Back
Poster Session E - Tuesday Afternoon
E0449 - Diverting Disaster: EUS-Guided Trans-Gastric Biliary Drainage
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
.jpg)
Asad Rehman, DO
HCA West Florida Largo Medical Center
Largo, FL
Presenting Author(s)
Asad Rehman, DO1, Vikas Sethi, DO2, Geoffrey Goldsberry, DO1, Joseph Namey, DO2, Muhammad Khan, MD, MPH1, Meir Mizrahi, MD1
1HCA West Florida Largo Medical Center, Largo, FL; 2Largo Medical Center, Largo, FL
Introduction: Lumen-apposing metal stents (LAMS) are a relatively new intervention that can be used for high risk surgical cases, such as malignant obstructions not amenable to ERCP. There are few case reports using LAMS with Endoscopic Ultrasound (EUS) to achieve drainage and palliative therapy in these situations, especially using a gastric over duodenal approach. In this case, we add to the growing body of literature supporting a transgastric approach for biliary drainage using LAMS.
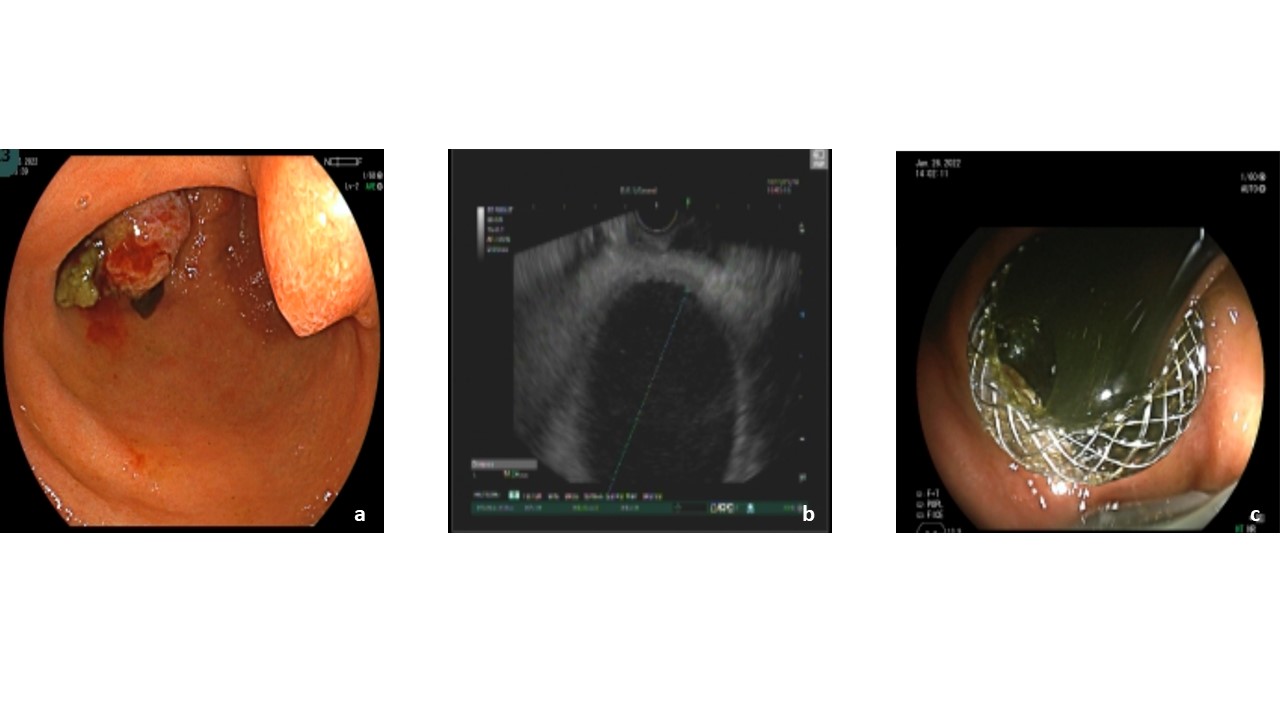
Case Description/Methods: A 73 year-old male was admitted due to concerns for obstructive jaundice. He presented with pruritis, nausea, vomiting, copious nasogastric tube bilious output and a total bilirubin of 19.8mg/dL. MRCP revealed a distal CBD stricture measuring 12 mm in length, marked intrahepatic and extrahepatic biliary dilatation and an 8mm dilated pancreatic duct. EGD revealed a submucosal mass within the duodenal bulb causing gallbladder impingement (a). EUS was then completed and revealed similar findings to MRCP including an atrophic pancreas and severely dilated gallbladder (b). The ampullary mass, noted on CT, was also identified under EUS and fine needle biopsy was performed. A 10mm x 10mm LAMS was placed under endoscopic and fluoroscopic visualization within the flanges in the gallbladder and the antrum of the stomach (c) and resolved the patient’s symptoms the next day. Surgical pathology demonstrated pancreatic ductal carcinoma of the major and minor papillae, pancreatic head and uncinate process.
Discussion: Interventions for obstructive jaundice include ERCP with biliary stenting, percutaneous transhepatic biliary drainage, EUS with LAMS placement, as well as surgery. While ERCP is the first line option, the patient’s distorted ampullary anatomy would have made cannulation and stenting challenging and high risk. Percutaneous drainage would expose the patient to risk of dislodging, obstructing, leaking, and infection. Seen below, LAMS has a relatively large diameter which allows for immediate biliary drainage, proven by the patient’s rapid relief of symptoms. Since a duodenal approach is more commonly used, current literature displays only a small number of cases showcasing the technical success of gastric approach for CBD access via LAMS, for instance, in the setting of duodenal stenosis. Our case demonstrates the versatility of the Axios stent with another successful alternative approach and proves a transgastric approach with LAMS is a viable alternative to surgery for malignant obstructive jaundice.
Disclosures:
Asad Rehman, DO1, Vikas Sethi, DO2, Geoffrey Goldsberry, DO1, Joseph Namey, DO2, Muhammad Khan, MD, MPH1, Meir Mizrahi, MD1. E0449 - Diverting Disaster: EUS-Guided Trans-Gastric Biliary Drainage, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1HCA West Florida Largo Medical Center, Largo, FL; 2Largo Medical Center, Largo, FL
Introduction: Lumen-apposing metal stents (LAMS) are a relatively new intervention that can be used for high risk surgical cases, such as malignant obstructions not amenable to ERCP. There are few case reports using LAMS with Endoscopic Ultrasound (EUS) to achieve drainage and palliative therapy in these situations, especially using a gastric over duodenal approach. In this case, we add to the growing body of literature supporting a transgastric approach for biliary drainage using LAMS.
Case Description/Methods: A 73 year-old male was admitted due to concerns for obstructive jaundice. He presented with pruritis, nausea, vomiting, copious nasogastric tube bilious output and a total bilirubin of 19.8mg/dL. MRCP revealed a distal CBD stricture measuring 12 mm in length, marked intrahepatic and extrahepatic biliary dilatation and an 8mm dilated pancreatic duct. EGD revealed a submucosal mass within the duodenal bulb causing gallbladder impingement (a). EUS was then completed and revealed similar findings to MRCP including an atrophic pancreas and severely dilated gallbladder (b). The ampullary mass, noted on CT, was also identified under EUS and fine needle biopsy was performed. A 10mm x 10mm LAMS was placed under endoscopic and fluoroscopic visualization within the flanges in the gallbladder and the antrum of the stomach (c) and resolved the patient’s symptoms the next day. Surgical pathology demonstrated pancreatic ductal carcinoma of the major and minor papillae, pancreatic head and uncinate process.
Discussion: Interventions for obstructive jaundice include ERCP with biliary stenting, percutaneous transhepatic biliary drainage, EUS with LAMS placement, as well as surgery. While ERCP is the first line option, the patient’s distorted ampullary anatomy would have made cannulation and stenting challenging and high risk. Percutaneous drainage would expose the patient to risk of dislodging, obstructing, leaking, and infection. Seen below, LAMS has a relatively large diameter which allows for immediate biliary drainage, proven by the patient’s rapid relief of symptoms. Since a duodenal approach is more commonly used, current literature displays only a small number of cases showcasing the technical success of gastric approach for CBD access via LAMS, for instance, in the setting of duodenal stenosis. Our case demonstrates the versatility of the Axios stent with another successful alternative approach and proves a transgastric approach with LAMS is a viable alternative to surgery for malignant obstructive jaundice.
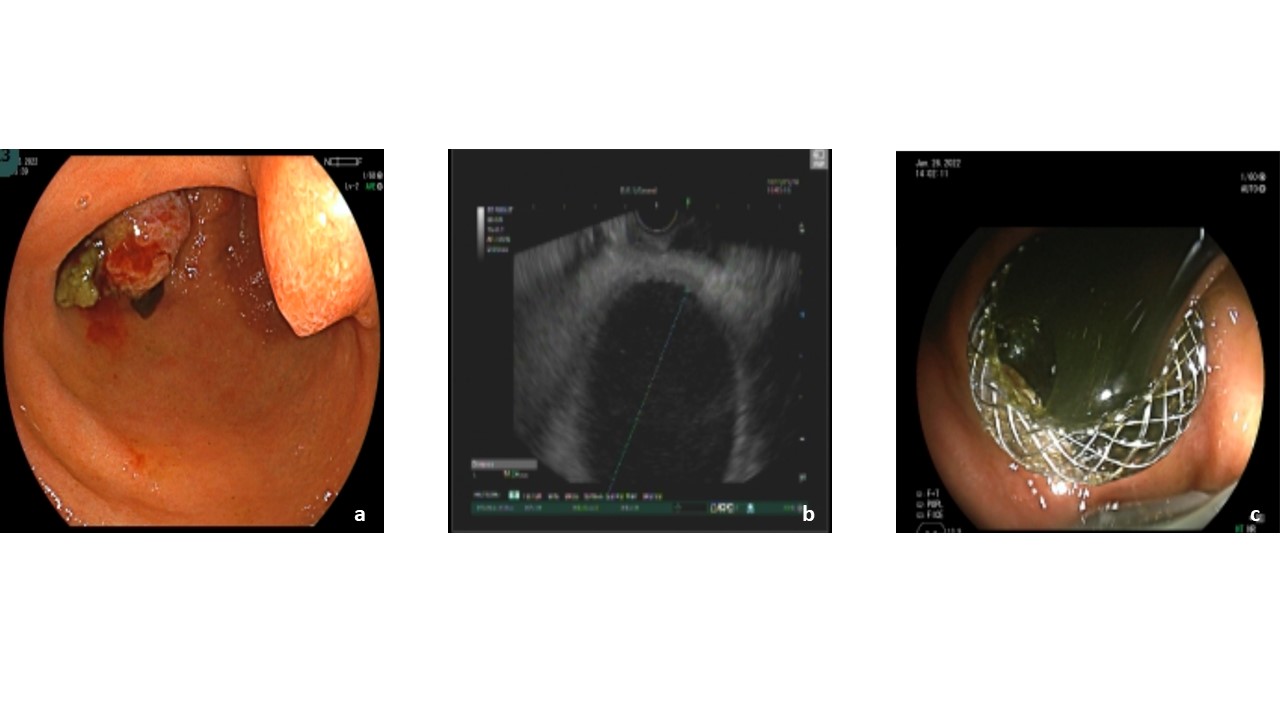
Figure: Image a: Dilated minor and major papillae with evidence of duodenal obstruction.
b: EUS view of the dilated gallbladder.
c: Biliary drainage from gallbladder after LAMS placement.
b: EUS view of the dilated gallbladder.
c: Biliary drainage from gallbladder after LAMS placement.
Disclosures:
Asad Rehman indicated no relevant financial relationships.
Vikas Sethi indicated no relevant financial relationships.
Geoffrey Goldsberry indicated no relevant financial relationships.
Joseph Namey indicated no relevant financial relationships.
Muhammad Khan indicated no relevant financial relationships.
Meir Mizrahi indicated no relevant financial relationships.
Asad Rehman, DO1, Vikas Sethi, DO2, Geoffrey Goldsberry, DO1, Joseph Namey, DO2, Muhammad Khan, MD, MPH1, Meir Mizrahi, MD1. E0449 - Diverting Disaster: EUS-Guided Trans-Gastric Biliary Drainage, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
