Back
Poster Session A - Sunday Afternoon
A0400 - Secukinumab-Induced Crohn’s Disease Complicated by Hemorrhagic Shock in a Patient Undergoing Treatment for Chronic Plaque Psoriasis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Pranay Reddy, MD, MPH
Jefferson Health Northeast
Philadelphia, PA
Presenting Author(s)
Pranay Reddy, MD, MPH1, Bryan Stone, DO2, Patricia Wong, MD3, Rachael Schneider, DO4, Walter M. Klein, MD2
1Jefferson Health Northeast, Philadelphia, PA; 2Lankenau Medical Center / Main Line Health, Wynnewood, PA; 3Lankenau Medical Center, Philadelphia, PA; 4Lankenau Medical Center, Wynnewood, PA
Introduction: Secukinumab is a human monoclonal antibody which inhibits the proinflammatory cytokine interleukin-17A (IL-17A). It is used to treat chronic plaque psoriasis, ankylosing spondylitis, and psoriatic arthritis. Over the past several years, it has been increasingly linked to exacerbations of pre-existing inflammatory bowel disease (IBD) as well as development of new onset IBD, including both ulcerative colitis and Crohn’s disease (CD). We present an 83-year-old patient on Secukinumab for psoriasis who presented with chronic diarrhea complicated by GI hemorrhage and was diagnosed with new onset CD.
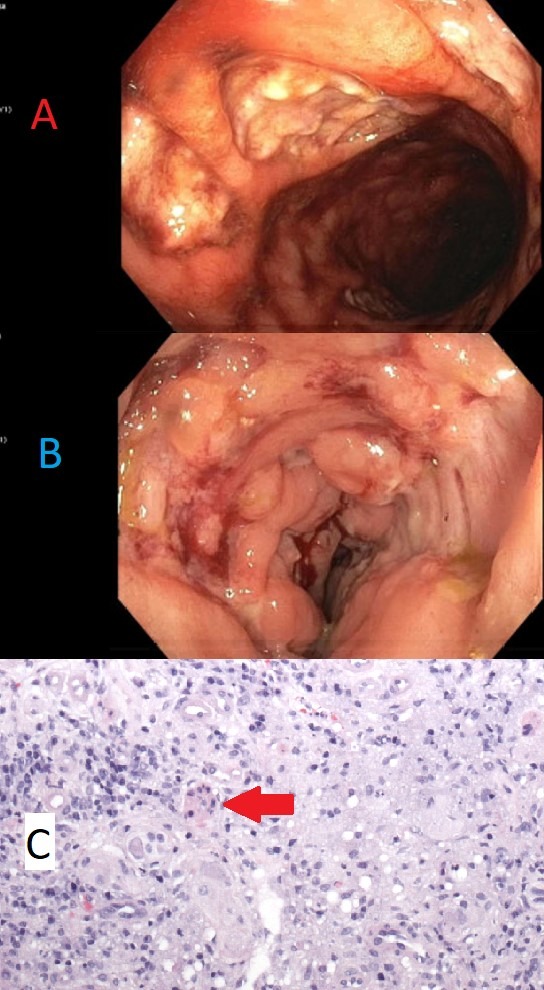
Case Description/Methods: An 83-year-old male with a past medical history of CAD, CKD and psoriasis presented with four weeks of diarrhea. He denied recent antibiotic use, travel, sick contacts or history of IBD, however endorsed initiation of Secukinumab prior to symptom onset. He reported distant ileocecectomy twenty years prior for unknown reasons. Labs remarkable for iron deficiency anemia (iron sat 3%), CRP 86 mg/dl and fecal calprotectin 1860 ug/g. CT scan revealed new ileal wall thickening with a normal appearing colon. Colonoscopy showed deep ulcers in the rectum and terminal ileum associated with mucus and friable mucosa. Biopsies revealed severe active ileitis with ulceration and rare epithelioid granulomas concerning for CD. He was started on high dose IV steroids but continued to have worsening diarrhea for 7 days. His course was further complicated by large volume hematochezia, hemorrhagic shock requiring 15 units of packed red blood cells, and acute kidney injury. Repeat colonoscopies demonstrated deep rectal ulcerations and oozing from the ileum. He was started on IV Remicade due to refractory symptoms but ultimately had significant clinical improvement and was discharged.
Discussion: There have been several case reports of Secukinumab-induced IBD. The exact mechanism is unknown but may involve shunting of the immunologic pathway from blockade of IL-17 which results in increased stimulation of an alternative pathway. It remains unclear whether new onset IBD associated with Secukinumab is a chronic condition or resolves with discontinuation of Secukinumab. This case demonstrates Secukinumab-induced CD and is the first case report of severe GI hemorrhage requiring massive transfusion protocol. When starting patients on Secukinumab therapy, it is important to advise them of the potential complication of new onset IBD and the complications associated with IBD including intestinal hemorrhage.
Disclosures:
Pranay Reddy, MD, MPH1, Bryan Stone, DO2, Patricia Wong, MD3, Rachael Schneider, DO4, Walter M. Klein, MD2. A0400 - Secukinumab-Induced Crohn’s Disease Complicated by Hemorrhagic Shock in a Patient Undergoing Treatment for Chronic Plaque Psoriasis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Jefferson Health Northeast, Philadelphia, PA; 2Lankenau Medical Center / Main Line Health, Wynnewood, PA; 3Lankenau Medical Center, Philadelphia, PA; 4Lankenau Medical Center, Wynnewood, PA
Introduction: Secukinumab is a human monoclonal antibody which inhibits the proinflammatory cytokine interleukin-17A (IL-17A). It is used to treat chronic plaque psoriasis, ankylosing spondylitis, and psoriatic arthritis. Over the past several years, it has been increasingly linked to exacerbations of pre-existing inflammatory bowel disease (IBD) as well as development of new onset IBD, including both ulcerative colitis and Crohn’s disease (CD). We present an 83-year-old patient on Secukinumab for psoriasis who presented with chronic diarrhea complicated by GI hemorrhage and was diagnosed with new onset CD.
Case Description/Methods: An 83-year-old male with a past medical history of CAD, CKD and psoriasis presented with four weeks of diarrhea. He denied recent antibiotic use, travel, sick contacts or history of IBD, however endorsed initiation of Secukinumab prior to symptom onset. He reported distant ileocecectomy twenty years prior for unknown reasons. Labs remarkable for iron deficiency anemia (iron sat 3%), CRP 86 mg/dl and fecal calprotectin 1860 ug/g. CT scan revealed new ileal wall thickening with a normal appearing colon. Colonoscopy showed deep ulcers in the rectum and terminal ileum associated with mucus and friable mucosa. Biopsies revealed severe active ileitis with ulceration and rare epithelioid granulomas concerning for CD. He was started on high dose IV steroids but continued to have worsening diarrhea for 7 days. His course was further complicated by large volume hematochezia, hemorrhagic shock requiring 15 units of packed red blood cells, and acute kidney injury. Repeat colonoscopies demonstrated deep rectal ulcerations and oozing from the ileum. He was started on IV Remicade due to refractory symptoms but ultimately had significant clinical improvement and was discharged.
Discussion: There have been several case reports of Secukinumab-induced IBD. The exact mechanism is unknown but may involve shunting of the immunologic pathway from blockade of IL-17 which results in increased stimulation of an alternative pathway. It remains unclear whether new onset IBD associated with Secukinumab is a chronic condition or resolves with discontinuation of Secukinumab. This case demonstrates Secukinumab-induced CD and is the first case report of severe GI hemorrhage requiring massive transfusion protocol. When starting patients on Secukinumab therapy, it is important to advise them of the potential complication of new onset IBD and the complications associated with IBD including intestinal hemorrhage.
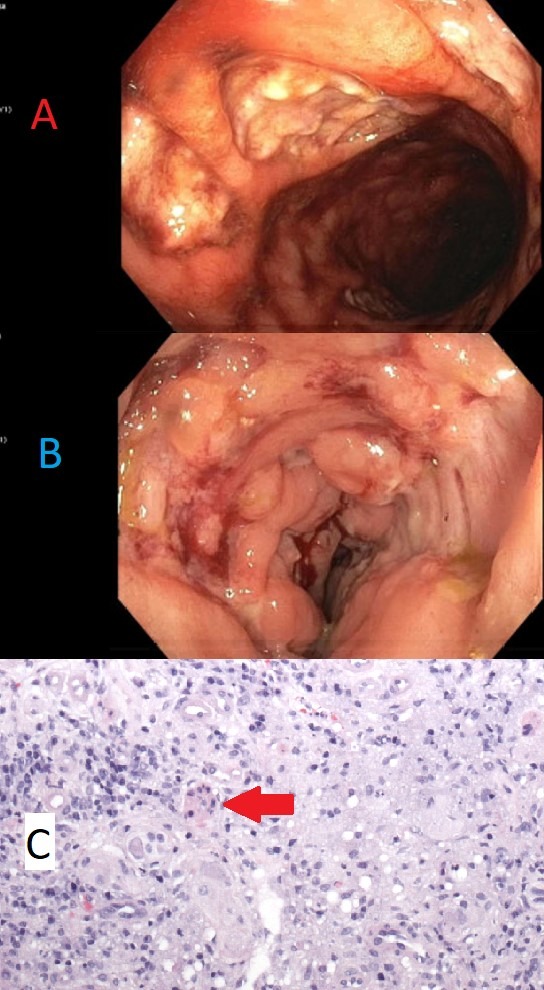
Figure: A. Large, nonbleeding deep ulcerations in rectum with surrounding friable mucosa
B. Oozing terminal ileum ulcerations with associated mucus and friable mucosa
C. Chronic, active granulomatous inflammation with a cluster of histiocytes surrounded by lymphocytes and plasma cells (indicated by red arrow).
B. Oozing terminal ileum ulcerations with associated mucus and friable mucosa
C. Chronic, active granulomatous inflammation with a cluster of histiocytes surrounded by lymphocytes and plasma cells (indicated by red arrow).
Disclosures:
Pranay Reddy indicated no relevant financial relationships.
Bryan Stone indicated no relevant financial relationships.
Patricia Wong indicated no relevant financial relationships.
Rachael Schneider indicated no relevant financial relationships.
Walter Klein indicated no relevant financial relationships.
Pranay Reddy, MD, MPH1, Bryan Stone, DO2, Patricia Wong, MD3, Rachael Schneider, DO4, Walter M. Klein, MD2. A0400 - Secukinumab-Induced Crohn’s Disease Complicated by Hemorrhagic Shock in a Patient Undergoing Treatment for Chronic Plaque Psoriasis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
