Back
Poster Session A - Sunday Afternoon
A0448 - Endoscopic Papillectomy for Gangliocytic Paraganglioma
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Edward Cay, DO
Spectrum Health Lakeland
St. Joseph, MI
Presenting Author(s)
Edward Cay, DO1, Nicholas McDonald, MD2, Mohammad Bilal, MD3
1Spectrum Health Lakeland, St. Joseph, MI; 2University of Minnesota, Minneapolis, MN; 3University of Minnesota, Minneapolis VA Medical Center, Minneapolis, MN
Introduction: Neuroendocrine tumors (NET) most commonly occur in the small bowel; however, NETs at the ampulla of Vater are rare and more aggressive, irrespective of size. Gangliocytic paragangliomas (GP) are a more benign type of NET that must be properly differentiated from other similar appearing NETs, which may carry a worse prognosis.
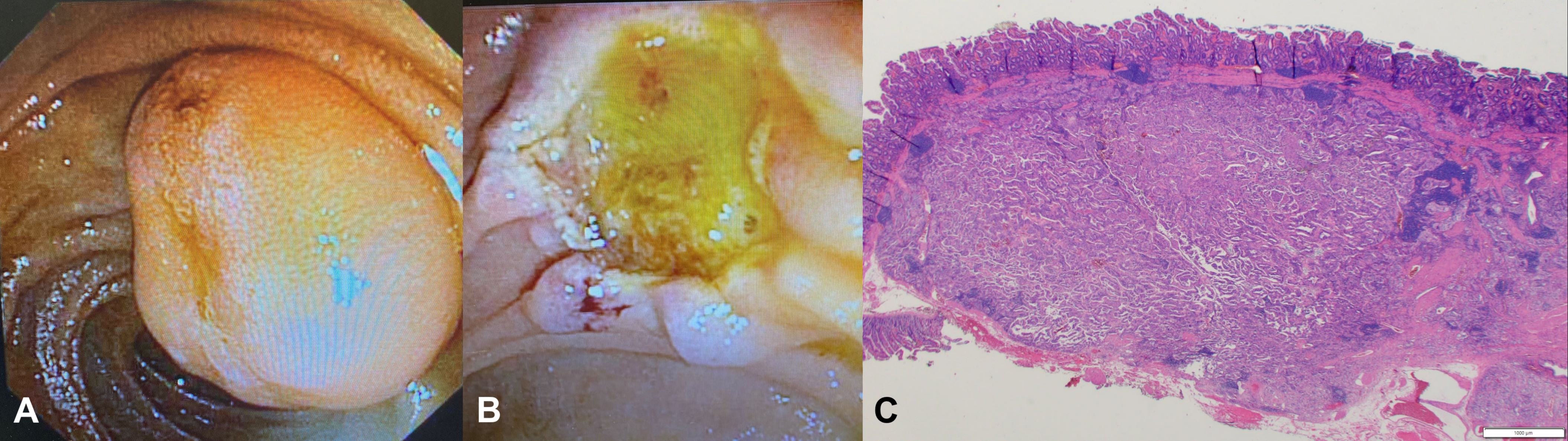
Case Description/Methods: A 77-year-old man presented with right flank pain and was incidentally found to have a duodenal mass in the periampullary region measuring 11 x 8 mm, with dilation of the common bile duct to 10 mm on computed tomography scan. Laboratory data showed normal liver function tests. Esophagogastroduodenoscopy revealed a subepithelial lesion at the ampulla, and endoscopic ultrasound (EUS) demonstrated a 15 x 12 mm hypoechoic subepithelial lesion arising from the submucosa. A fine needle biopsy was performed and immunohistochemical staining was positive for synaptophysin, chromogranin and pankeratin, consistent with neoplasm with neuroendocrine differentiation. Subsequent DOTATATE PET scan showed uptake in the ampullary region with no uptake anywhere else. The case was discussed in multidisciplinary conference, and the decision was made to proceed with endoscopic papillectomy given concerns for NET. An endoscopic retrograde cholangiopancreatography (ERCP) with endoscopic papillectomy was performed. A biliary and pancreatic duct stent was placed. The pathology was consistent with gangliocytic paraganglioma, and the patient had no adverse events with removal of stents after four weeks.
Discussion: Gangliocytic paragangliomas typically arise in the second part of the duodenum, presenting as gastrointestinal bleeding and abdominal pain.
Although its distribution varies significantly, GPs in particular embody epithelioid, spindle-shaped, and ganglion-like cell types. While GPs are predominantly benign, rare reports of spread to regional lymph nodes are present. Our report shows that endoscopic papillectomy is safe and effective for both diagnostic and therapeutic purposes in the management of ampullary gangliocytic paragangliomas.
Disclosures:
Edward Cay, DO1, Nicholas McDonald, MD2, Mohammad Bilal, MD3. A0448 - Endoscopic Papillectomy for Gangliocytic Paraganglioma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Spectrum Health Lakeland, St. Joseph, MI; 2University of Minnesota, Minneapolis, MN; 3University of Minnesota, Minneapolis VA Medical Center, Minneapolis, MN
Introduction: Neuroendocrine tumors (NET) most commonly occur in the small bowel; however, NETs at the ampulla of Vater are rare and more aggressive, irrespective of size. Gangliocytic paragangliomas (GP) are a more benign type of NET that must be properly differentiated from other similar appearing NETs, which may carry a worse prognosis.
Case Description/Methods: A 77-year-old man presented with right flank pain and was incidentally found to have a duodenal mass in the periampullary region measuring 11 x 8 mm, with dilation of the common bile duct to 10 mm on computed tomography scan. Laboratory data showed normal liver function tests. Esophagogastroduodenoscopy revealed a subepithelial lesion at the ampulla, and endoscopic ultrasound (EUS) demonstrated a 15 x 12 mm hypoechoic subepithelial lesion arising from the submucosa. A fine needle biopsy was performed and immunohistochemical staining was positive for synaptophysin, chromogranin and pankeratin, consistent with neoplasm with neuroendocrine differentiation. Subsequent DOTATATE PET scan showed uptake in the ampullary region with no uptake anywhere else. The case was discussed in multidisciplinary conference, and the decision was made to proceed with endoscopic papillectomy given concerns for NET. An endoscopic retrograde cholangiopancreatography (ERCP) with endoscopic papillectomy was performed. A biliary and pancreatic duct stent was placed. The pathology was consistent with gangliocytic paraganglioma, and the patient had no adverse events with removal of stents after four weeks.
Discussion: Gangliocytic paragangliomas typically arise in the second part of the duodenum, presenting as gastrointestinal bleeding and abdominal pain.
Although its distribution varies significantly, GPs in particular embody epithelioid, spindle-shaped, and ganglion-like cell types. While GPs are predominantly benign, rare reports of spread to regional lymph nodes are present. Our report shows that endoscopic papillectomy is safe and effective for both diagnostic and therapeutic purposes in the management of ampullary gangliocytic paragangliomas.
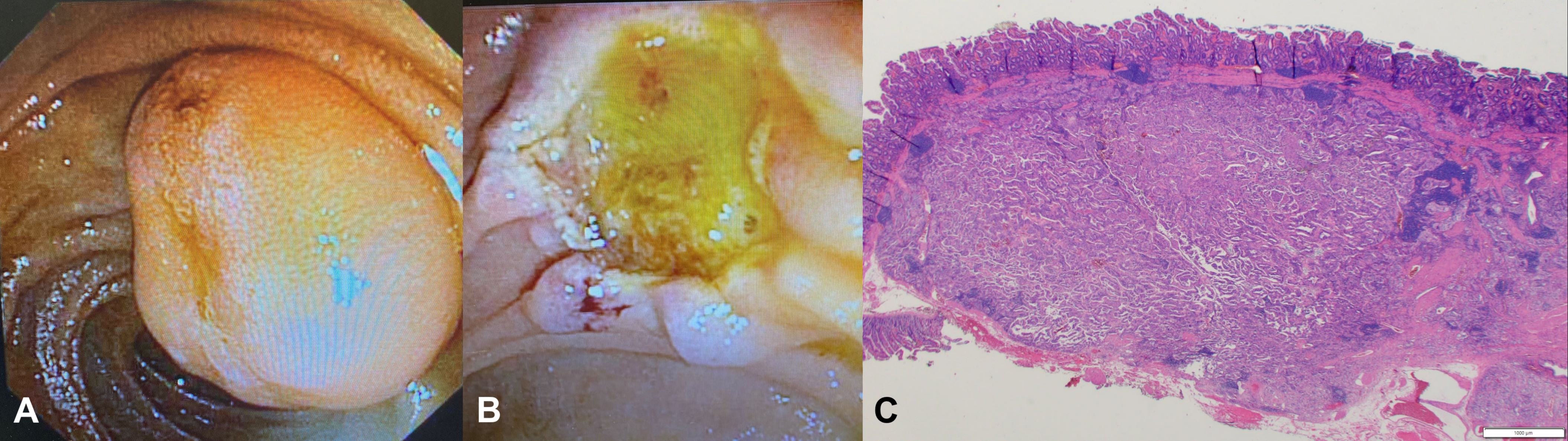
Figure: Figure 1. Ampullary lesion prior to (A) and after endoscopic papillectomy (B), with histopathology consistent with gangliocytic paraganglioma (C).
Disclosures:
Edward Cay indicated no relevant financial relationships.
Nicholas McDonald indicated no relevant financial relationships.
Mohammad Bilal indicated no relevant financial relationships.
Edward Cay, DO1, Nicholas McDonald, MD2, Mohammad Bilal, MD3. A0448 - Endoscopic Papillectomy for Gangliocytic Paraganglioma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
