Back
Poster Session E - Tuesday Afternoon
E0283 - Getting to the GIST of It: Rare Case of GIST in Ascending Colon
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Deepa Kumarjiguda, DO
Geisinger Health System
Danville, PA
Presenting Author(s)
Deepa Kumarjiguda, DO1, Shreya Vatsala, MD2, Ruchit Shah, DO1, Bradley D. Confer, DO2
1Geisinger Health System, Danville, PA; 2Geisinger Medical Center, Danville, PA
Introduction: Gastrointestinal stromal tumors (GIST) are the most common mesenchymal tumor of the gastrointestinal (GI) tract. GIST is most localized in the stomach (50 – 60%), followed by the small intestine (30 – 40%), and the colon (5-10%). Herein we describe a unique case of an ascending colon GIST requiring advanced endoscopic dissection to confirm the diagnosis.
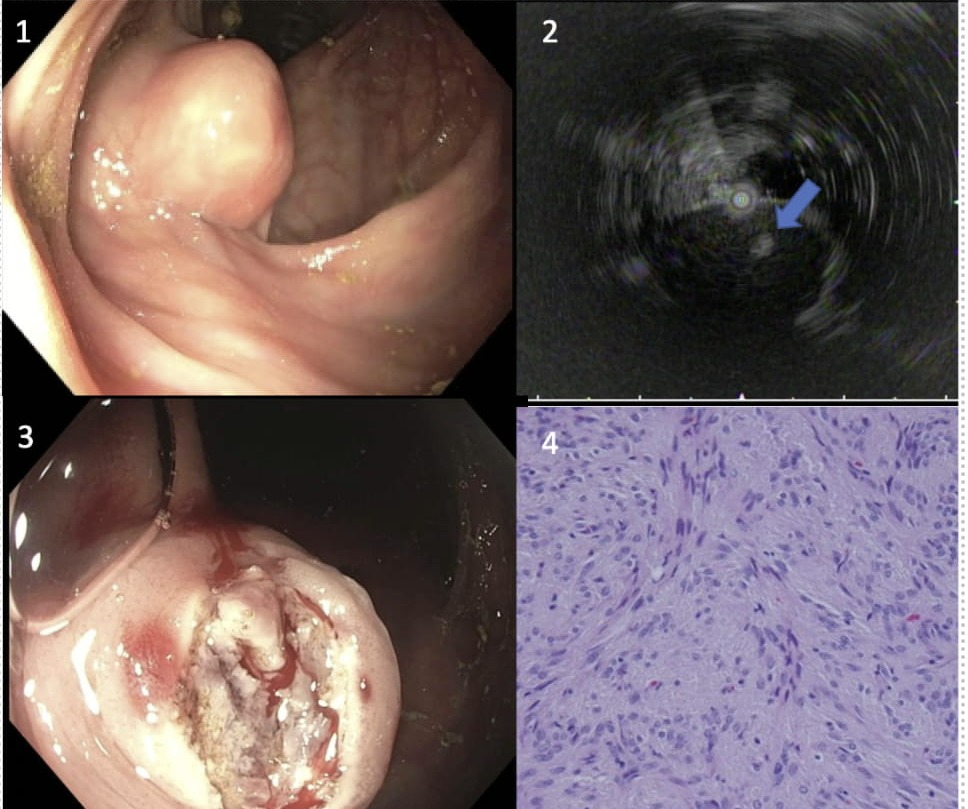
Case Description/Methods: A 78-year-old male presented with generalized abdominal discomfort associated with heartburn and for colon cancer screening. The upper endoscopy was unremarkable. On colonoscopy, a 4 cm subepithelial lesion was found in the ascending colon (Fig 1). Traditional endoscopic ultrasound (EUS) using a linear or forward viewing scope was not possible given the redundant sigmoid colon, leading to significant scope-looping. The lumen was filled with water and the miniprobe ultrasound catheter was advanced through the working channel of the colonoscope to assess the lesion. Ultrasound revealed a heterogenous, hypoechoic 4 by 3 cm lesion arising from the muscularis propria, suggestive of a mesenchymal tumor (Fig 2). Dissection of the middle portion of the lesion was completed using needle-knife to the muscularis propria and biopsy forceps were used to obtain deep biopsy (Fig 3). A clip was placed due to the small increased risk of delayed bleeding or perforation. Histopathology was positive for CD117, DOG-1, CD34, and h-caldesmon and stains negative for S100, GFAP, and SMA, consistent with GIST (Fig 4).
Further imaging of chest, abdomen, pelvis did not show metastatic disease. Surgical evaluation was recommended due to size, heterogeneous appearance on EUS and colonic origin. The patient underwent a right hemicolectomy. Pathology confirmed a low mitotic GIST. The post operative period was uneventful, and he was discharged home. He did not require adjuvant imatinib.
Discussion: Tumor size, mitotic rate, and location have been studied and used as prognostication factors to predict degree of malignancy potential in GIST but is only validated in gastric and small intestinal tumors. Knowledge is limited regarding colonic tumors versus antral tumors since occurrence is rare. Current data suggest colonic tumors are more malignant. Due to the unusual location of the subepithelial lesion and redundant colon, traditional EUS would not work to biopsy the lesion. Needle knife dissection assists in identifying and finding cancerous lesions in challenging situations.
Disclosures:
Deepa Kumarjiguda, DO1, Shreya Vatsala, MD2, Ruchit Shah, DO1, Bradley D. Confer, DO2. E0283 - Getting to the GIST of It: Rare Case of GIST in Ascending Colon, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Geisinger Health System, Danville, PA; 2Geisinger Medical Center, Danville, PA
Introduction: Gastrointestinal stromal tumors (GIST) are the most common mesenchymal tumor of the gastrointestinal (GI) tract. GIST is most localized in the stomach (50 – 60%), followed by the small intestine (30 – 40%), and the colon (5-10%). Herein we describe a unique case of an ascending colon GIST requiring advanced endoscopic dissection to confirm the diagnosis.
Case Description/Methods: A 78-year-old male presented with generalized abdominal discomfort associated with heartburn and for colon cancer screening. The upper endoscopy was unremarkable. On colonoscopy, a 4 cm subepithelial lesion was found in the ascending colon (Fig 1). Traditional endoscopic ultrasound (EUS) using a linear or forward viewing scope was not possible given the redundant sigmoid colon, leading to significant scope-looping. The lumen was filled with water and the miniprobe ultrasound catheter was advanced through the working channel of the colonoscope to assess the lesion. Ultrasound revealed a heterogenous, hypoechoic 4 by 3 cm lesion arising from the muscularis propria, suggestive of a mesenchymal tumor (Fig 2). Dissection of the middle portion of the lesion was completed using needle-knife to the muscularis propria and biopsy forceps were used to obtain deep biopsy (Fig 3). A clip was placed due to the small increased risk of delayed bleeding or perforation. Histopathology was positive for CD117, DOG-1, CD34, and h-caldesmon and stains negative for S100, GFAP, and SMA, consistent with GIST (Fig 4).
Further imaging of chest, abdomen, pelvis did not show metastatic disease. Surgical evaluation was recommended due to size, heterogeneous appearance on EUS and colonic origin. The patient underwent a right hemicolectomy. Pathology confirmed a low mitotic GIST. The post operative period was uneventful, and he was discharged home. He did not require adjuvant imatinib.
Discussion: Tumor size, mitotic rate, and location have been studied and used as prognostication factors to predict degree of malignancy potential in GIST but is only validated in gastric and small intestinal tumors. Knowledge is limited regarding colonic tumors versus antral tumors since occurrence is rare. Current data suggest colonic tumors are more malignant. Due to the unusual location of the subepithelial lesion and redundant colon, traditional EUS would not work to biopsy the lesion. Needle knife dissection assists in identifying and finding cancerous lesions in challenging situations.
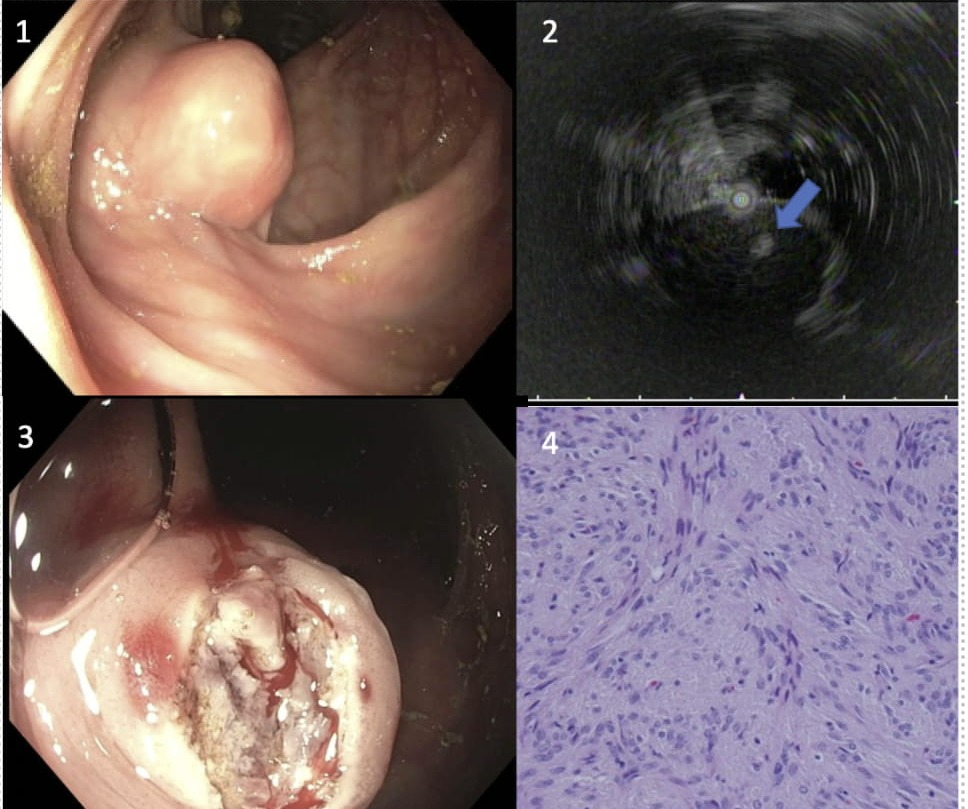
Figure: Figure 1. Endoscopic image of colonic subepithelial lesion
Figure 2. EUS demonstrates hypoechoic lesion with small hyperechoic area (blue arrow) in the center of the lesion
Figure 3. Post needle-knife dissection and biopsy
Figure 4. Histopathology reveals spindle cell morphology confirming GIST along with correlating diagnostic stains on H&E stain.
Figure 2. EUS demonstrates hypoechoic lesion with small hyperechoic area (blue arrow) in the center of the lesion
Figure 3. Post needle-knife dissection and biopsy
Figure 4. Histopathology reveals spindle cell morphology confirming GIST along with correlating diagnostic stains on H&E stain.
Disclosures:
Deepa Kumarjiguda indicated no relevant financial relationships.
Shreya Vatsala indicated no relevant financial relationships.
Ruchit Shah indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Deepa Kumarjiguda, DO1, Shreya Vatsala, MD2, Ruchit Shah, DO1, Bradley D. Confer, DO2. E0283 - Getting to the GIST of It: Rare Case of GIST in Ascending Colon, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

