Back
Poster Session E - Tuesday Afternoon
E0457 - A Case for Endoscopic Ultrasound-Directed TransGastric ERCP (EDGE) Procedure: Removal of Choledocholithiasis in Gastric Bypass Patient
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Yash P. Ashara, MBBS
BJMC
Rochester, MN
Presenting Author(s)
Yash Ashara, MBBS1, Bhavtosh Dedania, MD2, Rahman Nakshabendi, MD3, Shaina Grego, PA-C, MPAS2
1BJMC, Rochester, MN; 2Florida Digestive Health Specialist, Brandon, FL; 3Florida Advanced Gastroenterology Center, Brandon, FL
Introduction: Due to rise in obesity, there has been an increased number of gastric bypass surgeries. Around 36% morbidly obese patient develop cholelithiasis or choledocholithiasis (CDL) in their lifetime. Due to the anatomy, a conventional Endoscopic Retrograde Cholangio Pancreatography (ERCP) is often challenging and not possible. We present a case of an altered anatomy ERCP in a patient with CDL and Roux-en-Y gastric bypass (RYGB) who underwent Endoscopic ultrasound Directed trans-Gastric ERCP(EDGE) procedure.
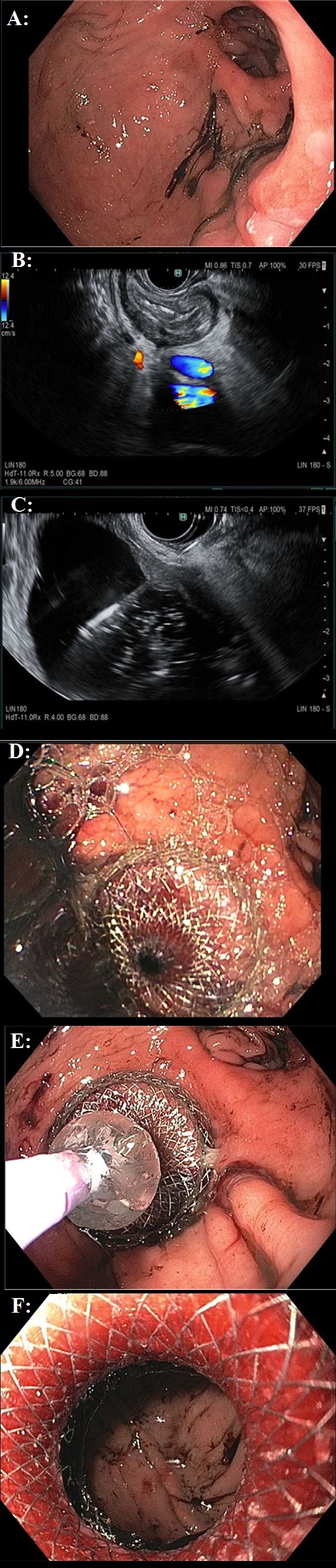
Case Description/Methods: A 69-year-old female with a history of RYGB admitted for Hartmann’s procedure. During the hospitalization, she complained of RUQ pain and CT abdomen showed a distended gallbladder with cholelithiasis and CBD dilation of 8.3mm; MRCP confirmed five or more CDL. A traditional attempt at an ERCP using a pediatric colonoscope was unsuccessful in reaching the papilla. She underwent cholecystectomy with an intraoperative cholangiogram re-demonstrating the CDL. Options were to do a laparoscopy assisted ERCP v/s double balloon assisted ERCP v/s EDGE. Due to already multiple surgeries patient opted for EDGE procedure. For stage 1 of the EDGE, the excluded stomach was identified under EUS and punctured using a 19-gauge-needle followed by a radiocontrast dye injection into the excluded stomach confirmed under fluoroscopy. Subsequently, a guidewire was advanced through the needle into the pylorus and duodenum to verify the patency of pylorus. After confirming access to the excluded stomach, a 20 x 10 mm (AXIOSTM) lumen apposing metal stent (LAMS) was placed and a gastro-gastric fistula between the gastric pouch and the excluded stomach was formed. The lumen of the stent was subsequently dilated using a CRE balloon confirming the direct visualization of the gastric rugae. (Figure). The LAMS was left for 4 weeks for the tract to mature. Stage 2 of the EDGE procedure was then completed by passing the duodenoscope through the LAMS and completion of the traditional ERCP followed by removal of the LAMS. Overall patient did well.
Discussion: EDGE is a minimally invasive EUS guided technique for doing an ERCP in patients with RYGB. Comparison studies have shown EDGE to have similar or better technical success when compared to laparoscopy-assisted ERCP and balloon Enteroscopy-assisted ERCP. Due to the high technical skill required in doing an EDGE, it is best advisable to offer this at institutions where a trained advanced endoscopist well versed with a therapeutic EUS is available.
Disclosures:
Yash Ashara, MBBS1, Bhavtosh Dedania, MD2, Rahman Nakshabendi, MD3, Shaina Grego, PA-C, MPAS2. E0457 - A Case for Endoscopic Ultrasound-Directed TransGastric ERCP (EDGE) Procedure: Removal of Choledocholithiasis in Gastric Bypass Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1BJMC, Rochester, MN; 2Florida Digestive Health Specialist, Brandon, FL; 3Florida Advanced Gastroenterology Center, Brandon, FL
Introduction: Due to rise in obesity, there has been an increased number of gastric bypass surgeries. Around 36% morbidly obese patient develop cholelithiasis or choledocholithiasis (CDL) in their lifetime. Due to the anatomy, a conventional Endoscopic Retrograde Cholangio Pancreatography (ERCP) is often challenging and not possible. We present a case of an altered anatomy ERCP in a patient with CDL and Roux-en-Y gastric bypass (RYGB) who underwent Endoscopic ultrasound Directed trans-Gastric ERCP(EDGE) procedure.
Case Description/Methods: A 69-year-old female with a history of RYGB admitted for Hartmann’s procedure. During the hospitalization, she complained of RUQ pain and CT abdomen showed a distended gallbladder with cholelithiasis and CBD dilation of 8.3mm; MRCP confirmed five or more CDL. A traditional attempt at an ERCP using a pediatric colonoscope was unsuccessful in reaching the papilla. She underwent cholecystectomy with an intraoperative cholangiogram re-demonstrating the CDL. Options were to do a laparoscopy assisted ERCP v/s double balloon assisted ERCP v/s EDGE. Due to already multiple surgeries patient opted for EDGE procedure. For stage 1 of the EDGE, the excluded stomach was identified under EUS and punctured using a 19-gauge-needle followed by a radiocontrast dye injection into the excluded stomach confirmed under fluoroscopy. Subsequently, a guidewire was advanced through the needle into the pylorus and duodenum to verify the patency of pylorus. After confirming access to the excluded stomach, a 20 x 10 mm (AXIOSTM) lumen apposing metal stent (LAMS) was placed and a gastro-gastric fistula between the gastric pouch and the excluded stomach was formed. The lumen of the stent was subsequently dilated using a CRE balloon confirming the direct visualization of the gastric rugae. (Figure). The LAMS was left for 4 weeks for the tract to mature. Stage 2 of the EDGE procedure was then completed by passing the duodenoscope through the LAMS and completion of the traditional ERCP followed by removal of the LAMS. Overall patient did well.
Discussion: EDGE is a minimally invasive EUS guided technique for doing an ERCP in patients with RYGB. Comparison studies have shown EDGE to have similar or better technical success when compared to laparoscopy-assisted ERCP and balloon Enteroscopy-assisted ERCP. Due to the high technical skill required in doing an EDGE, it is best advisable to offer this at institutions where a trained advanced endoscopist well versed with a therapeutic EUS is available.
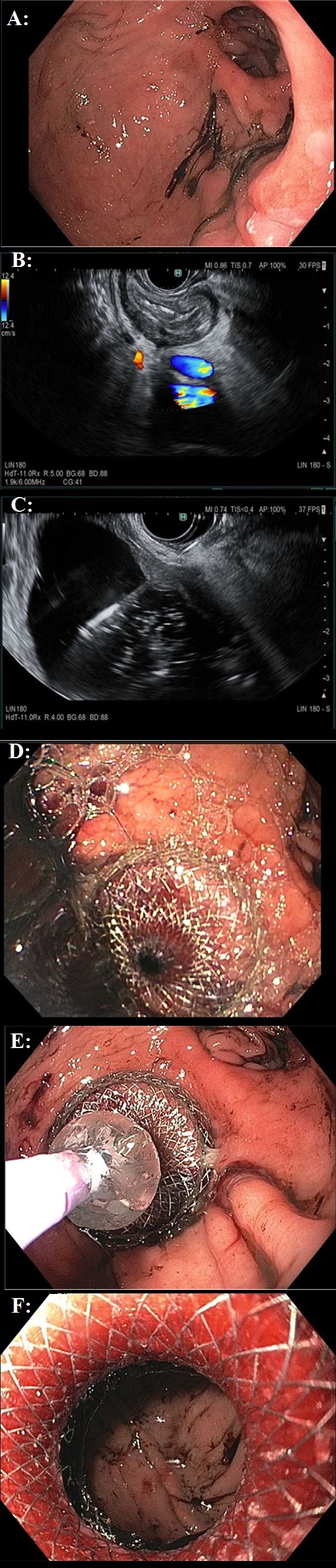
Figure: A: EGD showing gastric pouch post-RYGB
B: EUS suggests decompressed excluded stomach
C: Injecting contrast into the excluded stomach - to make cystic cavity
D: 20 x 10 mm(AXIOS) lumen apposing metal stent placement
E: CRE Baloon dilation of LAMS
F: Confirmed visualization of excluded gastric mucosa - gastrogastric fistula
B: EUS suggests decompressed excluded stomach
C: Injecting contrast into the excluded stomach - to make cystic cavity
D: 20 x 10 mm(AXIOS) lumen apposing metal stent placement
E: CRE Baloon dilation of LAMS
F: Confirmed visualization of excluded gastric mucosa - gastrogastric fistula
Disclosures:
Yash Ashara indicated no relevant financial relationships.
Bhavtosh Dedania indicated no relevant financial relationships.
Rahman Nakshabendi indicated no relevant financial relationships.
Shaina Grego indicated no relevant financial relationships.
Yash Ashara, MBBS1, Bhavtosh Dedania, MD2, Rahman Nakshabendi, MD3, Shaina Grego, PA-C, MPAS2. E0457 - A Case for Endoscopic Ultrasound-Directed TransGastric ERCP (EDGE) Procedure: Removal of Choledocholithiasis in Gastric Bypass Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
