Back
Poster Session E - Tuesday Afternoon
E0397 - Adherence to Venous Thromboembolism Prophylaxis in Hospitalized Patients With Inflammatory Bowel Disease Cared for in a Safety Net Hospital
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Melissa Ho, MD
Keck School of Medicine, University of Southern California
Los Angeles, CA
Presenting Author(s)
Prachi Nene, MD1, Melissa Ho, MD2, Thu Mai, MD1, Linda Huang, MD3, John J. Kim, MD4, Sarah Sheibani, MD2
1University of Southern California (LAC + USC), Los Angeles, CA; 2Keck School of Medicine, University of Southern California, Los Angeles, CA; 3University of Southern California, Los Angeles, CA; 4Loma Linda University Medical Center, Loma Linda, CA
Introduction: Patients with inflammatory bowel disease (IBD) are at 3-fold increased risk for developing venous thromboembolism (VTE) compared with patients without IBD. VTE events have been associated with poorer outcomes in patients with IBD and carry significant morbidity and mortality. Despite guidelines recommending the use of VTE prophylaxis in patients hospitalized with IBD flares, there is minimal data on the VTE prophylaxis adherence rate in underserved IBD patients. The aim of this study is to determine the rates of pharmacologic VTE prophylaxis in flaring IBD patients hospitalized in a safety net hospital and to determine factors associated with non-adherence.
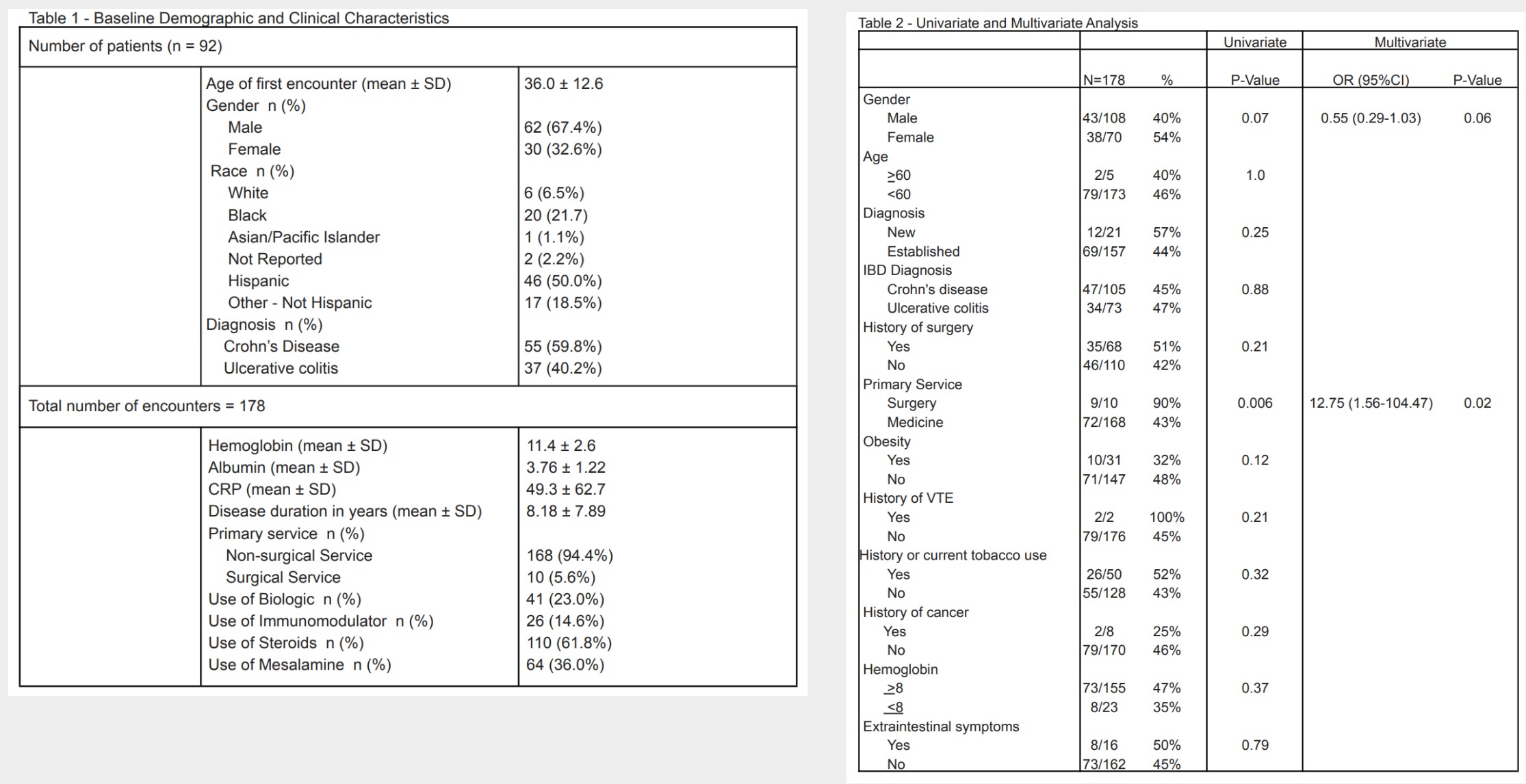
Methods: We performed a retrospective analysis of IBD patients hospitalized with a flare of symptoms between January 1, 2018 and December 31, 2020. Data abstraction included patient demographics, disease characteristics, medication use, medical comorbidities, in addition to characteristics during hospitalization including laboratory data. The medical records were reviewed to determine if pharmacologic prophylaxis was used and administered. A stepwise logistic regression was performed to identify independent predictors for the primary outcome. A univariate and multivariate logistic regression analysis was performed to determine factors associated with adherence of chemical VTE prophylaxis in this cohort.
Results: A total of 178 encounters in 92 individual patients (59.8% CD; 40.2% UC) were evaluated. In this cohort of patients, 50.0% were Hispanic, 21.7% were Black, and 6.5% were White (Table 1). The overall VTE pharmacologic prophylaxis rate of the total 178 encounters was 45.5% (81 encounters). In the multiple logistic regression analysis, being on a primary surgical service was associated with adherence to VTE prophylaxis (OR 12.75 [CI 1.56-104.47], p = 0.02) with a trend towards significance in female
patients (OR 0.55 [CI 0.29 - 1.03], p = 0.06) (Table 2).
Discussion: In IBD patients hospitalized with a flare, adherence to VTE prophylaxis was low at 45.5%. In multivariate analysis, the major predictor of non-adherence to VTE prophylaxis was primary admitting service. Quality improvement interventions are needed to improve adherence to VTE prophylaxis and prevent morbidity and mortality in this vulnerable population.
Disclosures:
Prachi Nene, MD1, Melissa Ho, MD2, Thu Mai, MD1, Linda Huang, MD3, John J. Kim, MD4, Sarah Sheibani, MD2. E0397 - Adherence to Venous Thromboembolism Prophylaxis in Hospitalized Patients With Inflammatory Bowel Disease Cared for in a Safety Net Hospital, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Southern California (LAC + USC), Los Angeles, CA; 2Keck School of Medicine, University of Southern California, Los Angeles, CA; 3University of Southern California, Los Angeles, CA; 4Loma Linda University Medical Center, Loma Linda, CA
Introduction: Patients with inflammatory bowel disease (IBD) are at 3-fold increased risk for developing venous thromboembolism (VTE) compared with patients without IBD. VTE events have been associated with poorer outcomes in patients with IBD and carry significant morbidity and mortality. Despite guidelines recommending the use of VTE prophylaxis in patients hospitalized with IBD flares, there is minimal data on the VTE prophylaxis adherence rate in underserved IBD patients. The aim of this study is to determine the rates of pharmacologic VTE prophylaxis in flaring IBD patients hospitalized in a safety net hospital and to determine factors associated with non-adherence.
Methods: We performed a retrospective analysis of IBD patients hospitalized with a flare of symptoms between January 1, 2018 and December 31, 2020. Data abstraction included patient demographics, disease characteristics, medication use, medical comorbidities, in addition to characteristics during hospitalization including laboratory data. The medical records were reviewed to determine if pharmacologic prophylaxis was used and administered. A stepwise logistic regression was performed to identify independent predictors for the primary outcome. A univariate and multivariate logistic regression analysis was performed to determine factors associated with adherence of chemical VTE prophylaxis in this cohort.
Results: A total of 178 encounters in 92 individual patients (59.8% CD; 40.2% UC) were evaluated. In this cohort of patients, 50.0% were Hispanic, 21.7% were Black, and 6.5% were White (Table 1). The overall VTE pharmacologic prophylaxis rate of the total 178 encounters was 45.5% (81 encounters). In the multiple logistic regression analysis, being on a primary surgical service was associated with adherence to VTE prophylaxis (OR 12.75 [CI 1.56-104.47], p = 0.02) with a trend towards significance in female
patients (OR 0.55 [CI 0.29 - 1.03], p = 0.06) (Table 2).
Discussion: In IBD patients hospitalized with a flare, adherence to VTE prophylaxis was low at 45.5%. In multivariate analysis, the major predictor of non-adherence to VTE prophylaxis was primary admitting service. Quality improvement interventions are needed to improve adherence to VTE prophylaxis and prevent morbidity and mortality in this vulnerable population.
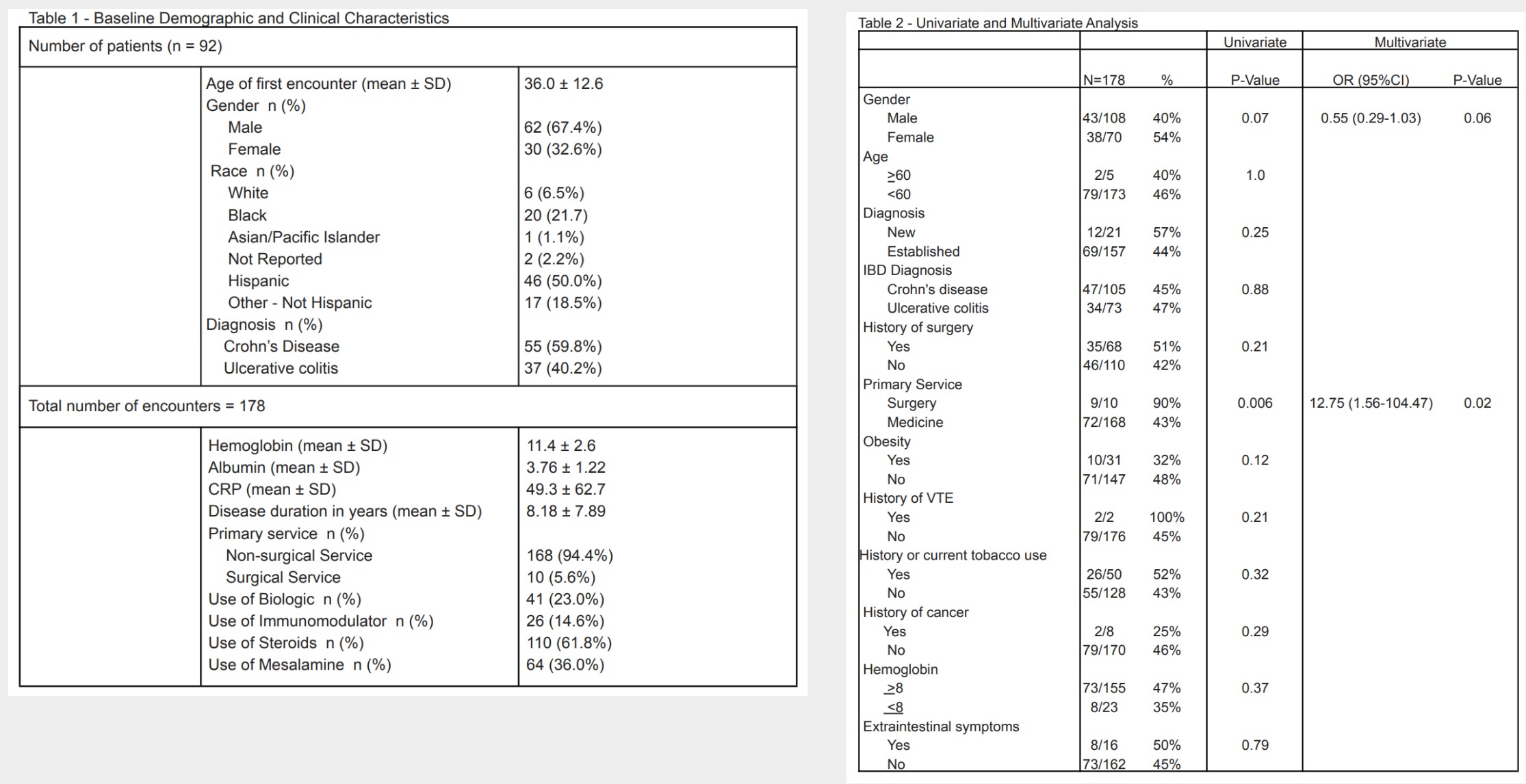
Figure: Tables
Disclosures:
Prachi Nene indicated no relevant financial relationships.
Melissa Ho indicated no relevant financial relationships.
Thu Mai indicated no relevant financial relationships.
Linda Huang indicated no relevant financial relationships.
John Kim indicated no relevant financial relationships.
Sarah Sheibani indicated no relevant financial relationships.
Prachi Nene, MD1, Melissa Ho, MD2, Thu Mai, MD1, Linda Huang, MD3, John J. Kim, MD4, Sarah Sheibani, MD2. E0397 - Adherence to Venous Thromboembolism Prophylaxis in Hospitalized Patients With Inflammatory Bowel Disease Cared for in a Safety Net Hospital, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

