Back
Poster Session E - Tuesday Afternoon
E0497 - Appropriate Use of Ascitic Fluid Studies Among Inpatients With Ascites: A Quality Improvement Project
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
- SG
Srilaxmi Gujjula, MD
The Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Srilaxmi Gujjula, MD, Rajarajeshwari Ramachandran, MD, Suut Gokturk, MD, Praneeth Bandaru, MD, Vikash Kumar, MD, Isaac Giovannie, MD, Denzil Etienne, MD, Madhavi Reddy, MD
The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Ascites is the most common decompensating event in cirrhosis. Paracentesis is recommended in all patients with new-onset ascites, all patients admitted with ascites and all patients with ascites and signs or symptoms of infection. Standard of care tests from ascitic fluid include cell count with differential, total protein, albumin, and culture. In a limited number of patients, glucose, lactate dehydrogenase, cytology, amylase, pH, and bilirubin will be helpful. However, in clinical practice, a battery of ascitic fluid studies are commonly ordered. Many of these tests have no clinical impact and do not help guide management. Our initiative was to educate the residents enrolled in the internal medicine training program at The Brooklyn Hospital Center on appropriateness of ascitic fluid testing in patients admitted with ascites and improve the testing practices.
Methods: We provided an educational session focused on most recent guidelines on ascitic fluid tests to the residents enrolled in the internal medicine training program at The Brooklyn Hospital Center. Participants included residents first through third year of residency training. The educational session focused on appropriate use of ascitic fluid testing based on the most recent American Association for the Study of Liver Diseases (AASLD) guidelines. All participants completed a questionnaire testing the participant’s knowledge on appropriate use of ascitic fluid tests before and after the educational session.
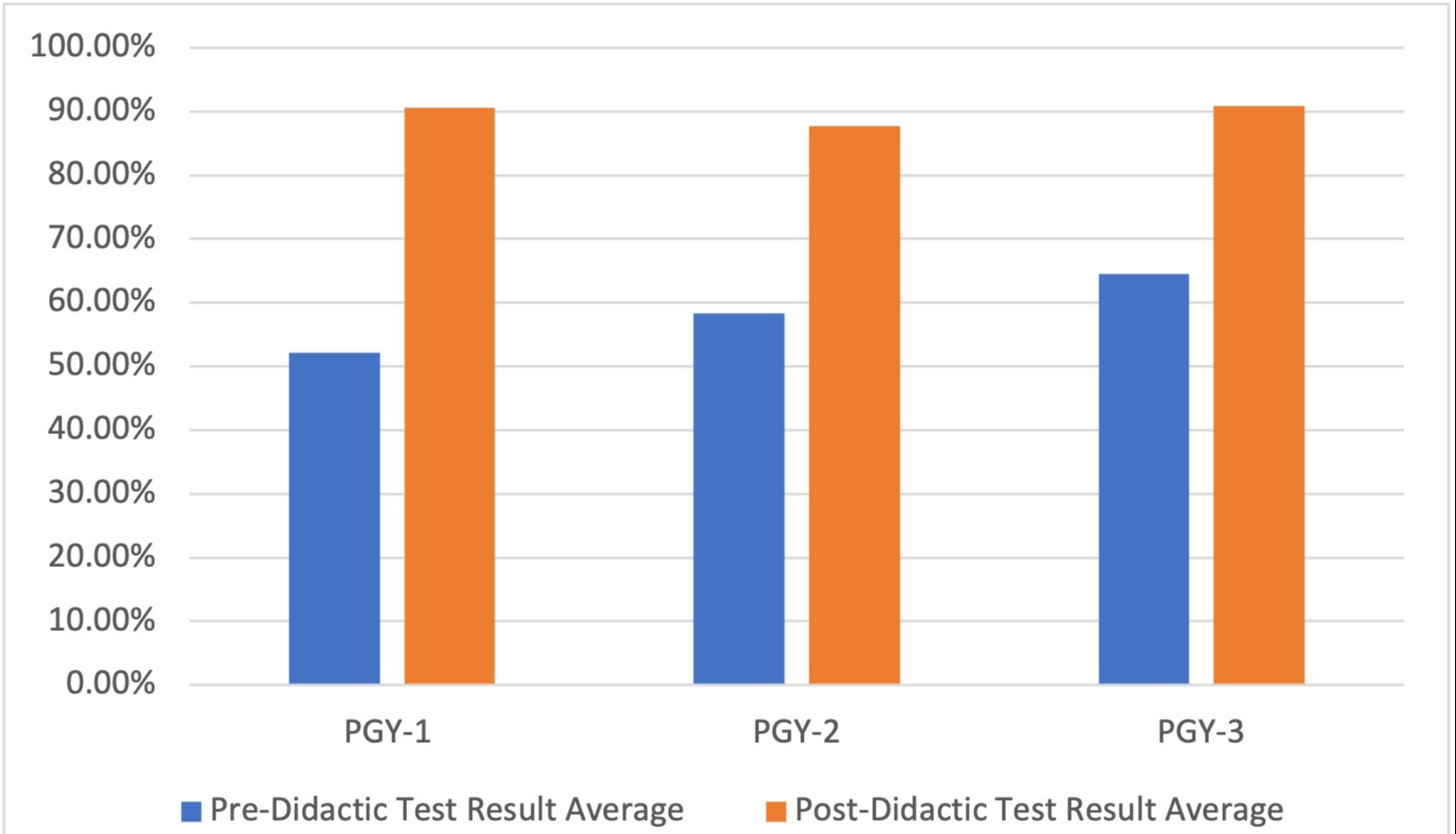
Results: Our results portray a significant improvement in the participants' understanding of the appropriate use of ascitic fluid tests after the educational session (figure 1). In the questionnaire completed before the educational session, post-graduate year 3 (PGY-3) participants scored the highest followed by PGY-2 and PGY-1 participants. After the educational session, there was increase in scores from all three category of participants with the highest improvement in the PGY-1 class (38.52%), followed by PGY-2 (29.32%) and PGY-3 participants (26.47%) (table 1).
Discussion: Ordering physician’s knowledge and education plays a key role in relevant use of ascitic fluid testing. Our study has demonstrated improved understanding of the appropriate use of ascitic fluid tests after our educational session. As a follow up, we plan on performing a retrospective chart review and post-intervention (post-educational session) chart review to monitor for improvement in the appropriate use of ascitic fluid testing.
Disclosures:
Srilaxmi Gujjula, MD, Rajarajeshwari Ramachandran, MD, Suut Gokturk, MD, Praneeth Bandaru, MD, Vikash Kumar, MD, Isaac Giovannie, MD, Denzil Etienne, MD, Madhavi Reddy, MD. E0497 - Appropriate Use of Ascitic Fluid Studies Among Inpatients With Ascites: A Quality Improvement Project, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Ascites is the most common decompensating event in cirrhosis. Paracentesis is recommended in all patients with new-onset ascites, all patients admitted with ascites and all patients with ascites and signs or symptoms of infection. Standard of care tests from ascitic fluid include cell count with differential, total protein, albumin, and culture. In a limited number of patients, glucose, lactate dehydrogenase, cytology, amylase, pH, and bilirubin will be helpful. However, in clinical practice, a battery of ascitic fluid studies are commonly ordered. Many of these tests have no clinical impact and do not help guide management. Our initiative was to educate the residents enrolled in the internal medicine training program at The Brooklyn Hospital Center on appropriateness of ascitic fluid testing in patients admitted with ascites and improve the testing practices.
Methods: We provided an educational session focused on most recent guidelines on ascitic fluid tests to the residents enrolled in the internal medicine training program at The Brooklyn Hospital Center. Participants included residents first through third year of residency training. The educational session focused on appropriate use of ascitic fluid testing based on the most recent American Association for the Study of Liver Diseases (AASLD) guidelines. All participants completed a questionnaire testing the participant’s knowledge on appropriate use of ascitic fluid tests before and after the educational session.
Results: Our results portray a significant improvement in the participants' understanding of the appropriate use of ascitic fluid tests after the educational session (figure 1). In the questionnaire completed before the educational session, post-graduate year 3 (PGY-3) participants scored the highest followed by PGY-2 and PGY-1 participants. After the educational session, there was increase in scores from all three category of participants with the highest improvement in the PGY-1 class (38.52%), followed by PGY-2 (29.32%) and PGY-3 participants (26.47%) (table 1).
Discussion: Ordering physician’s knowledge and education plays a key role in relevant use of ascitic fluid testing. Our study has demonstrated improved understanding of the appropriate use of ascitic fluid tests after our educational session. As a follow up, we plan on performing a retrospective chart review and post-intervention (post-educational session) chart review to monitor for improvement in the appropriate use of ascitic fluid testing.
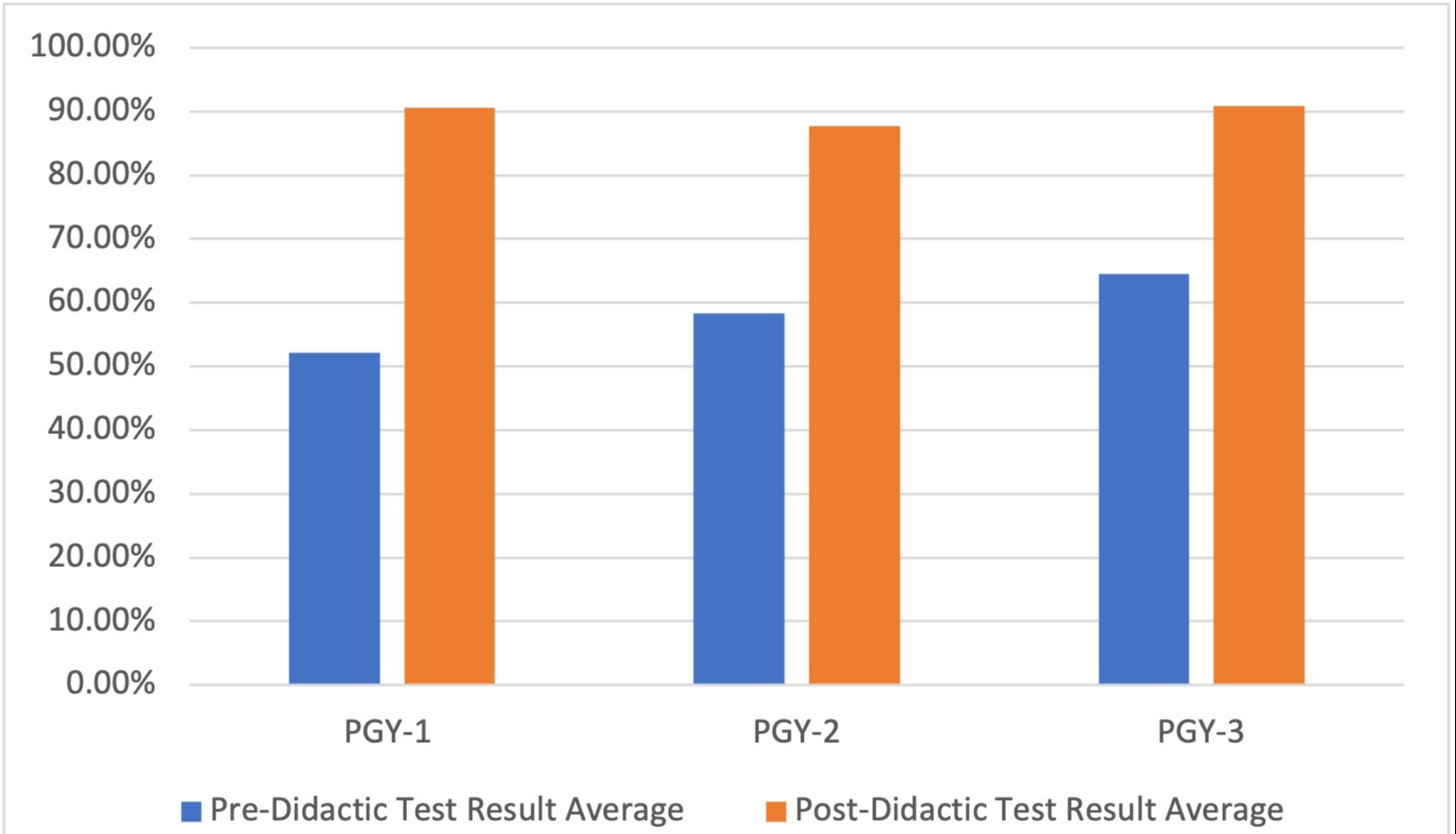
Figure: Figure 1: Results of Pre-Didactic and Post-Didactic Tests of all Classes
| Class | Pre-Didactic Test Result Average | Post-Didactic Test Result Average |
| PGY-1 | 52.08% | 90.60% |
| PGY-2 | 58.33% | 87.65% |
| PGY-3 | 64.44% | 90.91% |
Table: Table 1: Results of Pre-Didactic and Post-Didactic Tests of all Classes
Disclosures:
Srilaxmi Gujjula indicated no relevant financial relationships.
Rajarajeshwari Ramachandran indicated no relevant financial relationships.
Suut Gokturk indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Isaac Giovannie indicated no relevant financial relationships.
Denzil Etienne indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Srilaxmi Gujjula, MD, Rajarajeshwari Ramachandran, MD, Suut Gokturk, MD, Praneeth Bandaru, MD, Vikash Kumar, MD, Isaac Giovannie, MD, Denzil Etienne, MD, Madhavi Reddy, MD. E0497 - Appropriate Use of Ascitic Fluid Studies Among Inpatients With Ascites: A Quality Improvement Project, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
