Back
Poster Session D - Tuesday Morning
D0330 - The Eroding Ulcer
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom

Maurice Marcuard, MD
Hackensack University Medical Center
Hackensack, NJ
Presenting Author(s)
Maurice Marcuard, MD, Ali Alshati, MD, Nathan Campbell, MD, Ali Sedarat, MD
Hackensack University Medical Center, Hackensack, NJ
Introduction: Massive upper gastrointestinal (GI) bleeds can be life threatening. Common causes are peptic ulcer disease and esophagogastric varices. These, when presented, often can be managed endoscopically. Ulcers in the GI tract can, rarely, erode into major arteries including the splenic artery and cause bleeding that may need embolization or surgery to control. Here we report a case of a massive upper GI bleed.
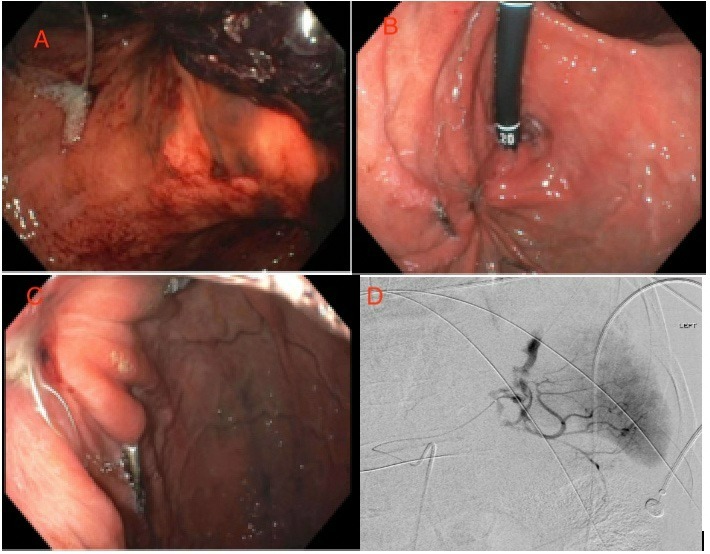
Case Description/Methods: Patient is a 65 year old male with PMH of alcohol abuse, drug use, bed bound who presented with reported hematemesis. Initially patient reported he drank red liquid prior and refused an endoscopy. A day into hospitalization he had another episode of hematemesis and hypotension and was transferred to the ICU. There he transfused and stabilized. He underwent an endoscopy discovering a gastric ulcer in the fundus. Epinephrine was injected with good effect and cautery was initiated with bipolar probe starting at the periphery of the visible vessel and on the edges of the ulcer. While performing cautery, the vessel in the ulcer started to hemorrhage causing red out and inability to visualize. He was intubated and started massive transfusion protocol. Interventional radiology (IR) and surgery was consulted. He had three cardiac arrests with rapid return of pulse. When he made it to the IR suite, underwent angiography which showing significant bleeding from mid splenic artery which was coiled (d). With the location the ulcer had eroded into the splenic artery causing a fistula. He recovered well and was later discharged from the hospital. He underwent a repeat endoscopy a few days later (a) and another a few weeks after discharge (b,c).
Discussion: Often with vascular fistulas there is an initial small bleed followed by a more significant bleed as seen in this case. When encountering massive GI bleeding, one must keep enteric vascular fistulas in the differential and have interventional radiology and surgery engaged early. Presenting with a splenic artery aneurysm with bleeding is rare, 0.01 to 10.4% depending on literature. Hemorrhage is one of the most common presentation for splenic artery pseudoaneurysms with 47% of cases and mortality approaches 90% if not properly managed. This case reminds us to keep a broad differential and to involve IR and surgery early in a massive GI bleed.
Disclosures:
Maurice Marcuard, MD, Ali Alshati, MD, Nathan Campbell, MD, Ali Sedarat, MD. D0330 - The Eroding Ulcer, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Hackensack University Medical Center, Hackensack, NJ
Introduction: Massive upper gastrointestinal (GI) bleeds can be life threatening. Common causes are peptic ulcer disease and esophagogastric varices. These, when presented, often can be managed endoscopically. Ulcers in the GI tract can, rarely, erode into major arteries including the splenic artery and cause bleeding that may need embolization or surgery to control. Here we report a case of a massive upper GI bleed.
Case Description/Methods: Patient is a 65 year old male with PMH of alcohol abuse, drug use, bed bound who presented with reported hematemesis. Initially patient reported he drank red liquid prior and refused an endoscopy. A day into hospitalization he had another episode of hematemesis and hypotension and was transferred to the ICU. There he transfused and stabilized. He underwent an endoscopy discovering a gastric ulcer in the fundus. Epinephrine was injected with good effect and cautery was initiated with bipolar probe starting at the periphery of the visible vessel and on the edges of the ulcer. While performing cautery, the vessel in the ulcer started to hemorrhage causing red out and inability to visualize. He was intubated and started massive transfusion protocol. Interventional radiology (IR) and surgery was consulted. He had three cardiac arrests with rapid return of pulse. When he made it to the IR suite, underwent angiography which showing significant bleeding from mid splenic artery which was coiled (d). With the location the ulcer had eroded into the splenic artery causing a fistula. He recovered well and was later discharged from the hospital. He underwent a repeat endoscopy a few days later (a) and another a few weeks after discharge (b,c).
Discussion: Often with vascular fistulas there is an initial small bleed followed by a more significant bleed as seen in this case. When encountering massive GI bleeding, one must keep enteric vascular fistulas in the differential and have interventional radiology and surgery engaged early. Presenting with a splenic artery aneurysm with bleeding is rare, 0.01 to 10.4% depending on literature. Hemorrhage is one of the most common presentation for splenic artery pseudoaneurysms with 47% of cases and mortality approaches 90% if not properly managed. This case reminds us to keep a broad differential and to involve IR and surgery early in a massive GI bleed.
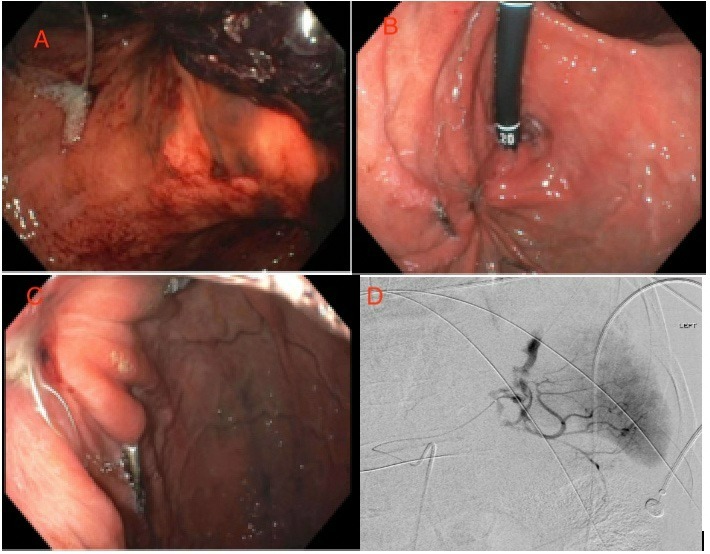
Figure: A.Endoscopy post coiling with coil emerging from ulcer. B. Endoscopy after discharge. C. Endoscopy after discharge, coils still present from ulcer. D. Angiogram showing active bleeding
Disclosures:
Maurice Marcuard indicated no relevant financial relationships.
Ali Alshati indicated no relevant financial relationships.
Nathan Campbell indicated no relevant financial relationships.
Ali Sedarat indicated no relevant financial relationships.
Maurice Marcuard, MD, Ali Alshati, MD, Nathan Campbell, MD, Ali Sedarat, MD. D0330 - The Eroding Ulcer, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
