Back
Poster Session E - Tuesday Afternoon
E0365 - Venous Thromboembolism in the Setting of Inflammatory Bowel Disease: A Multi-Centric Retrospective Analysis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Garvit Chhabra, MD
University of Louisville
Louisville, KY
Presenting Author(s)
Garvit Chhabra, MD, Anuja Abhyankar, MD, Michael Eiswerth, DO, Freeha Khan, MD, Robert Luckett, MD, Gerald Dryden, MD
University of Louisville, Louisville, KY
Introduction: Inflammatory bowel disease (IBD) is a systemic inflammatory condition with an increased risk of venous thromboembolism (VTE). The most common sites include deep veins of lower extremities and pulmonary vasculature, and rarely cerebrovascular veins which can significantly increase morbidity and mortality. While the higher incidence of VTE in IBD has been well established, standardized risk assessment models for VTE do not consider the presence of IBD as a high-risk factor.
Methods: A retrospective chart review of 261 randomly selected patients with IBD over the last 5 years was performed. Patients with an incidence of VTE in the last 5 years (2017-2022) were identified. Baseline characteristics, site of VTE, use of anticoagulation for VTE prophylaxis, and anticoagulant used were collected. Descriptive statistics were used to analyze the incidence of VTE and the percentage of patients on anticoagulation.
Results: The 5-year incidence of VTE in the studied 259 patients was 13.51% (35) of which 11.2% (29) had DVT, 3.5% (9) had both DVT and PE, and 2.3% (6) had only PE. The average age of the patients with VTE was 57.4 ± 12.3 years; 37% (13) were men and 63% (22) were women; 66% (23) were Caucasian, 31% (11) were African American, and 3% (1) were Pacific-islander. Of the 259 patients, 133 (51.4%) received VTE prophylaxis during hospitalizations, while 126 (48.6%) did not. Of the patients who received prophylaxis, the incidence of VTE was 4.5% (6 of 133) whereas the incidence was 23% (29 of 126) in those who did not receive VTE prophylaxis.
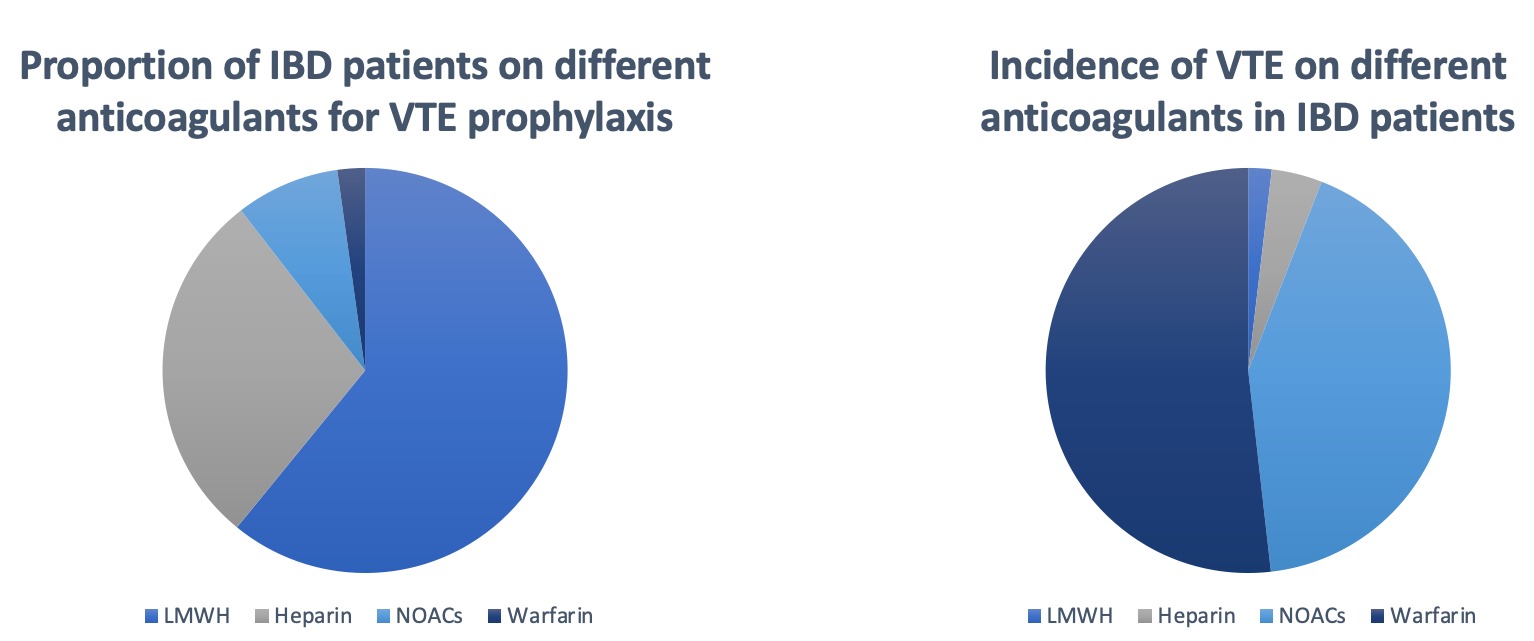
Of the 133 patients who were on anticoagulation, 11 were on NOACs (8.3%), 38 were on heparin (28.6%), 81 were on LMWH (60.9%), and 3 were on warfarin (2.2%). Of the 6 patients who had an incidence of VTE on anticoagulation, 3 were on NOACs, 1 was on heparin, 1 was on LMWH, and 1 was on warfarin.
Discussion: Being a chronic inflammatory state, IBD is associated with a 2-3 times higher incidence of VTE. However, multiple factors exist in both the pathophysiology and treatment of the disease that may contribute to the development of VTE. Numerous factors such as surgeries, use of steroids, and gender have been implicated in increasing the risk for VTE. There is a wide scope for further research regarding the same. Despite conclusive evidence, at most centers, the presence of IBD is not considered to be a high-risk factor for VTE warranting anticoagulation. Awareness and education are the cornerstones to cause a momentous change in practice patterns.
Disclosures:
Garvit Chhabra, MD, Anuja Abhyankar, MD, Michael Eiswerth, DO, Freeha Khan, MD, Robert Luckett, MD, Gerald Dryden, MD. E0365 - Venous Thromboembolism in the Setting of Inflammatory Bowel Disease: A Multi-Centric Retrospective Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Louisville, Louisville, KY
Introduction: Inflammatory bowel disease (IBD) is a systemic inflammatory condition with an increased risk of venous thromboembolism (VTE). The most common sites include deep veins of lower extremities and pulmonary vasculature, and rarely cerebrovascular veins which can significantly increase morbidity and mortality. While the higher incidence of VTE in IBD has been well established, standardized risk assessment models for VTE do not consider the presence of IBD as a high-risk factor.
Methods: A retrospective chart review of 261 randomly selected patients with IBD over the last 5 years was performed. Patients with an incidence of VTE in the last 5 years (2017-2022) were identified. Baseline characteristics, site of VTE, use of anticoagulation for VTE prophylaxis, and anticoagulant used were collected. Descriptive statistics were used to analyze the incidence of VTE and the percentage of patients on anticoagulation.
Results: The 5-year incidence of VTE in the studied 259 patients was 13.51% (35) of which 11.2% (29) had DVT, 3.5% (9) had both DVT and PE, and 2.3% (6) had only PE. The average age of the patients with VTE was 57.4 ± 12.3 years; 37% (13) were men and 63% (22) were women; 66% (23) were Caucasian, 31% (11) were African American, and 3% (1) were Pacific-islander. Of the 259 patients, 133 (51.4%) received VTE prophylaxis during hospitalizations, while 126 (48.6%) did not. Of the patients who received prophylaxis, the incidence of VTE was 4.5% (6 of 133) whereas the incidence was 23% (29 of 126) in those who did not receive VTE prophylaxis.
Of the 133 patients who were on anticoagulation, 11 were on NOACs (8.3%), 38 were on heparin (28.6%), 81 were on LMWH (60.9%), and 3 were on warfarin (2.2%). Of the 6 patients who had an incidence of VTE on anticoagulation, 3 were on NOACs, 1 was on heparin, 1 was on LMWH, and 1 was on warfarin.
Discussion: Being a chronic inflammatory state, IBD is associated with a 2-3 times higher incidence of VTE. However, multiple factors exist in both the pathophysiology and treatment of the disease that may contribute to the development of VTE. Numerous factors such as surgeries, use of steroids, and gender have been implicated in increasing the risk for VTE. There is a wide scope for further research regarding the same. Despite conclusive evidence, at most centers, the presence of IBD is not considered to be a high-risk factor for VTE warranting anticoagulation. Awareness and education are the cornerstones to cause a momentous change in practice patterns.
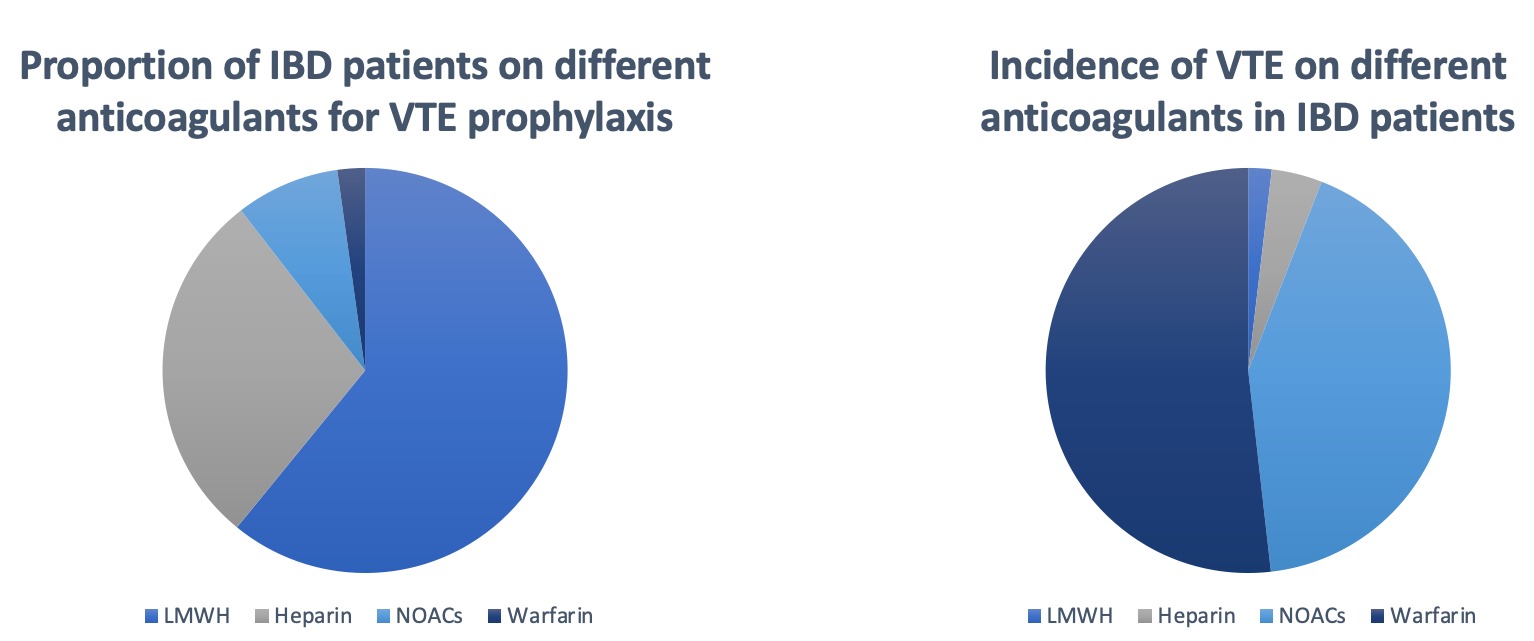
Figure: Proportion of IBD patients on different anticoagulants and the incidence of VTE while on them
Disclosures:
Garvit Chhabra indicated no relevant financial relationships.
Anuja Abhyankar indicated no relevant financial relationships.
Michael Eiswerth indicated no relevant financial relationships.
Freeha Khan indicated no relevant financial relationships.
Robert Luckett indicated no relevant financial relationships.
Gerald Dryden indicated no relevant financial relationships.
Garvit Chhabra, MD, Anuja Abhyankar, MD, Michael Eiswerth, DO, Freeha Khan, MD, Robert Luckett, MD, Gerald Dryden, MD. E0365 - Venous Thromboembolism in the Setting of Inflammatory Bowel Disease: A Multi-Centric Retrospective Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
