Back
Poster Session E - Tuesday Afternoon
E0464 - EUS-Guided Jejunojejunostomy Through a Gastrojejunal Stent
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Bryan Wey, MD
Robert Wood Johnson University Hospital
New Brunswick, NJ
Presenting Author(s)
Bryan Wey, MD1, Rodrigo Duarte-Chavez, MD2, Haroon Shahid, MD2, Michel Kahaleh, MD2
1Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: In patients with malignant gastric outlet obstruction, surgical gastrojejunostomy has been classically viewed as the intervention of choice. With advancements in endoscopy, enteral self-expandable metal stents (SEMS) have become a non-operative alternative. Although boasting a high rate of success, stent patency is brief, frequently requiring reintervention due to tumor ingrowth. Endoscopic-ultrasound-guided gastrojejunostomy (EUS-GJ) with lumen-apposing metal stents (LAMS) is a newer but feasible approach that provides symptom relief without the invasive risk of surgery or the limited lifespan of enteral stenting.
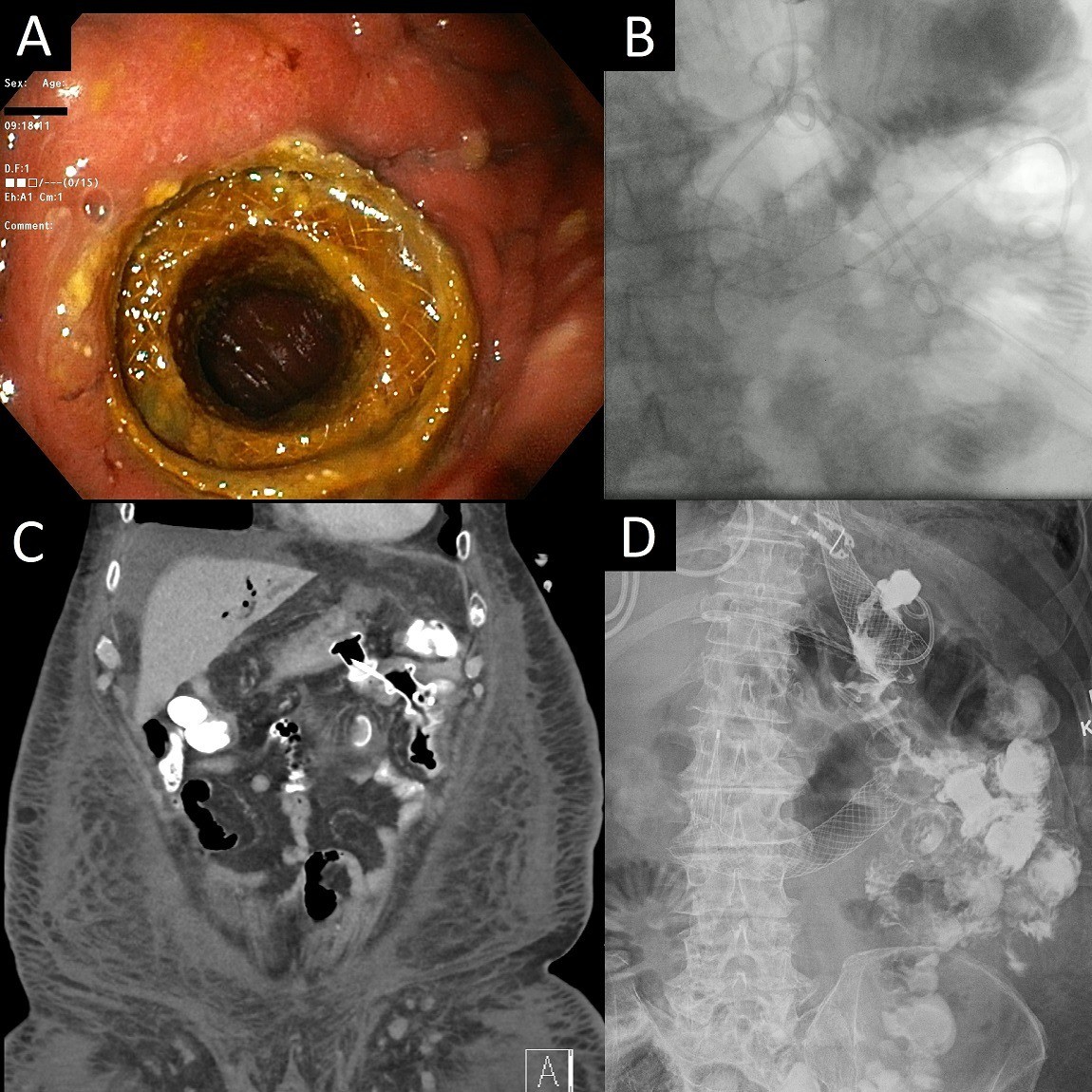
Case Description/Methods: A 75-year-old Caucasian male with a past medical history of metastatic distal esophageal adenocarcinoma presented to the hospital for early satiety and vomiting. He was diagnosed with malignant gastric outlet obstruction, underwent upper endoscopy, and received a SEMS to traverse the duodenal lesion. His obstructive symptoms resolved, but he returned to the hospital shortly after due to recurrent symptoms. He underwent repeat endoscopy and received an EUS-GJ that was functional at discharge. Several months later, the patient was admitted to a sister hospital with recurrent obstructive symptoms, where he received a surgical jejunal tube distal to the EUS-GJ. Shortly after the patient was again unable to tolerate oral or tube feeds, and he was transferred to the original hospital for interventional endoscopy. The initial EUS-GJ was widely patent and easily traversed with the endoscope (Figure A). The jejunal tube was visualized, but the endoscope could not be advanced past the tube due to intraluminal narrowing, which persisted even after removal and exchange of the tube. The decision was made to perform an EUS-guided enteroenterostomy to bypass the jejunal tube and area of obstruction (Figure B). Imaging was obtained to confirm stent patency (Figures C and D) and the patient was able tolerate an oral diet without difficulty.
Discussion: Methods of transluminal stenting have been demonstrated previously in patients with altered anatomy. EUS-GJ utilizes similar concepts, allowing for non-surgical bypass of malignant gastrointestinal obstructions. Given its distance from the obstructive tumor, EUS-GJ is not as affected by tumor ingrowth or expansion compared to SEMS. Here we present a novel case of an EUS-guided enteroenterostomy through an existing EUS-GJ. Like an EUS-GJ, EUS-guided enteroenterostomy can be offered for palliation of malignant bowel obstruction.
Disclosures:
Bryan Wey, MD1, Rodrigo Duarte-Chavez, MD2, Haroon Shahid, MD2, Michel Kahaleh, MD2. E0464 - EUS-Guided Jejunojejunostomy Through a Gastrojejunal Stent, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: In patients with malignant gastric outlet obstruction, surgical gastrojejunostomy has been classically viewed as the intervention of choice. With advancements in endoscopy, enteral self-expandable metal stents (SEMS) have become a non-operative alternative. Although boasting a high rate of success, stent patency is brief, frequently requiring reintervention due to tumor ingrowth. Endoscopic-ultrasound-guided gastrojejunostomy (EUS-GJ) with lumen-apposing metal stents (LAMS) is a newer but feasible approach that provides symptom relief without the invasive risk of surgery or the limited lifespan of enteral stenting.
Case Description/Methods: A 75-year-old Caucasian male with a past medical history of metastatic distal esophageal adenocarcinoma presented to the hospital for early satiety and vomiting. He was diagnosed with malignant gastric outlet obstruction, underwent upper endoscopy, and received a SEMS to traverse the duodenal lesion. His obstructive symptoms resolved, but he returned to the hospital shortly after due to recurrent symptoms. He underwent repeat endoscopy and received an EUS-GJ that was functional at discharge. Several months later, the patient was admitted to a sister hospital with recurrent obstructive symptoms, where he received a surgical jejunal tube distal to the EUS-GJ. Shortly after the patient was again unable to tolerate oral or tube feeds, and he was transferred to the original hospital for interventional endoscopy. The initial EUS-GJ was widely patent and easily traversed with the endoscope (Figure A). The jejunal tube was visualized, but the endoscope could not be advanced past the tube due to intraluminal narrowing, which persisted even after removal and exchange of the tube. The decision was made to perform an EUS-guided enteroenterostomy to bypass the jejunal tube and area of obstruction (Figure B). Imaging was obtained to confirm stent patency (Figures C and D) and the patient was able tolerate an oral diet without difficulty.
Discussion: Methods of transluminal stenting have been demonstrated previously in patients with altered anatomy. EUS-GJ utilizes similar concepts, allowing for non-surgical bypass of malignant gastrointestinal obstructions. Given its distance from the obstructive tumor, EUS-GJ is not as affected by tumor ingrowth or expansion compared to SEMS. Here we present a novel case of an EUS-guided enteroenterostomy through an existing EUS-GJ. Like an EUS-GJ, EUS-guided enteroenterostomy can be offered for palliation of malignant bowel obstruction.
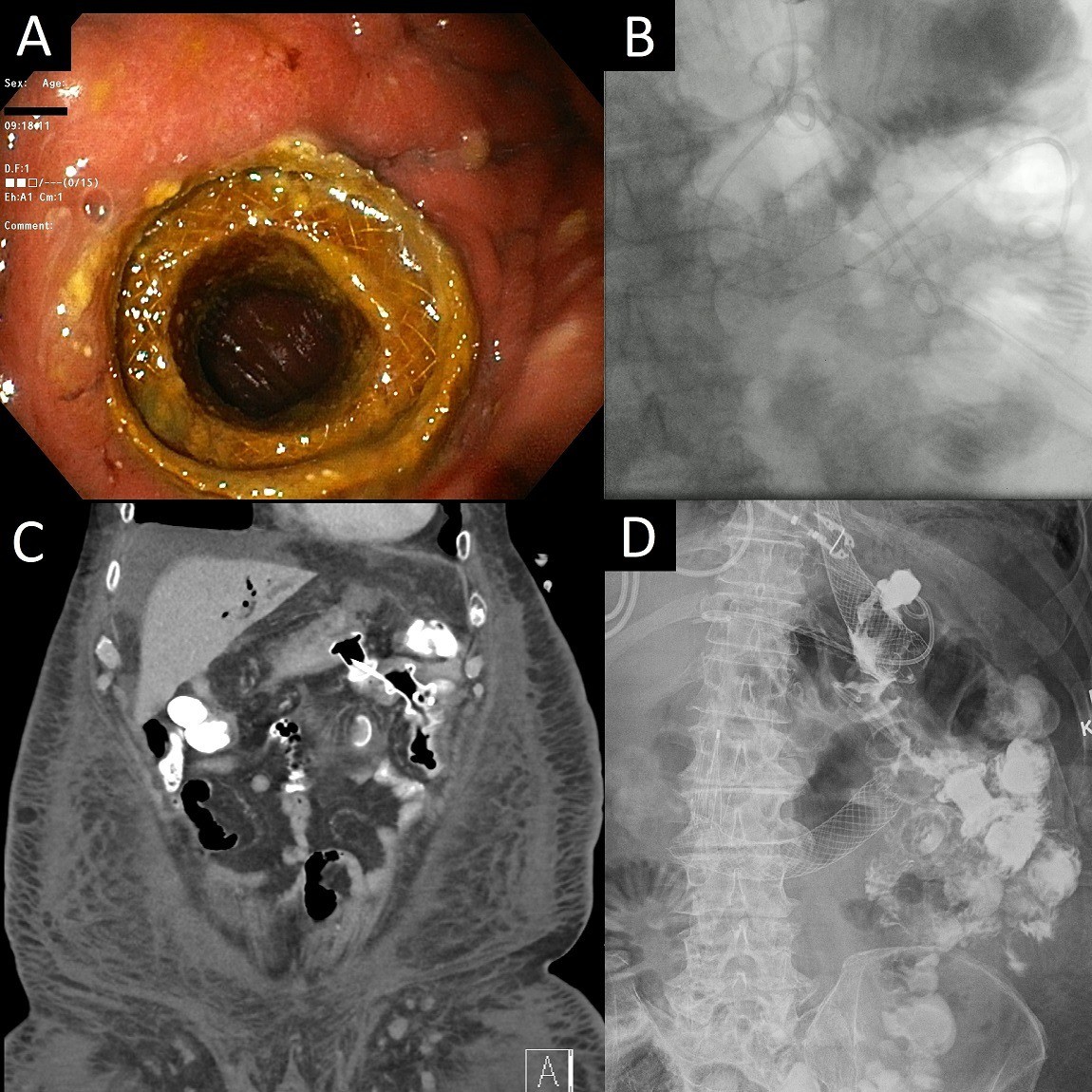
Figure: Figure A. Patent gastrojejunal stent.
Figure B. Intraprocedure fluoroscopy showing a gastrojejunal stent, duodenal stent, and newly inserted jejunojejunal stent.
Figures C and D. Postprocedure abdominal imaging showing the functional jejunojejunal stent.
Figure B. Intraprocedure fluoroscopy showing a gastrojejunal stent, duodenal stent, and newly inserted jejunojejunal stent.
Figures C and D. Postprocedure abdominal imaging showing the functional jejunojejunal stent.
Disclosures:
Bryan Wey indicated no relevant financial relationships.
Rodrigo Duarte-Chavez indicated no relevant financial relationships.
Haroon Shahid indicated no relevant financial relationships.
Michel Kahaleh indicated no relevant financial relationships.
Bryan Wey, MD1, Rodrigo Duarte-Chavez, MD2, Haroon Shahid, MD2, Michel Kahaleh, MD2. E0464 - EUS-Guided Jejunojejunostomy Through a Gastrojejunal Stent, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
