Back
Poster Session E - Tuesday Afternoon
E0599 - Tips for a Heartbreak: Hepatic Hydropericardium Improves After Transhepatic Portosystemic Shunt Placement
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Brendan Andres, MD
University of Arizona
Tucson, AZ
Presenting Author(s)
Brendan Andres, MD, Radhika Babaria, MD, Avin Aggarwal, MD
University of Arizona, Tucson, AZ
Introduction: Hepatic hydropericardium (HHP) has been observed as a complication of cirrhosis in patients with and without compensation. We present a case of HHP that improved after transhepatic portosystemic shunt (TIPS) placement in a patient with decompensated, non-alcoholic cirrhosis and constrictive cardiomyopathy (CCM) with a remote history of cardiac tamponade due to viral pericarditis.
Case Description/Methods: A 63-year-old-male with compensated non-alcoholic cirrhosis, obesity, chronic kidney disease, coronary artery disease, and CCM presented with abdominal distension and generalized anasarca despite high dose diuretics.
Abdomen and pelvis computerized tomography (CT) revealed large volume ascites, moderate anasarca, varices, splenomegaly and a 11.3 x 3.8 x 4.2 cm substernal fluid collection (Figure 1A). Transthoracic echocardiogram to further evaluate the fluid collection showed a 70 % left ventricular ejection fraction and a 2.8 cm loculated pericardial effusion (PE) with tamponade physiology. Emergent pericardiocentesis and paracentesis were performed. During the bubble study of the pericardiocentesis, translocation from the pericardial to the peritoneal space suggestive of a fistula was noted. Fluid studies were transudative and sterile with equal protein and albumin levels of 1.7 and 1.2 g/dL respectively.
The PE and ascites recurred (Figure 1B). CT chest again suggested a peritoneal-pericardial fistula. Two years prior, the patient had inflammatory pleural effusions and PE with cardiac tamponade due to viral pneumonia that completely resolved after drainage. Work up at that time revealed CCM on cardiac catheterization, and a pericardiectomy showing chronic inflammation and fibrosis was performed 4 months prior to the current admission.
Due to refractory ascites and PE with tamponade, the patient underwent TIPS placement. Subsequently, the patient had significant improvement in volume status and was discharged on daily furosemide 40 mg and spironolactone 25 mg. Follow up imaging revealed resolution of ascites and a non-tamponading 1.7 cm loculated PE.
Discussion: Our case illustrates HHP can be diagnosed via pericardiocentesis with bubble study and improves after TIPS. We hypothesize the patient developed a fistula after pericarditis or cardiothoracic surgery that led to HHP in the setting of portal hypertension via this tract, ultimately improving with TIPS. The HHP likely did not fully resolve due to loculation from PE chronicity and prior inflammation.
Disclosures:
Brendan Andres, MD, Radhika Babaria, MD, Avin Aggarwal, MD. E0599 - Tips for a Heartbreak: Hepatic Hydropericardium Improves After Transhepatic Portosystemic Shunt Placement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Arizona, Tucson, AZ
Introduction: Hepatic hydropericardium (HHP) has been observed as a complication of cirrhosis in patients with and without compensation. We present a case of HHP that improved after transhepatic portosystemic shunt (TIPS) placement in a patient with decompensated, non-alcoholic cirrhosis and constrictive cardiomyopathy (CCM) with a remote history of cardiac tamponade due to viral pericarditis.
Case Description/Methods: A 63-year-old-male with compensated non-alcoholic cirrhosis, obesity, chronic kidney disease, coronary artery disease, and CCM presented with abdominal distension and generalized anasarca despite high dose diuretics.
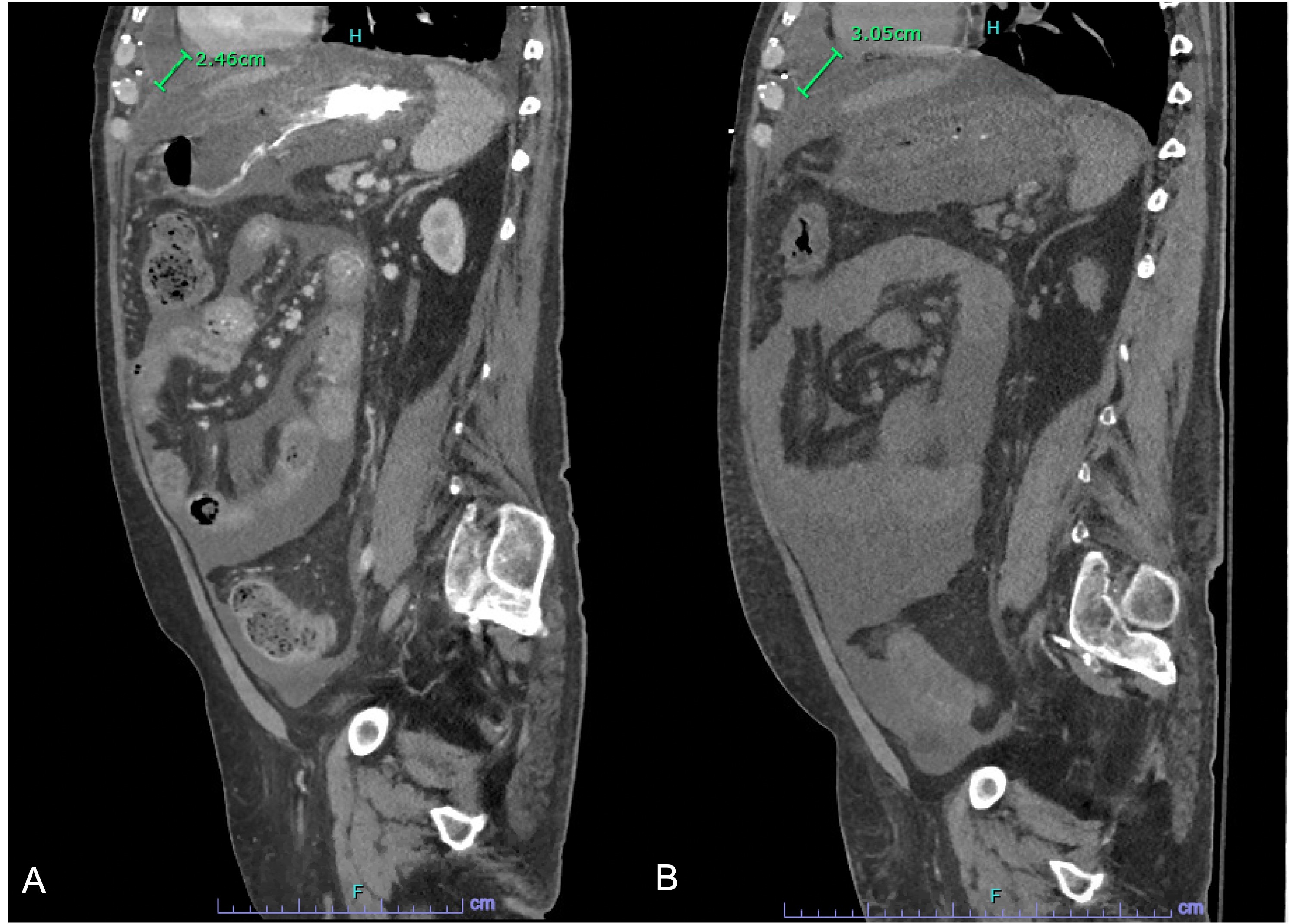
Abdomen and pelvis computerized tomography (CT) revealed large volume ascites, moderate anasarca, varices, splenomegaly and a 11.3 x 3.8 x 4.2 cm substernal fluid collection (Figure 1A). Transthoracic echocardiogram to further evaluate the fluid collection showed a 70 % left ventricular ejection fraction and a 2.8 cm loculated pericardial effusion (PE) with tamponade physiology. Emergent pericardiocentesis and paracentesis were performed. During the bubble study of the pericardiocentesis, translocation from the pericardial to the peritoneal space suggestive of a fistula was noted. Fluid studies were transudative and sterile with equal protein and albumin levels of 1.7 and 1.2 g/dL respectively.
The PE and ascites recurred (Figure 1B). CT chest again suggested a peritoneal-pericardial fistula. Two years prior, the patient had inflammatory pleural effusions and PE with cardiac tamponade due to viral pneumonia that completely resolved after drainage. Work up at that time revealed CCM on cardiac catheterization, and a pericardiectomy showing chronic inflammation and fibrosis was performed 4 months prior to the current admission.
Due to refractory ascites and PE with tamponade, the patient underwent TIPS placement. Subsequently, the patient had significant improvement in volume status and was discharged on daily furosemide 40 mg and spironolactone 25 mg. Follow up imaging revealed resolution of ascites and a non-tamponading 1.7 cm loculated PE.
Discussion: Our case illustrates HHP can be diagnosed via pericardiocentesis with bubble study and improves after TIPS. We hypothesize the patient developed a fistula after pericarditis or cardiothoracic surgery that led to HHP in the setting of portal hypertension via this tract, ultimately improving with TIPS. The HHP likely did not fully resolve due to loculation from PE chronicity and prior inflammation.
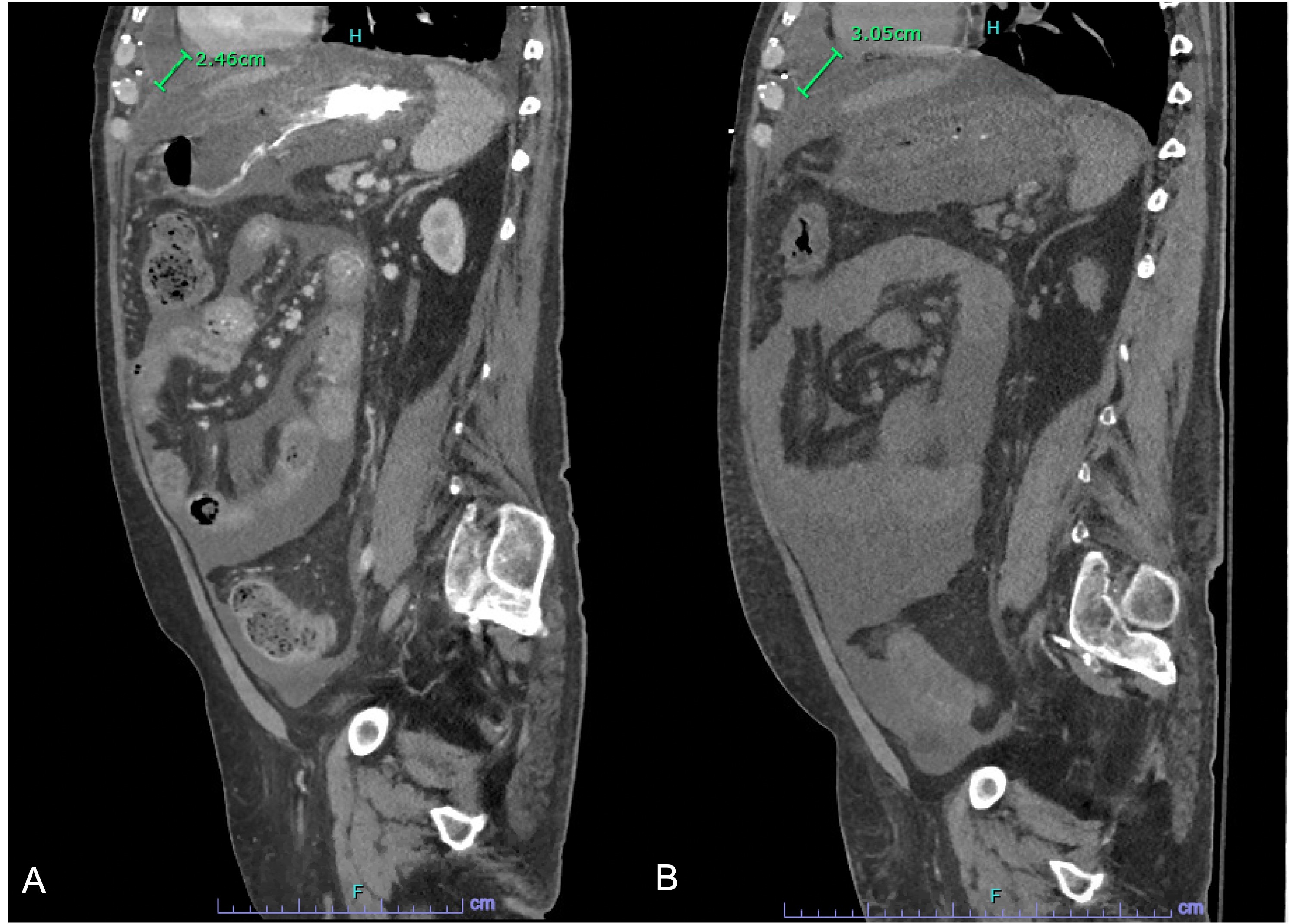
Figure: Figure 1. A) Sagittal CT demonstrating PE prior to pericardiocentesis. B) Sagittal CT demonstrating recurrence of PE after pericardiocentesis.
Disclosures:
Brendan Andres indicated no relevant financial relationships.
Radhika Babaria indicated no relevant financial relationships.
Avin Aggarwal indicated no relevant financial relationships.
Brendan Andres, MD, Radhika Babaria, MD, Avin Aggarwal, MD. E0599 - Tips for a Heartbreak: Hepatic Hydropericardium Improves After Transhepatic Portosystemic Shunt Placement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

