Back
Poster Session E - Tuesday Afternoon
E0413 - CMV in IBD: An Innocent Bystander, or Active Pathogen?
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Michael Liben, MD
NewYork Presbyterian Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Michael Liben, MD, Karthik Chandrasekaran, MD, Douglas Sepkowitz, MD, Ofem Ajah, MD
NewYork Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Ulcerative Colitis (UC) is a gastrointestinal inflammatory disease that affects over 6 million people worldwide. Clinical manifestations of UC such as bloody diarrhea and abdominal pain can often mimic an infectious colitis, such as cytomegalovirus (CMV) colitis. Often a silent infection, CMV has a worldwide seroprevalence of 83%. We present an interesting case of a UC patient with biopsy positive CMV colitis, who symptomatically improved on steroids and mesalamine alone.
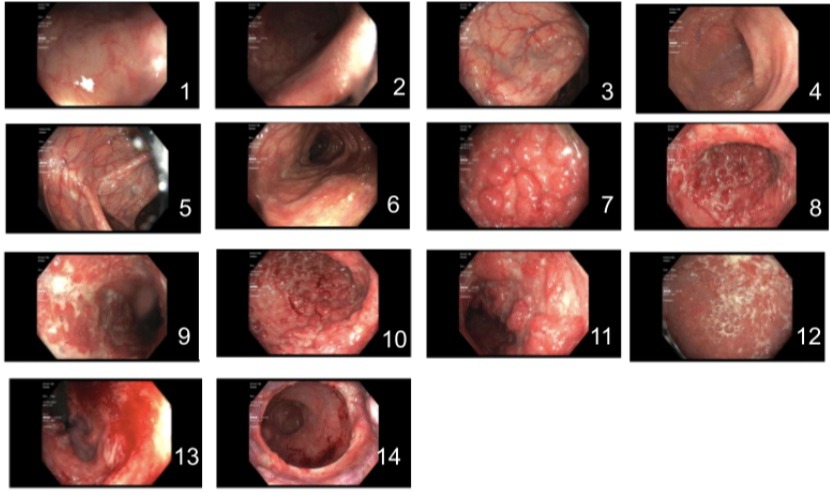
Case Description/Methods: A 66 year old African American female with a history of well-controlled UC was evaluated for acute onset bloody diarrhea and abdominal pain. Following negative stool studies for infection, the patient underwent colonoscopic evaluation. Preliminary imaging and results demonstrated a left-sided UC flare extending from the rectum to the splenic flexure. The patient was started on pulse dose steroids with instructions to taper as an outpatient and experienced resolution of symptoms. Biopsy revealed CMV with subsequent serologic testing showing a CMV viral load of < 390 cpy/mL, IgM level of 45.4 AU/mL and negative IgG levels. Interestingly, the patient's acute gastrointestinal symptoms resolved with glucocorticoid treatment.
Discussion: CMV reactivation is common in patients with moderate to severe UC. Symptoms of diarrhea, bloody stool, abdominal pain and complications such as megacolon, fulminant colitis and perforation often overlap in both CMV and UC. Endoscopic evaluation can provide a more definitive means of differentiating CMV colitis from an acute exacerbation of UC, however, may not be able to be quickly performed before complications arise.
There has been much debate on the role of CMV in UC and whether it is an active pathogen contributing to the inflammatory state or simply a surrogate marker for disease severity. Multiple studies have demonstrated an association of CMV antigenemia with endoscopically significant severe UC. In such patients, after detection of CMV in the colon with biopsy, treatment with antiviral therapy and withdrawal of immunosuppressive agents would be expected to induce clinical response. Continuation of immunosuppressive therapies was associated with adverse events such as fulminant colitis and colectomy.
Differentiating an active CMV infection versus a UC flare can be challenging given the wide overlap of symptoms. Colonoscopic evaluation is important in supplementing a diagnosis with histopathological confirmation of CMV and can help guide treatment.
Disclosures:
Michael Liben, MD, Karthik Chandrasekaran, MD, Douglas Sepkowitz, MD, Ofem Ajah, MD. E0413 - CMV in IBD: An Innocent Bystander, or Active Pathogen?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
NewYork Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Ulcerative Colitis (UC) is a gastrointestinal inflammatory disease that affects over 6 million people worldwide. Clinical manifestations of UC such as bloody diarrhea and abdominal pain can often mimic an infectious colitis, such as cytomegalovirus (CMV) colitis. Often a silent infection, CMV has a worldwide seroprevalence of 83%. We present an interesting case of a UC patient with biopsy positive CMV colitis, who symptomatically improved on steroids and mesalamine alone.
Case Description/Methods: A 66 year old African American female with a history of well-controlled UC was evaluated for acute onset bloody diarrhea and abdominal pain. Following negative stool studies for infection, the patient underwent colonoscopic evaluation. Preliminary imaging and results demonstrated a left-sided UC flare extending from the rectum to the splenic flexure. The patient was started on pulse dose steroids with instructions to taper as an outpatient and experienced resolution of symptoms. Biopsy revealed CMV with subsequent serologic testing showing a CMV viral load of < 390 cpy/mL, IgM level of 45.4 AU/mL and negative IgG levels. Interestingly, the patient's acute gastrointestinal symptoms resolved with glucocorticoid treatment.
Discussion: CMV reactivation is common in patients with moderate to severe UC. Symptoms of diarrhea, bloody stool, abdominal pain and complications such as megacolon, fulminant colitis and perforation often overlap in both CMV and UC. Endoscopic evaluation can provide a more definitive means of differentiating CMV colitis from an acute exacerbation of UC, however, may not be able to be quickly performed before complications arise.
There has been much debate on the role of CMV in UC and whether it is an active pathogen contributing to the inflammatory state or simply a surrogate marker for disease severity. Multiple studies have demonstrated an association of CMV antigenemia with endoscopically significant severe UC. In such patients, after detection of CMV in the colon with biopsy, treatment with antiviral therapy and withdrawal of immunosuppressive agents would be expected to induce clinical response. Continuation of immunosuppressive therapies was associated with adverse events such as fulminant colitis and colectomy.
Differentiating an active CMV infection versus a UC flare can be challenging given the wide overlap of symptoms. Colonoscopic evaluation is important in supplementing a diagnosis with histopathological confirmation of CMV and can help guide treatment.
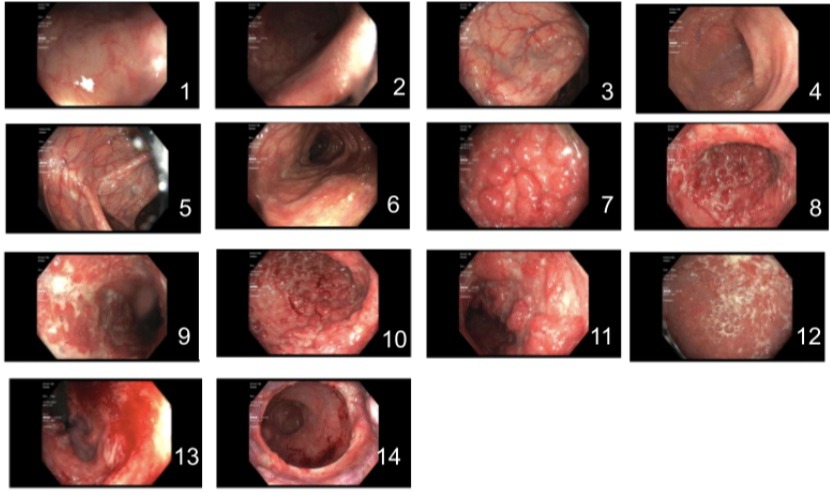
Figure: Inflammation characterized by friability, loss of vascularity, mucous, pseudopolyps and deep ulcerations was found in a continuous and circumferential pattern in the terminal ileum (1,2), hepatic flexure (3), transverse colon (4,5,6), descending colon (7,8), sigmoid colon (9,10,11), and rectum (12,13,14). This was graded as Mayo Score 3 (severe, with spontaneous bleeding, ulcerations).
Disclosures:
Michael Liben indicated no relevant financial relationships.
Karthik Chandrasekaran indicated no relevant financial relationships.
Douglas Sepkowitz indicated no relevant financial relationships.
Ofem Ajah indicated no relevant financial relationships.
Michael Liben, MD, Karthik Chandrasekaran, MD, Douglas Sepkowitz, MD, Ofem Ajah, MD. E0413 - CMV in IBD: An Innocent Bystander, or Active Pathogen?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
