Back
Poster Session E - Tuesday Afternoon
E0371 - Recent Trends and Mortality Outcomes Among Inflammatory Bowel Disease Patients With and Without Severe Obesity
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
- PS
Phani Keerthi Surapaneni, MD
Morehouse School of Medicine
Morgantown, WV
Presenting Author(s)
Phani Keerthi Surapaneni, MD1, Joseph-Kevin Igwe, MD, MPH2, Laura Davisson, MD3, Jabez K. Beazer, MD4, Treah Haggerty, MD5, Darwish Alabyad, MBBS6, Krystal Mills, MD2, Phuong Nguyen, MD2, Paula Adamson, MD2
1Morehouse School of Medicine, Morgantown, WV; 2Morehouse School of Medicine, Atlanta, GA; 3West Virginia University School of Medicine, Morgantown, WV; 4Morehouse Internal Medicine GME, Atlanta, GA; 5West Virginia University School Of Medicine, Morgantown, WV; 6Morehouse School Of Medicine, Atlanta, WV
Introduction: Inflammatory bowel disease (IBD) comprises crohn's disease and ulcerative colitis. Severe obesity (SO) is defined as body mass index (BMI) >40 kg/m2. Obesity is a known risk factor for developing IBD due to accumulation of intra-abdominal fat, cytokine production, alteration of gut microbiome contributing to mucosal inflammation. Using the National Inpatient Sample (NIS), our study examines trends and mortality outcomes among IBD patients with and without SO.
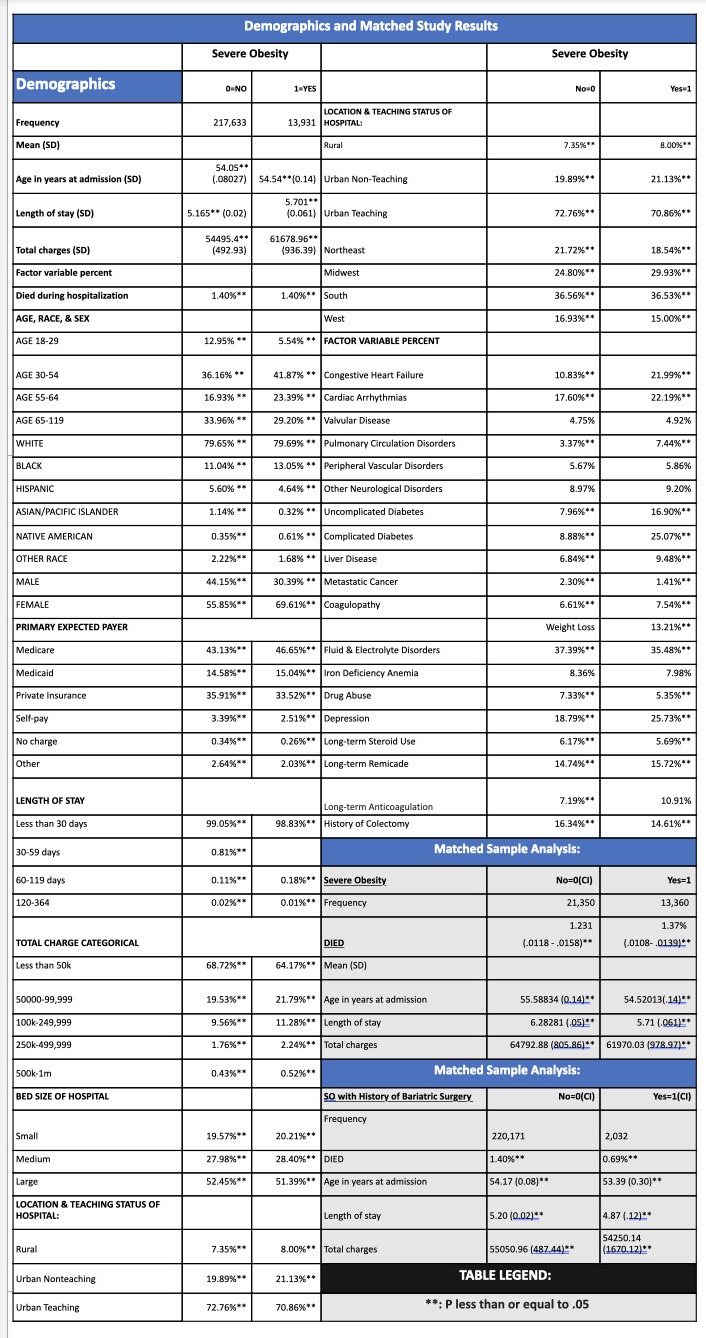
Methods: The NIS database was used to identify patients (pts) aged ≥18 years with diagnosis of IBD using ICD-10 codes between 2016-2019. Chi square, ANOVA, and multivariate regression were used to compare significant associations with variables and primary outcome of mortality among pts with IBD stratified by BMI >40 (Severe Obesity-SO) and < 40kg/m2 (Non- severe obesity) . Propensity Score Matching was used to assess the effect of SO and history of bariatric surgery on the outcome of death. STATA MP 17 software was used for analysis.
Results: Of the 222,203 pts meeting inclusion criteria, 13,931 (69.61% female; mean age: 54) had SO and 217,633 (55.85% female; mean age: 54) without SO (p=0.23). There was a positive temporal relationship in death rate over time and SO (p=0.00); but a significant negative relationship generally within the IBD population (p=0.02). There was a positive trend in bariatric surgery over time within the general IBD population (p=0.00) and among the IBD-SO subpopulation (p=0.00). Adjusted odds (aOR) of death were 46.73% higher among those with severe obesity compared to other BMI groups (95%CI 1.180-1.865, p=0.00). In propensity score matching analysis, there was a 2.40% higher risk of death in patients with SO compared to non-SO patients (p= 0.03). History of bariatric surgery was associated with 0.70% (p=.026) and 0.85%(p=.01) decreased risk of death in the IBD population and the SO subpopulation compared to those without a history of bariatric surgery, respectively.
Discussion: Among IBD pts, severe obesity was associated with increased mortality compared non severe obesity. Nonetheless, bariatric surgery within the entirety of the population was associated with decreased mortality. There may be some mortality benefit associated with higher weights-possibly related to medication side effects or markers of well controlled disease as weight loss itself was associated with increased odds of mortality. More studies are warranted to analyze efficacy of bariatric surgery in other BMI groups.
Disclosures:
Phani Keerthi Surapaneni, MD1, Joseph-Kevin Igwe, MD, MPH2, Laura Davisson, MD3, Jabez K. Beazer, MD4, Treah Haggerty, MD5, Darwish Alabyad, MBBS6, Krystal Mills, MD2, Phuong Nguyen, MD2, Paula Adamson, MD2. E0371 - Recent Trends and Mortality Outcomes Among Inflammatory Bowel Disease Patients With and Without Severe Obesity, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Morehouse School of Medicine, Morgantown, WV; 2Morehouse School of Medicine, Atlanta, GA; 3West Virginia University School of Medicine, Morgantown, WV; 4Morehouse Internal Medicine GME, Atlanta, GA; 5West Virginia University School Of Medicine, Morgantown, WV; 6Morehouse School Of Medicine, Atlanta, WV
Introduction: Inflammatory bowel disease (IBD) comprises crohn's disease and ulcerative colitis. Severe obesity (SO) is defined as body mass index (BMI) >40 kg/m2. Obesity is a known risk factor for developing IBD due to accumulation of intra-abdominal fat, cytokine production, alteration of gut microbiome contributing to mucosal inflammation. Using the National Inpatient Sample (NIS), our study examines trends and mortality outcomes among IBD patients with and without SO.
Methods: The NIS database was used to identify patients (pts) aged ≥18 years with diagnosis of IBD using ICD-10 codes between 2016-2019. Chi square, ANOVA, and multivariate regression were used to compare significant associations with variables and primary outcome of mortality among pts with IBD stratified by BMI >40 (Severe Obesity-SO) and < 40kg/m2 (Non- severe obesity) . Propensity Score Matching was used to assess the effect of SO and history of bariatric surgery on the outcome of death. STATA MP 17 software was used for analysis.
Results: Of the 222,203 pts meeting inclusion criteria, 13,931 (69.61% female; mean age: 54) had SO and 217,633 (55.85% female; mean age: 54) without SO (p=0.23). There was a positive temporal relationship in death rate over time and SO (p=0.00); but a significant negative relationship generally within the IBD population (p=0.02). There was a positive trend in bariatric surgery over time within the general IBD population (p=0.00) and among the IBD-SO subpopulation (p=0.00). Adjusted odds (aOR) of death were 46.73% higher among those with severe obesity compared to other BMI groups (95%CI 1.180-1.865, p=0.00). In propensity score matching analysis, there was a 2.40% higher risk of death in patients with SO compared to non-SO patients (p= 0.03). History of bariatric surgery was associated with 0.70% (p=.026) and 0.85%(p=.01) decreased risk of death in the IBD population and the SO subpopulation compared to those without a history of bariatric surgery, respectively.
Discussion: Among IBD pts, severe obesity was associated with increased mortality compared non severe obesity. Nonetheless, bariatric surgery within the entirety of the population was associated with decreased mortality. There may be some mortality benefit associated with higher weights-possibly related to medication side effects or markers of well controlled disease as weight loss itself was associated with increased odds of mortality. More studies are warranted to analyze efficacy of bariatric surgery in other BMI groups.
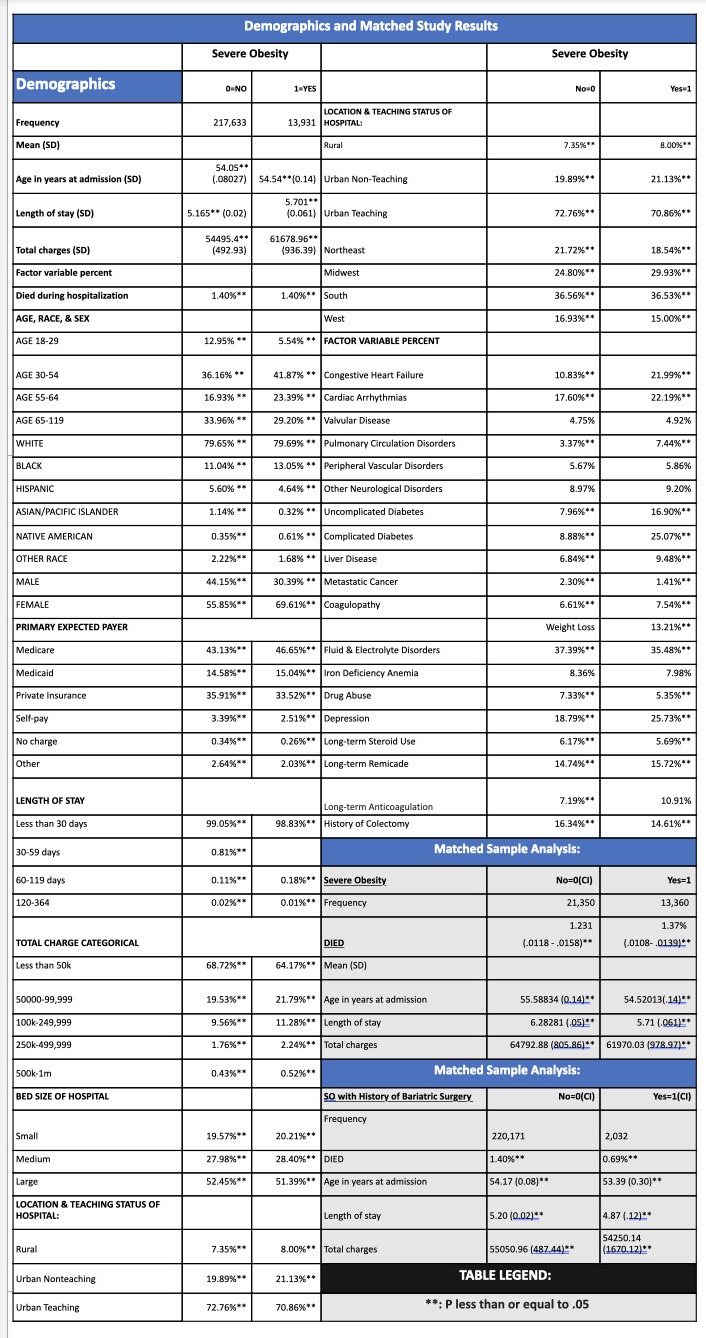
Figure: Demographics and matched study results
Disclosures:
Phani Keerthi Surapaneni indicated no relevant financial relationships.
Joseph-Kevin Igwe indicated no relevant financial relationships.
Laura Davisson indicated no relevant financial relationships.
Jabez Beazer indicated no relevant financial relationships.
Treah Haggerty indicated no relevant financial relationships.
Darwish Alabyad indicated no relevant financial relationships.
Krystal Mills indicated no relevant financial relationships.
Phuong Nguyen indicated no relevant financial relationships.
Paula Adamson indicated no relevant financial relationships.
Phani Keerthi Surapaneni, MD1, Joseph-Kevin Igwe, MD, MPH2, Laura Davisson, MD3, Jabez K. Beazer, MD4, Treah Haggerty, MD5, Darwish Alabyad, MBBS6, Krystal Mills, MD2, Phuong Nguyen, MD2, Paula Adamson, MD2. E0371 - Recent Trends and Mortality Outcomes Among Inflammatory Bowel Disease Patients With and Without Severe Obesity, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
