Back
Poster Session E - Tuesday Afternoon
E0428 - Necrobiotic Lung Nodules in Patient With Ulcerative Colitis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
- AJ
Ayeza Jamil, DO
MercyHealth
Rockford, IL
Presenting Author(s)
Ayeza Jamil, DO1, Altaf Dawood, MD2, Naser Khan, MD1, Thayer Hamoudah, MD1, Addie Spier, MD1
1MercyHealth, Rockford, IL; 2MercyHealth Internal Medicine Residency Program, Rockford, IL
Introduction: Ulcerative colitis and Crohn’s disease are two forms of inflammatory bowel disease (IBD). 25-40% of IBD patients have extra-intestinal manifestations (EIM). Pulmonary manifestations are one of the rarest forms of EIM, particularly necrobiotic nodules. It is a challenge to diagnose as it presents with symptoms similar to autoimmune, vasculitis, or infectious pathologies. We present a rare case of a patient who was found to have necrobiotic lung nodules during an acute ulcerative colitis flare.
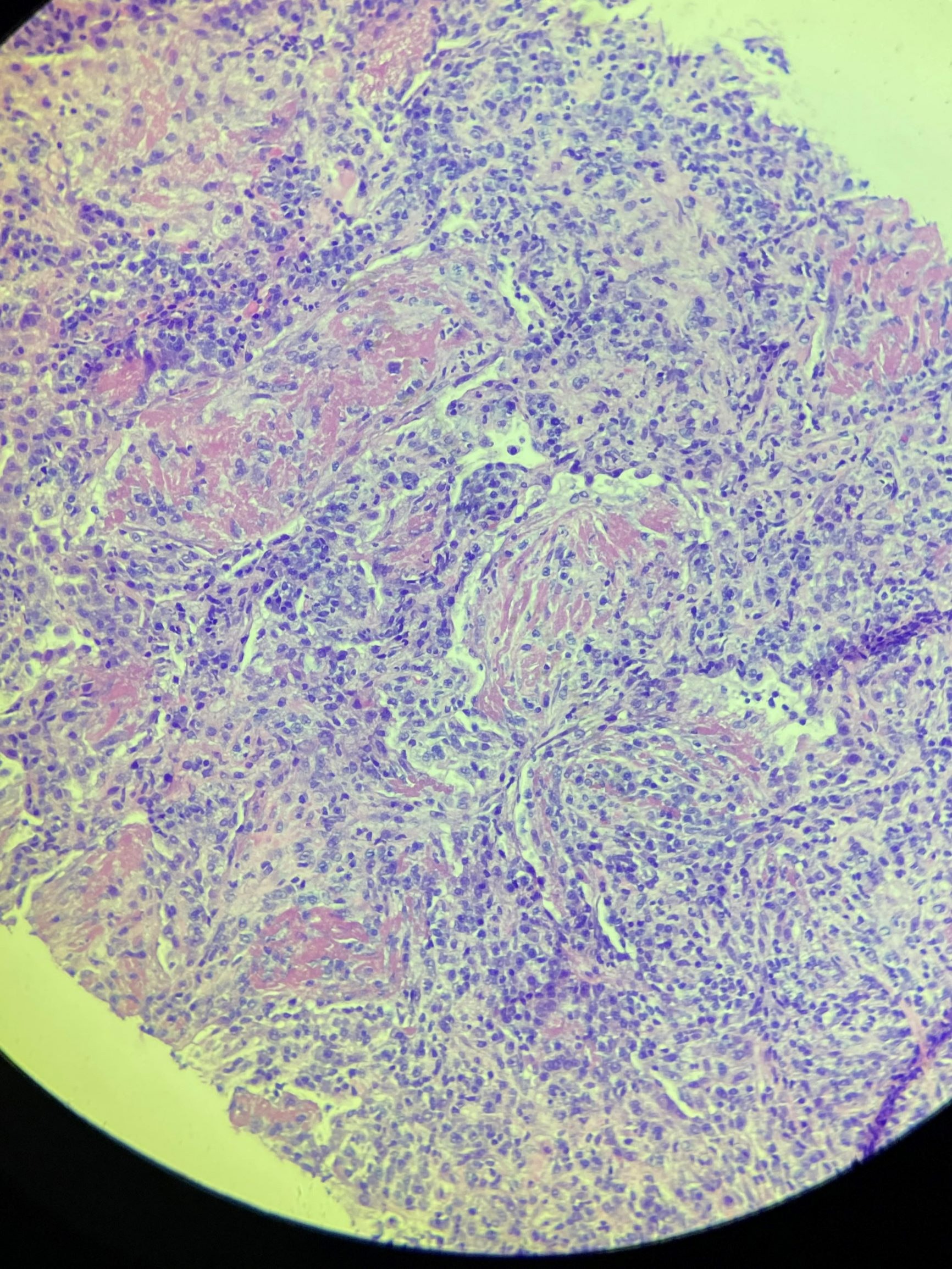
Case Description/Methods: 44-year-old male with newly diagnosed ulcerative pancolitis, presented with diarrhea and hematochezia for 8 weeks and 4 weeks of leg ulcers. He denied any other symptoms. 4 months ago, he was started on high dose steroids and switched to vedolizumab, however began to relapse after steroids were tapered. On admission, vitals significant for tachycardia at 118 bpm. Physical exam was significant for lower extremity ulcers consistent with pyoderma gangrenosum. Labs significant for leukocytosis (16,500/µL), Hg of 6.8, and elevated CRP at 160.26. Findings were suggestive of IBD flare and he also underwent chest x-ray which showed multifocal nodular airspace opacities, which appeared to have developed cavitations. CT chest revealed bilateral pulmonary nodules. He underwent infectious, autoimmune and vasculitis work up including HIV, tuberculosis, bacterial, viral, endocarditis, ANA, ANCA as well as fungal serologies which were all negative. He had CT guided biopsies, which were suggestive of necrobiotic lung nodules. Repeat CT chest showed interval improvement in solid and cavitary nodules. Given extensive negative infectious work up and improvement with steroids and infliximab, his presentation was consistent with necrobiotic lung nodules secondary to uncontrolled inflammatory bowel disease.
Discussion: We describe a rare case of necrobiotic lung nodules as an extra-intestinal manifestation of uncontrolled ulcerative colitis. Histologically, these nodules are sterile aggregates of neutrophils, that can cavitate and have a high degree of resemblance to pyoderma gangrenosum in cases of IBD. Few cases of necrobiotic lung nodules with IBD have been reported and most of them had respiratory symptoms but our case did not present with respiratory manifestations. In conclusion, necrobiotic lung nodules should be considered as a differential diagnosis of lung nodules in patients with IBD while excluding any infectious etiologies as mandatory before starting treatment with steroids and biologics.
Disclosures:
Ayeza Jamil, DO1, Altaf Dawood, MD2, Naser Khan, MD1, Thayer Hamoudah, MD1, Addie Spier, MD1. E0428 - Necrobiotic Lung Nodules in Patient With Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1MercyHealth, Rockford, IL; 2MercyHealth Internal Medicine Residency Program, Rockford, IL
Introduction: Ulcerative colitis and Crohn’s disease are two forms of inflammatory bowel disease (IBD). 25-40% of IBD patients have extra-intestinal manifestations (EIM). Pulmonary manifestations are one of the rarest forms of EIM, particularly necrobiotic nodules. It is a challenge to diagnose as it presents with symptoms similar to autoimmune, vasculitis, or infectious pathologies. We present a rare case of a patient who was found to have necrobiotic lung nodules during an acute ulcerative colitis flare.
Case Description/Methods: 44-year-old male with newly diagnosed ulcerative pancolitis, presented with diarrhea and hematochezia for 8 weeks and 4 weeks of leg ulcers. He denied any other symptoms. 4 months ago, he was started on high dose steroids and switched to vedolizumab, however began to relapse after steroids were tapered. On admission, vitals significant for tachycardia at 118 bpm. Physical exam was significant for lower extremity ulcers consistent with pyoderma gangrenosum. Labs significant for leukocytosis (16,500/µL), Hg of 6.8, and elevated CRP at 160.26. Findings were suggestive of IBD flare and he also underwent chest x-ray which showed multifocal nodular airspace opacities, which appeared to have developed cavitations. CT chest revealed bilateral pulmonary nodules. He underwent infectious, autoimmune and vasculitis work up including HIV, tuberculosis, bacterial, viral, endocarditis, ANA, ANCA as well as fungal serologies which were all negative. He had CT guided biopsies, which were suggestive of necrobiotic lung nodules. Repeat CT chest showed interval improvement in solid and cavitary nodules. Given extensive negative infectious work up and improvement with steroids and infliximab, his presentation was consistent with necrobiotic lung nodules secondary to uncontrolled inflammatory bowel disease.
Discussion: We describe a rare case of necrobiotic lung nodules as an extra-intestinal manifestation of uncontrolled ulcerative colitis. Histologically, these nodules are sterile aggregates of neutrophils, that can cavitate and have a high degree of resemblance to pyoderma gangrenosum in cases of IBD. Few cases of necrobiotic lung nodules with IBD have been reported and most of them had respiratory symptoms but our case did not present with respiratory manifestations. In conclusion, necrobiotic lung nodules should be considered as a differential diagnosis of lung nodules in patients with IBD while excluding any infectious etiologies as mandatory before starting treatment with steroids and biologics.
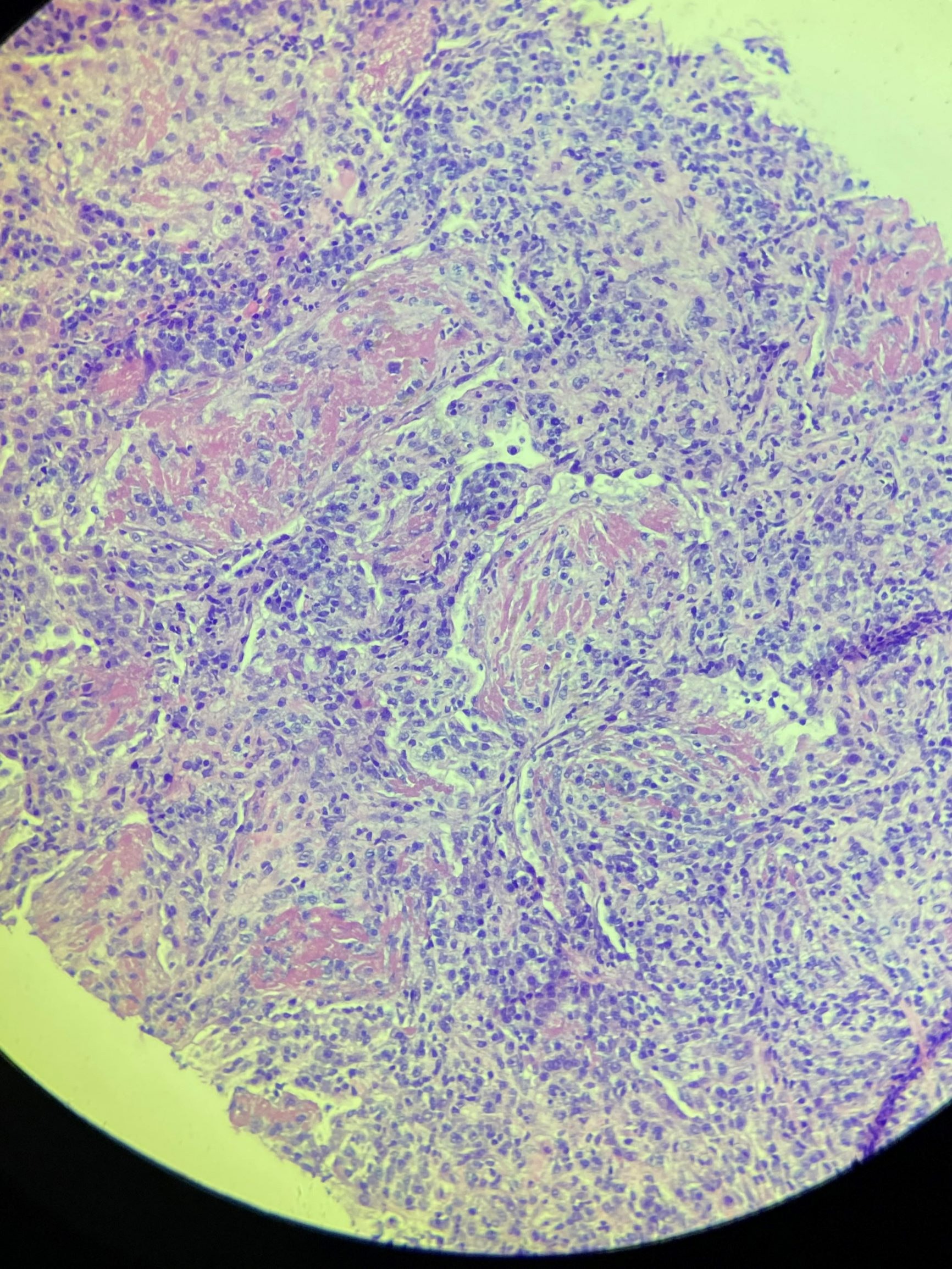
Figure: CT guided biopsy suggestive of necrobiotic lung nodule.
Disclosures:
Ayeza Jamil indicated no relevant financial relationships.
Altaf Dawood indicated no relevant financial relationships.
Naser Khan indicated no relevant financial relationships.
Thayer Hamoudah indicated no relevant financial relationships.
Addie Spier indicated no relevant financial relationships.
Ayeza Jamil, DO1, Altaf Dawood, MD2, Naser Khan, MD1, Thayer Hamoudah, MD1, Addie Spier, MD1. E0428 - Necrobiotic Lung Nodules in Patient With Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
