Back
Poster Session E - Tuesday Afternoon
E0336 - Upper Gastrointestinal Bleeding Due to Duodenal Ischemia: A Case Series
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Parth Desai, DO
Tower Health - Reading Hospital
Reading, PA
Presenting Author(s)
Parth Desai, DO1, Jesus Salas Noain, MD1, Anish Paudel, MD1, Ameya Deshmukh, DO2, Biraj Shrestha, MD1, Kevin Gordon, MD1
1Tower Health - Reading Hospital, Reading, PA; 2Saint Louis University School of Medicine, St. Louis, MO
Introduction: Duodenal ischemia is a rare entity given dual blood supply from branches of the Celiac axis and Superior Mesenteric artery. However, it may present with clinically significant GI bleeding. We present three cases of duodenal ischemia diagnosed on EGD.
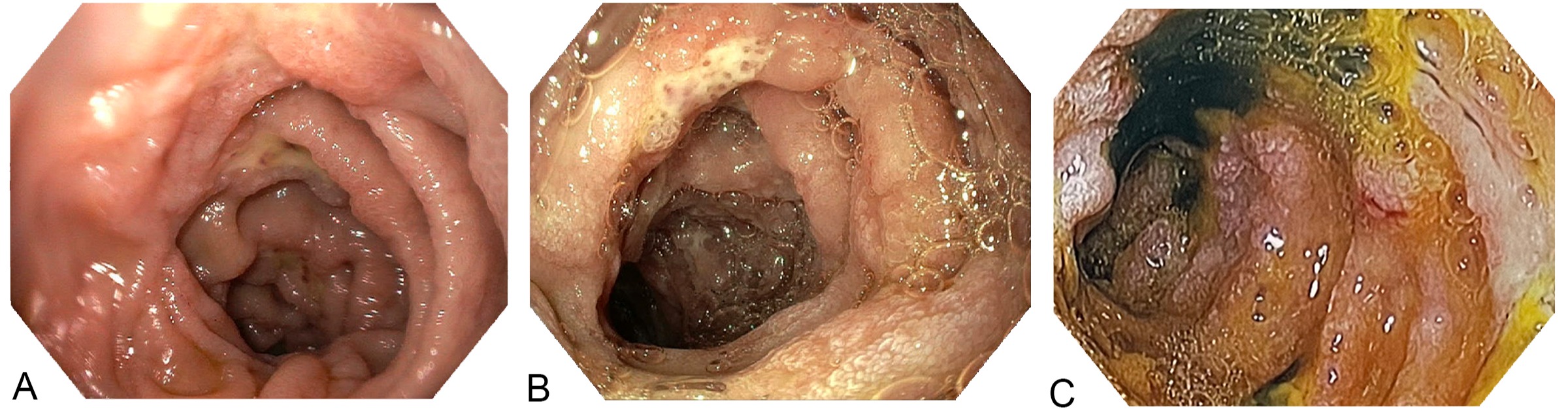
Case Description/Methods: Case 1: An 84-year-old lady with heart failure presented with abdominal pain and melena. Vitals were BP 90/55, HR 112. She was cachectic with a mildly tender abdomen. Labs were notable for hemoglobin 6.6 g/dL from baseline of 8.2; BUN 65 mg/dL. CT abdomen noted bowel wall edema involving the duodenum. EGD revealed 5 duodenal ulcers with surrounding erythematous and friable mucosa consistent with ischemia (Figure 1A). She was discharged in stable condition on pantoprazole BID.
Case 2: A 63-year-old lady presented with chest pain and was diagnosed with an inferior STEMI. On presentation vitals were BP 76/50 mmHg and HR 43 bpm. Cardiac catheterization was performed with two drug-eluting stents placed in the right coronary artery. Patient was started on aspirin and clopidogrel and developed melena 3 days later. Hemoglobin dripped from 12.4 to 8.4 g/dL. EGD noted pallor of the gastric body with areas of patchy erythema and erosions within the antrum, in addition to several clean based ulcers with erythema within the duodenal bulb through the second portion (Figure 1B). Admission CT abdomen showed moderate celiac narrowing. Patient was continued on pantoprazole BID and did not have further bleeding episodes prior to discharge.
Case 3: A 63-year-old man with ESRD was admitted with endocarditis, MSSA bacteremia and embolic strokes. On day 9, he suffered PEA arrest and was resuscitated. He subsequently developed melena and shock. Hemoglobin dropped from 9.8 g/dL to 6.6 g/dL. Urgent EGD revealed a diffusely hemorrhagic stomach and the duodenum was noted to have spotty areas of necrosis, erosions and ulcerations within the bulb and second portion (Figure 1C). CTA revealed moderate to severe stenosis in the proximal SMA and celiac axis. The patient was transitioned to comfort measures after suffering recurrent embolic strokes during admission.
Discussion: Clinicians should maintain a high index of suspicion for duodenal ischemia in patients presenting with upper GI bleeding in the setting of a low-flow state, as illustrated in the above three cases. Management is typically supportive; however prognosis may be poor reflecting patients’ systemic illnesses leading to the process.
Disclosures:
Parth Desai, DO1, Jesus Salas Noain, MD1, Anish Paudel, MD1, Ameya Deshmukh, DO2, Biraj Shrestha, MD1, Kevin Gordon, MD1. E0336 - Upper Gastrointestinal Bleeding Due to Duodenal Ischemia: A Case Series, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Tower Health - Reading Hospital, Reading, PA; 2Saint Louis University School of Medicine, St. Louis, MO
Introduction: Duodenal ischemia is a rare entity given dual blood supply from branches of the Celiac axis and Superior Mesenteric artery. However, it may present with clinically significant GI bleeding. We present three cases of duodenal ischemia diagnosed on EGD.
Case Description/Methods: Case 1: An 84-year-old lady with heart failure presented with abdominal pain and melena. Vitals were BP 90/55, HR 112. She was cachectic with a mildly tender abdomen. Labs were notable for hemoglobin 6.6 g/dL from baseline of 8.2; BUN 65 mg/dL. CT abdomen noted bowel wall edema involving the duodenum. EGD revealed 5 duodenal ulcers with surrounding erythematous and friable mucosa consistent with ischemia (Figure 1A). She was discharged in stable condition on pantoprazole BID.
Case 2: A 63-year-old lady presented with chest pain and was diagnosed with an inferior STEMI. On presentation vitals were BP 76/50 mmHg and HR 43 bpm. Cardiac catheterization was performed with two drug-eluting stents placed in the right coronary artery. Patient was started on aspirin and clopidogrel and developed melena 3 days later. Hemoglobin dripped from 12.4 to 8.4 g/dL. EGD noted pallor of the gastric body with areas of patchy erythema and erosions within the antrum, in addition to several clean based ulcers with erythema within the duodenal bulb through the second portion (Figure 1B). Admission CT abdomen showed moderate celiac narrowing. Patient was continued on pantoprazole BID and did not have further bleeding episodes prior to discharge.
Case 3: A 63-year-old man with ESRD was admitted with endocarditis, MSSA bacteremia and embolic strokes. On day 9, he suffered PEA arrest and was resuscitated. He subsequently developed melena and shock. Hemoglobin dropped from 9.8 g/dL to 6.6 g/dL. Urgent EGD revealed a diffusely hemorrhagic stomach and the duodenum was noted to have spotty areas of necrosis, erosions and ulcerations within the bulb and second portion (Figure 1C). CTA revealed moderate to severe stenosis in the proximal SMA and celiac axis. The patient was transitioned to comfort measures after suffering recurrent embolic strokes during admission.
Discussion: Clinicians should maintain a high index of suspicion for duodenal ischemia in patients presenting with upper GI bleeding in the setting of a low-flow state, as illustrated in the above three cases. Management is typically supportive; however prognosis may be poor reflecting patients’ systemic illnesses leading to the process.
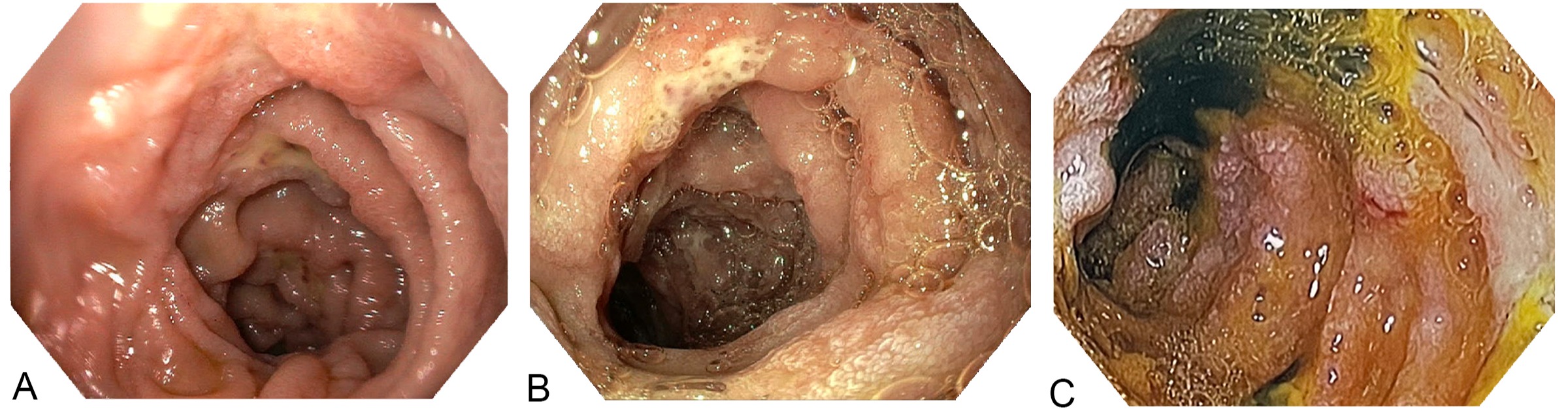
Figure: Endoscopic images demonstrating duodenal ischemia
Disclosures:
Parth Desai indicated no relevant financial relationships.
Jesus Salas Noain indicated no relevant financial relationships.
Anish Paudel indicated no relevant financial relationships.
Ameya Deshmukh indicated no relevant financial relationships.
Biraj Shrestha indicated no relevant financial relationships.
Kevin Gordon indicated no relevant financial relationships.
Parth Desai, DO1, Jesus Salas Noain, MD1, Anish Paudel, MD1, Ameya Deshmukh, DO2, Biraj Shrestha, MD1, Kevin Gordon, MD1. E0336 - Upper Gastrointestinal Bleeding Due to Duodenal Ischemia: A Case Series, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
