Back
Poster Session C - Monday Afternoon
C0311 - Double Pylorus Secondary to Peptic Ulcer Disease
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Jared Micho, MD
Indiana University Internal Medicine Residency - Southwest
Evansville, IN
Presenting Author(s)
Jared Micho, MD1, Colin Martyn, MD2, Oluwagbenga Serrano, MD, FACG3
1Indiana University Internal Medicine Residency - Southwest, Evansville, IN; 2Indiana University Internal Medicine Residency - Southwest, Vincennes, IN; 3Good Samaritan Hospital, Vincennes, IN
Introduction: Double pylorus is an unusual endoscopic finding viewed as a fistula between the gastric antrum and duodenal bulb. The presence of double pylorus occurs in 0.001 to 0.4% of upper endoscopy procedures and is more frequent in men and those with peptic ulcer disease. We describe a 74-year-old female with prior H. pylori infection and gastroduodenal ulcerations resulting in a double pylorus.
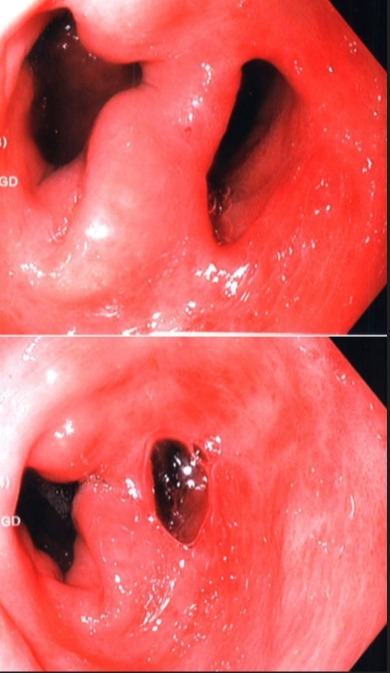
Case Description/Methods: A 74-year-old female was referred to our clinic for evaluation of dyspnea and persistent iron deficiency anemia over several months with a history of alcoholic cirrhosis, right hemicolectomy due to diverticulitis, and gastroduodenal ulcer disease in the setting of prior H. pylori infection. Her dyspnea was associated with dull pleuritic epigastric pain radiating to her back but she denied nausea, melena, hematochezia, dysphagia, odynophagia, and weight loss. She was compliant with oral iron supplementation and reported 3 years of sobriety. Vital signs and physical examination were unremarkable. CBC displayed macrocytic anemia with iron deficiency on iron panel. Abdominal CT revealed a large paraesophageal hernia and a lobular liver contour compatible with cirrhosis. Given her prior antral and duodenal ulceration, EGD was performed, which revealed antral erythema, an 11 cm hiatal hernia, and a double pylorus (Figure 1). Both ostia at the antrum were intubated separately and appeared endoscopically normal. H. pylori biopsies were negative. The patient continued proton pump inhibitor therapy without further procedural intervention.
Discussion: Most cases of double pylorus are acquired in the setting of peripyloric ulceration with resulting mucosal perforation from repetitive damage and impaired healing. After perforation occurs, a fistula can form between the gastric antrum and duodenal bulb. Common symptoms include dyspepsia, emesis, and chronic abdominal pain. Occult bleeding is common and diagnosis requires upper endoscopy to visualize each ostia of the double pylorus along the lesser curvature. Management typically consists of risk factor reduction (NSAID and corticosteroid use, H. pylori infection) and pharmacologic promotion of mucosal healing (proton pump inhibitors, H2 receptor antagonists, and antacids). Utilization of these strategies was shown in one study to close the double pylorus false lumen in 9% of cases and cause the two pylori to fuse in 27% of cases. However, 64% of patients in the same study had persistent double pylorus despite treatment.
Disclosures:
Jared Micho, MD1, Colin Martyn, MD2, Oluwagbenga Serrano, MD, FACG3. C0311 - Double Pylorus Secondary to Peptic Ulcer Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Indiana University Internal Medicine Residency - Southwest, Evansville, IN; 2Indiana University Internal Medicine Residency - Southwest, Vincennes, IN; 3Good Samaritan Hospital, Vincennes, IN
Introduction: Double pylorus is an unusual endoscopic finding viewed as a fistula between the gastric antrum and duodenal bulb. The presence of double pylorus occurs in 0.001 to 0.4% of upper endoscopy procedures and is more frequent in men and those with peptic ulcer disease. We describe a 74-year-old female with prior H. pylori infection and gastroduodenal ulcerations resulting in a double pylorus.
Case Description/Methods: A 74-year-old female was referred to our clinic for evaluation of dyspnea and persistent iron deficiency anemia over several months with a history of alcoholic cirrhosis, right hemicolectomy due to diverticulitis, and gastroduodenal ulcer disease in the setting of prior H. pylori infection. Her dyspnea was associated with dull pleuritic epigastric pain radiating to her back but she denied nausea, melena, hematochezia, dysphagia, odynophagia, and weight loss. She was compliant with oral iron supplementation and reported 3 years of sobriety. Vital signs and physical examination were unremarkable. CBC displayed macrocytic anemia with iron deficiency on iron panel. Abdominal CT revealed a large paraesophageal hernia and a lobular liver contour compatible with cirrhosis. Given her prior antral and duodenal ulceration, EGD was performed, which revealed antral erythema, an 11 cm hiatal hernia, and a double pylorus (Figure 1). Both ostia at the antrum were intubated separately and appeared endoscopically normal. H. pylori biopsies were negative. The patient continued proton pump inhibitor therapy without further procedural intervention.
Discussion: Most cases of double pylorus are acquired in the setting of peripyloric ulceration with resulting mucosal perforation from repetitive damage and impaired healing. After perforation occurs, a fistula can form between the gastric antrum and duodenal bulb. Common symptoms include dyspepsia, emesis, and chronic abdominal pain. Occult bleeding is common and diagnosis requires upper endoscopy to visualize each ostia of the double pylorus along the lesser curvature. Management typically consists of risk factor reduction (NSAID and corticosteroid use, H. pylori infection) and pharmacologic promotion of mucosal healing (proton pump inhibitors, H2 receptor antagonists, and antacids). Utilization of these strategies was shown in one study to close the double pylorus false lumen in 9% of cases and cause the two pylori to fuse in 27% of cases. However, 64% of patients in the same study had persistent double pylorus despite treatment.
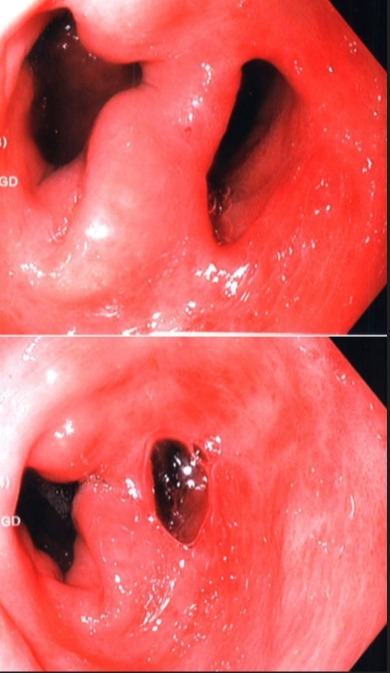
Figure: Endoscopic view of the pylorus from the antrum of the stomach
Disclosures:
Jared Micho indicated no relevant financial relationships.
Colin Martyn indicated no relevant financial relationships.
Oluwagbenga Serrano: Gilead – Independent Contractor. Merck – Stock-publicly held company(excluding mutual/index funds).
Jared Micho, MD1, Colin Martyn, MD2, Oluwagbenga Serrano, MD, FACG3. C0311 - Double Pylorus Secondary to Peptic Ulcer Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
