Back
Poster Session C - Monday Afternoon
C0515 - Temporal Trends, Outcomes and Predictors of Mortality of Renal Replacement Therapy in Hepatorenal Syndrome Patients: Inpatient Analysis 2000-2019
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Maryam Haider, MD
Wayne State University/Detroit Medical Center Sinai Grace Hospital
Detroit, MI
Presenting Author(s)
Maryam Haider, MD1, Rawan Aljaras, MD2, Tooba Tariq, MD3, Hamidreza Moein, MD4, Paul Naylor, PhD5, Milton G. Mutchnick, MD5
1Wayne State University/Detroit Medical Center Sinai Grace Hospital, Detroit, MI; 2Indiana University School of Medicine, Indianapolis, IN; 3Wayne State University, Detroit, MI; 4Atrium Health Wake Forest Baptist Medical Center, Charlotte, NC; 5Wayne State University School of Medicine, Detroit, MI
Introduction: Hepatorenal syndrome (HRS) is a complication of end-stage renal failure. Liver transplantation (LT) remains the only definitive treatment for hepatorenal syndrome. The initiation of renal replacement therapy (RRT) in patients with HRS has extremely high mortality rates and has been utilized as a bridge to LT. We aimed to analyze temporal trends and outcomes of RRT in HRS patients.
Methods: The National Inpatient Sample (NIS) database from the year 2000 to 2019 was queried for patients to identify HRS patients using ICD codes. We used linear regression for continuous variables, the Cochran-Armitage Trend Test for categorical variables with two levels, and the Cochran-Mantel Haenszel Test for categorical variables with more than two levels. The p-values of < 0.01 were considered significant.
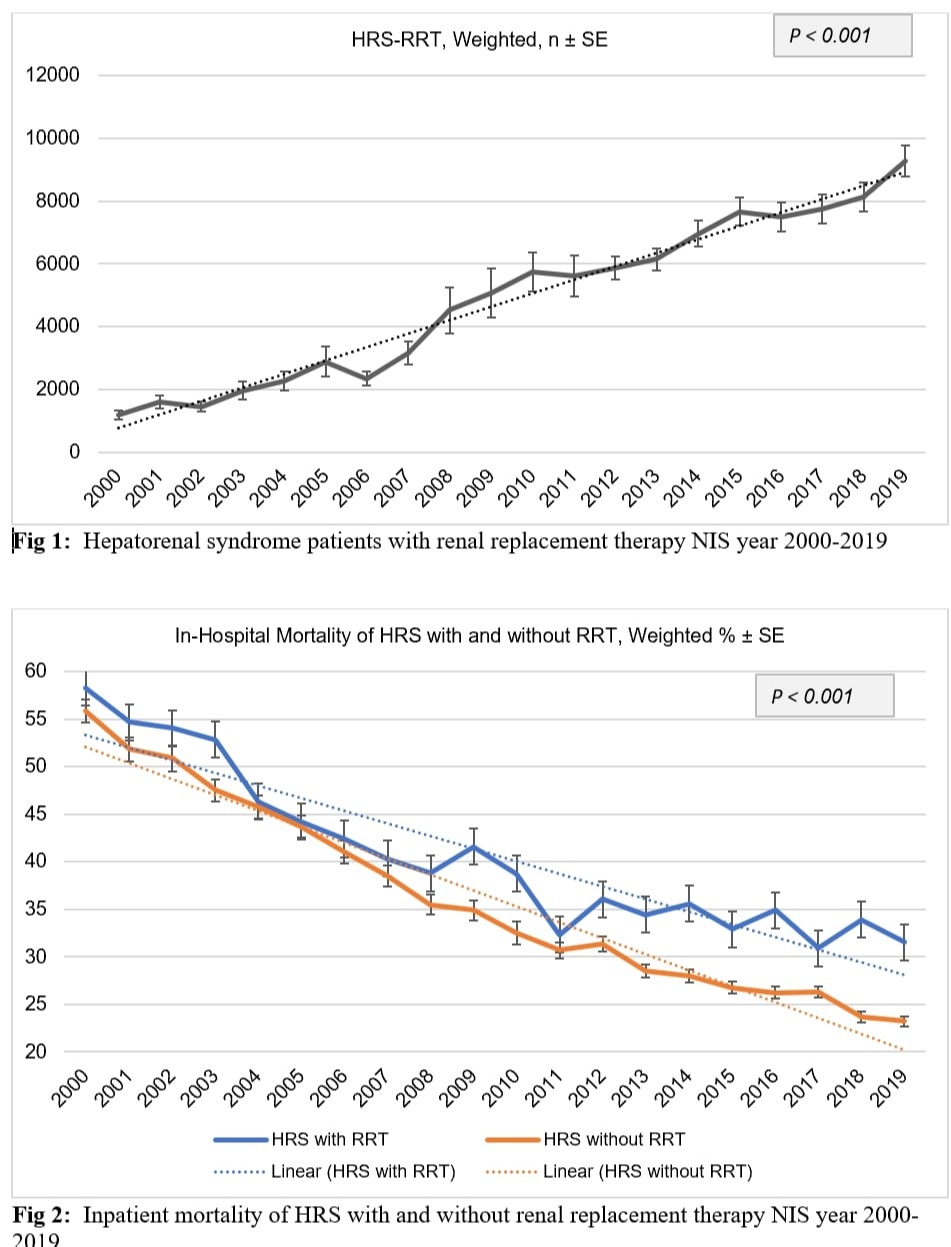
Results: We identified 518,464 patients with HRS, of which 97,037 (18.7%) underwent RRT. During 2000 to 2019, the weighted HRS-RRT prevalence increased from 11.2% to 19.9% with Ptrend < .0001. The mortality of HRS without RRT decreased from 55.9% to 23.2% Ptrend < .0001, and with RRT decreased from 58.3% to 31.5% Ptrend < .0001. The mortality of HRS-RRT female patients decreased from 50.5% to 29.1%, males from 62.4% to 33.1%, Caucasians (CAU) from 60.0% to 30.7%, African Americans (AA) from 65.1% to 33.9%, Hispanics (H) from 58.0% to 26.6%, and Asians from 60.1% to 36.2%, all with Ptrend < .0001. The multivariate analysis showed that older age (aOR:1.89; 99% CI, 1.18 – 3.03 ; P < .0001) for 85+, compared to 18-44, AA (aOR: 1.19; 99% CI, 1.03 – 1.37; P < .0001), compared to CAU, metastatic cancer (aOR: 1.87; 99% CI, 1.48 – 2.37; P < .0001), cerebrovascular disease (aOR: 1.66; 99% CI, 1.28 – 2.16; P < .0001) , CHF (aOR: 1.38; 99% CI, 1.24 – 1.55; P < .0001) , coagulopathy (aOR: 1.43; 99% CI, 1.31 – 1.56; P < .0001) , hypertension (aOR: 1.19; 99% CI, 1.04 – 1.37; P = 0.0010), seizures and epilepsy (aOR: 1.34; 99% CI, 1.09 – 1.65; P < .0001), and neurological disorders (aOR: 1.51; 99% CI, 1.36 – 1.69; P < .0001) were correlated with higher in-hospital mortality.
Discussion: The mortality of HRS patients decreased over the last two decades. This may be explained by better ICU care and management and also by more access to LT and better post-transplant care during years. HRS patients with RRT showed higher mortality than those without RRT, possibly due to the severity of the disease in HRS-RRT cohort. Older age, male gender, AA and H race are risk factors for mortality in HRS patients going under RRT.
Disclosures:
Maryam Haider, MD1, Rawan Aljaras, MD2, Tooba Tariq, MD3, Hamidreza Moein, MD4, Paul Naylor, PhD5, Milton G. Mutchnick, MD5. C0515 - Temporal Trends, Outcomes and Predictors of Mortality of Renal Replacement Therapy in Hepatorenal Syndrome Patients: Inpatient Analysis 2000-2019, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Wayne State University/Detroit Medical Center Sinai Grace Hospital, Detroit, MI; 2Indiana University School of Medicine, Indianapolis, IN; 3Wayne State University, Detroit, MI; 4Atrium Health Wake Forest Baptist Medical Center, Charlotte, NC; 5Wayne State University School of Medicine, Detroit, MI
Introduction: Hepatorenal syndrome (HRS) is a complication of end-stage renal failure. Liver transplantation (LT) remains the only definitive treatment for hepatorenal syndrome. The initiation of renal replacement therapy (RRT) in patients with HRS has extremely high mortality rates and has been utilized as a bridge to LT. We aimed to analyze temporal trends and outcomes of RRT in HRS patients.
Methods: The National Inpatient Sample (NIS) database from the year 2000 to 2019 was queried for patients to identify HRS patients using ICD codes. We used linear regression for continuous variables, the Cochran-Armitage Trend Test for categorical variables with two levels, and the Cochran-Mantel Haenszel Test for categorical variables with more than two levels. The p-values of < 0.01 were considered significant.
Results: We identified 518,464 patients with HRS, of which 97,037 (18.7%) underwent RRT. During 2000 to 2019, the weighted HRS-RRT prevalence increased from 11.2% to 19.9% with Ptrend < .0001. The mortality of HRS without RRT decreased from 55.9% to 23.2% Ptrend < .0001, and with RRT decreased from 58.3% to 31.5% Ptrend < .0001. The mortality of HRS-RRT female patients decreased from 50.5% to 29.1%, males from 62.4% to 33.1%, Caucasians (CAU) from 60.0% to 30.7%, African Americans (AA) from 65.1% to 33.9%, Hispanics (H) from 58.0% to 26.6%, and Asians from 60.1% to 36.2%, all with Ptrend < .0001. The multivariate analysis showed that older age (aOR:1.89; 99% CI, 1.18 – 3.03 ; P < .0001) for 85+, compared to 18-44, AA (aOR: 1.19; 99% CI, 1.03 – 1.37; P < .0001), compared to CAU, metastatic cancer (aOR: 1.87; 99% CI, 1.48 – 2.37; P < .0001), cerebrovascular disease (aOR: 1.66; 99% CI, 1.28 – 2.16; P < .0001) , CHF (aOR: 1.38; 99% CI, 1.24 – 1.55; P < .0001) , coagulopathy (aOR: 1.43; 99% CI, 1.31 – 1.56; P < .0001) , hypertension (aOR: 1.19; 99% CI, 1.04 – 1.37; P = 0.0010), seizures and epilepsy (aOR: 1.34; 99% CI, 1.09 – 1.65; P < .0001), and neurological disorders (aOR: 1.51; 99% CI, 1.36 – 1.69; P < .0001) were correlated with higher in-hospital mortality.
Discussion: The mortality of HRS patients decreased over the last two decades. This may be explained by better ICU care and management and also by more access to LT and better post-transplant care during years. HRS patients with RRT showed higher mortality than those without RRT, possibly due to the severity of the disease in HRS-RRT cohort. Older age, male gender, AA and H race are risk factors for mortality in HRS patients going under RRT.
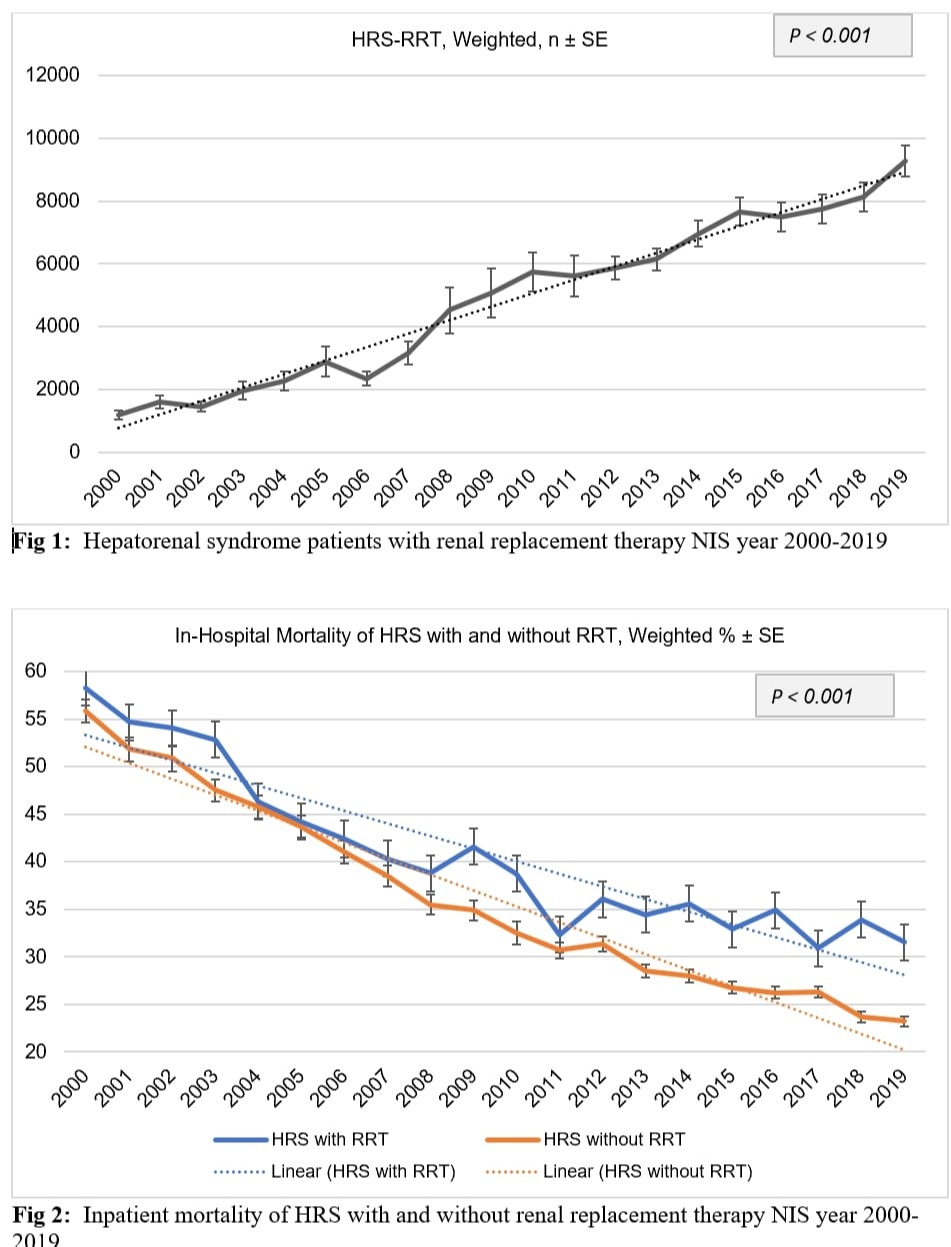
Figure: Weighted Hepatorenal syndrome patients with renal replacement therapy and Inpatient Mortality, NIS 2000 - 2019
Disclosures:
Maryam Haider indicated no relevant financial relationships.
Rawan Aljaras indicated no relevant financial relationships.
Tooba Tariq indicated no relevant financial relationships.
Hamidreza Moein indicated no relevant financial relationships.
Paul Naylor: Gilead Sciences – Grant/Research Support.
Milton Mutchnick: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau.
Maryam Haider, MD1, Rawan Aljaras, MD2, Tooba Tariq, MD3, Hamidreza Moein, MD4, Paul Naylor, PhD5, Milton G. Mutchnick, MD5. C0515 - Temporal Trends, Outcomes and Predictors of Mortality of Renal Replacement Therapy in Hepatorenal Syndrome Patients: Inpatient Analysis 2000-2019, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
