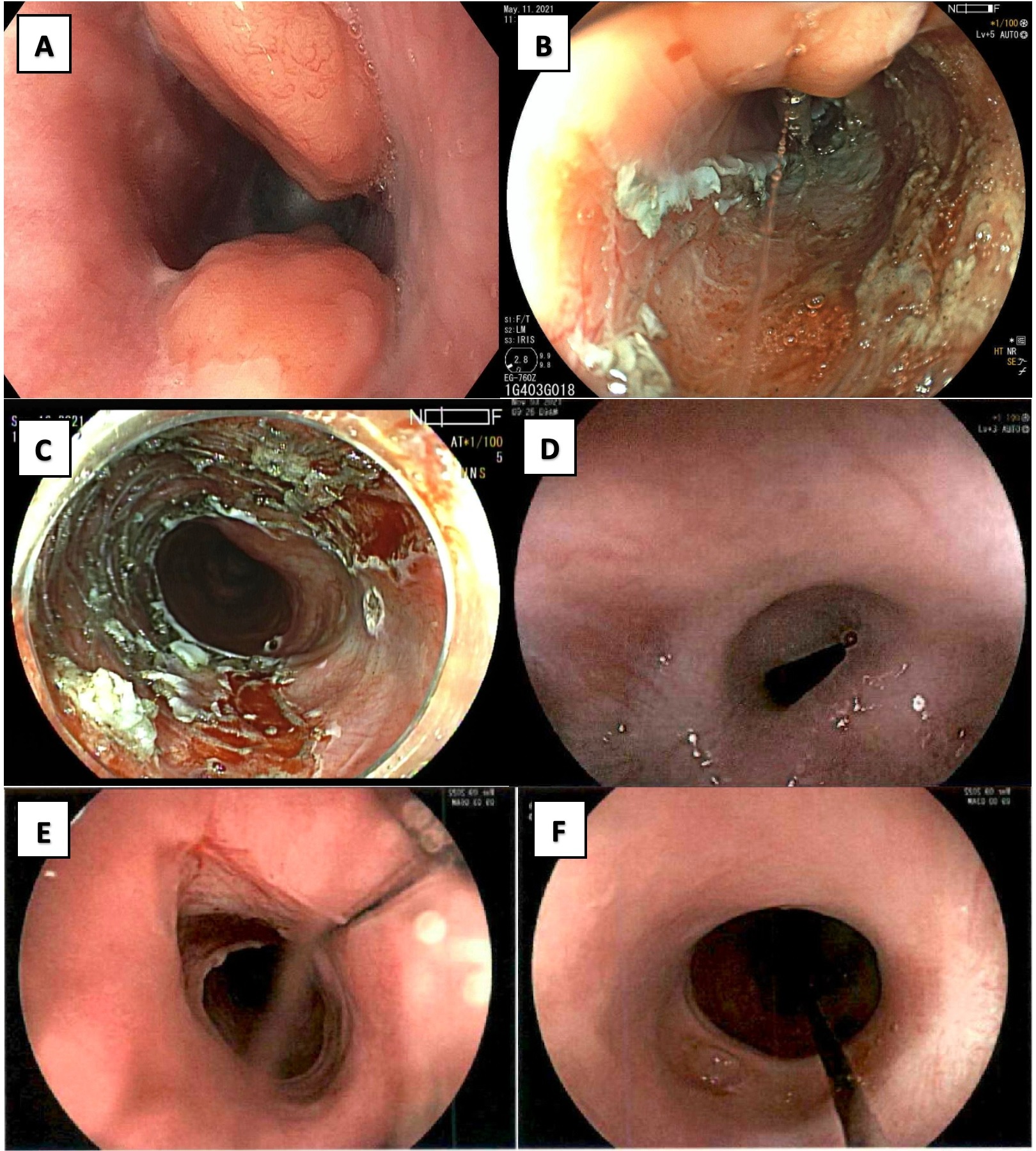
We performed an EGD with endoscopic ultrasound. Two 15 and 20-mm subepithelial lesions were found in the proximal esophagus at 18 cm from the incisors (figure 1, panel A), and the lesions appeared to arise from the superficial submucosa. Biopsies revealed hyperplastic gastric foveolar epithelium, consistent with MD involving the esophageal inlet patch.
We proceeded with ESD of the two lesions in two separate sessions. First, ESD of the 20 mm lesion was successful, and histologic examination showed MD with negative margins and no evidence of intestinal metaplasia or dysplasia (figure 1, panel B). One month later, she underwent ESD of the 15 mm lesion (figure 1, panel C). Histologic examination showed MD with negative margins and no evidence of intestinal metaplasia or dysplasia. The patient continued to report dysphagia and underwent EGD 3 weeks later which showed a benign-appearing esophageal stricture at the ESD site (figure 1, panel D). This was dilated to 12mm. She then underwent three more dilations to 12, 13, and 15mm at 6, 10, and 22 weeks later, respectively (figure 1, panels E and F). There was no evidence of residual or recurrent disease on any of the repeat endoscopies. The patient has remained symptom-free for 3 months now.
Discussion: To our knowledge, this is the first report of symptomatic MD involving the esophageal inlet patch that was managed with ESD for two reasons. First, the lesions appeared to arise from the superficial submucosa. Second, underlying malignancy could not be ruled out in either lesion given family history of gastric adenocarcinoma. In patients with symptomatic MD at high-risk of gastric adenocarcinoma, ESD, when compared with mucosal resection, has the advantage of en-bloc resection which in the setting of malignancy can provide staging data and can be potentially curative.
Disclosures:
Iris Lu, 1, Ahmad Al-Taee, MD2, Gregory Haber, MD3. E0462 - Symptomatic Ménétrier Disease of the Esophageal Inlet Patch Managed With Endoscopic Submucosal Dissection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1New York Institute of Technology College of Osteopathic Medicine, Old Westbury, NY; 2NYU Grossman School of Medicine, New York, NY; 3NYU Langone Medical Center, New York, NY
Introduction: Ménétrier disease (MD) is a rare protein-losing hypertrophic gastropathy usually confined to the gastric fundus and body. Involvement of the esophageal inlet patch is extremely rare. We report a case of symptomatic MD involving the inlet patch that was managed with endoscopic submucosal dissection (ESD).
Case Description/Methods: A 27-year-old woman with a history of MD was referred to our clinic for further evaluation of dysphagia and globus sensation. She had a family history of MD and gastric adenocarcinoma in her maternal grandmother who passed away at the age of 56. Outside upper endoscopy (EGD) revealed two proximal esophageal lesions, biopsies of which revealed gastric heterotopia.
We performed an EGD with endoscopic ultrasound. Two 15 and 20-mm subepithelial lesions were found in the proximal esophagus at 18 cm from the incisors (figure 1, panel A), and the lesions appeared to arise from the superficial submucosa. Biopsies revealed hyperplastic gastric foveolar epithelium, consistent with MD involving the esophageal inlet patch.
We proceeded with ESD of the two lesions in two separate sessions. First, ESD of the 20 mm lesion was successful, and histologic examination showed MD with negative margins and no evidence of intestinal metaplasia or dysplasia (figure 1, panel B). One month later, she underwent ESD of the 15 mm lesion (figure 1, panel C). Histologic examination showed MD with negative margins and no evidence of intestinal metaplasia or dysplasia. The patient continued to report dysphagia and underwent EGD 3 weeks later which showed a benign-appearing esophageal stricture at the ESD site (figure 1, panel D). This was dilated to 12mm. She then underwent three more dilations to 12, 13, and 15mm at 6, 10, and 22 weeks later, respectively (figure 1, panels E and F). There was no evidence of residual or recurrent disease on any of the repeat endoscopies. The patient has remained symptom-free for 3 months now.
Discussion: To our knowledge, this is the first report of symptomatic MD involving the esophageal inlet patch that was managed with ESD for two reasons. First, the lesions appeared to arise from the superficial submucosa. Second, underlying malignancy could not be ruled out in either lesion given family history of gastric adenocarcinoma. In patients with symptomatic MD at high-risk of gastric adenocarcinoma, ESD, when compared with mucosal resection, has the advantage of en-bloc resection which in the setting of malignancy can provide staging data and can be potentially curative.
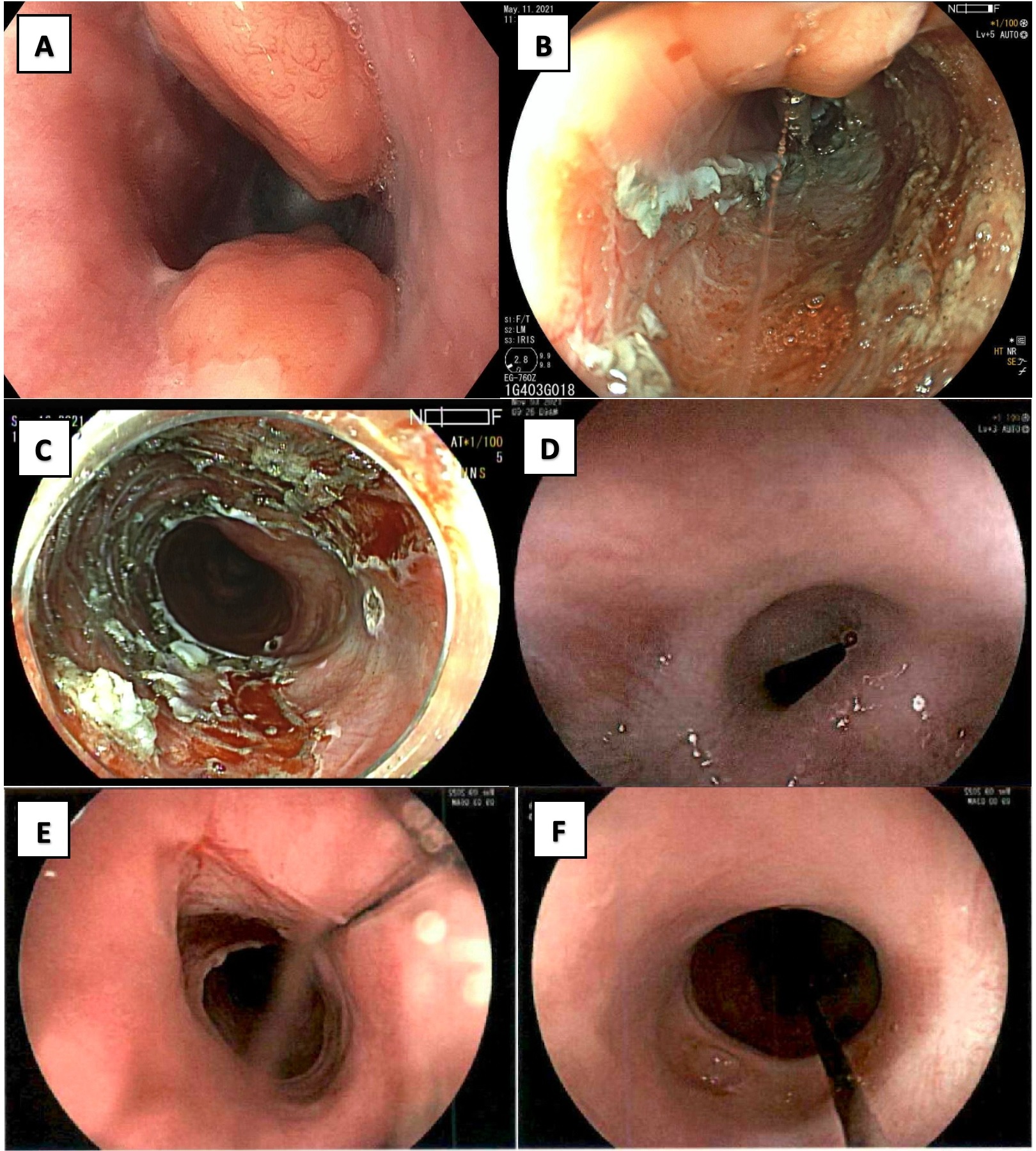
Figure: Figure 1. Endoscopic appearance of the two upper esophageal subepithelial lesions (panel A). Endoscopic submucosal dissection (ESD) was performed in two separate sessions (panels B and C). Benign-appearing post-ESD stricture before (panel D) and after dilation (panels E and F). Patient remains asymptomatic 3 months after last stricture dilation.
Disclosures:
Iris Lu indicated no relevant financial relationships.
Ahmad Al-Taee indicated no relevant financial relationships.
Gregory Haber indicated no relevant financial relationships.
Iris Lu, 1, Ahmad Al-Taee, MD2, Gregory Haber, MD3. E0462 - Symptomatic Ménétrier Disease of the Esophageal Inlet Patch Managed With Endoscopic Submucosal Dissection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
