Back
Poster Session E - Tuesday Afternoon
E0339 - Massive Lower Gastrointestinal Bleeding From a Cholecysto-Colonic Fistula
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Bryan Wey, MD
Robert Wood Johnson University Hospital
New Brunswick, NJ
Presenting Author(s)
Bryan Wey, MD1, Kapil Gupta, MD2, Keerthana Kesavarapu, DO2, Anish Vinit Patel, MD2
1Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: Gastrointestinal bleeds are a common but potentially life-threatening presentation to the inpatient setting. Hemorrhage in the biliary system can sometimes be the underlying source. Fistula formation between the gallbladder and bowel/colon can be a rare complication of chronic and advanced gallstone disease, with cholecysto-colonic fistulae occurring in 0.06 to 0.14% of cases. A bleed in such instances makes localization a clinical challenge without the aid of angiography or endoscopy.
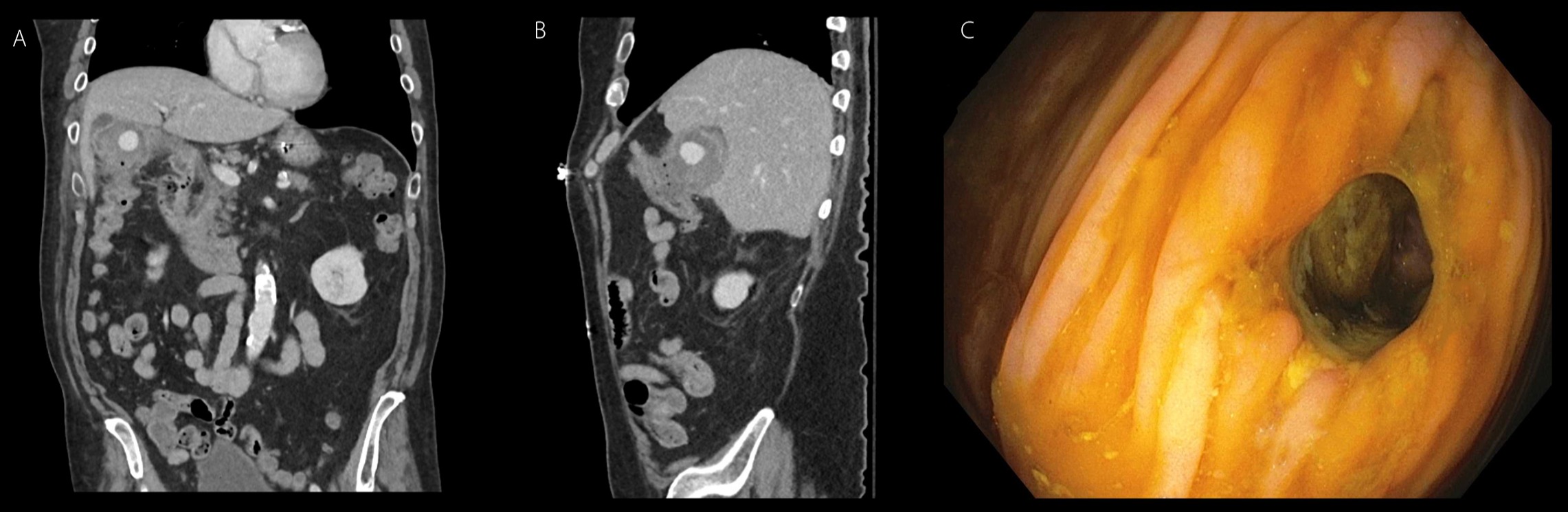
Case Description/Methods: A 78-year-old Caucasian male with a past medical history of coronary artery disease on dual antiplatelet therapy, hyperlipidemia, and type II diabetes mellitus presented to the hospital with two days of large-volume hematochezia. He was in hemorrhagic shock with a blood pressure of 66/34 mmHg, and hemoglobin 6.2 g/dL. He was rapidly resuscitated with 4 units of packed red blood cells and taken for computed tomography angiography (CTA) of the abdomen and pelvis. The scan revealed active contrast extravasation in the area of the gallbladder and hepatic flexure, originating from the cystic artery, with a local 5.6 x 5.1 cm hematoma containing foci of air, suggestive of a communication with the bowel (Figures A and B). The patient underwent successful embolization of the cystic artery by interventional radiology. Hepatobiliary iminodiacetic acid (HIDA) scan revealed cystic duct obstruction. Colonoscopy identified an 8 mm fistula at the hepatic flexure (Figure C). The patient remained hemodynamically stable with no further hematochezia and was discharged with outpatient surgical follow-up for cholecystectomy and right hemicolectomy.
Discussion: We present here a case of massive lower gastrointestinal bleeding due to a cholecysto-colonic fistula. With improved diagnosis and treatment of cholecystitis, complications of advanced gallstone disease are rarely seen today. Cholecysto-colonic or cholecysto-enteric fistulas lack common symptoms and are mainly diagnosed during abdominal surgery. Complications include biliary sepsis and peritonitis. Gastrointestinal bleeding in the setting of fistulizing disease can occur and makes early diagnosis challenging, though angiography, cholangiography and endoscopy prove to be beneficial. Awareness of this entity and early recognition can prevent catastrophic outcomes. No consensus exists regarding optimal treatment. Management ranges from minimally invasive procedures including endoscopic fistula closure to extensive surgery.
Disclosures:
Bryan Wey, MD1, Kapil Gupta, MD2, Keerthana Kesavarapu, DO2, Anish Vinit Patel, MD2. E0339 - Massive Lower Gastrointestinal Bleeding From a Cholecysto-Colonic Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: Gastrointestinal bleeds are a common but potentially life-threatening presentation to the inpatient setting. Hemorrhage in the biliary system can sometimes be the underlying source. Fistula formation between the gallbladder and bowel/colon can be a rare complication of chronic and advanced gallstone disease, with cholecysto-colonic fistulae occurring in 0.06 to 0.14% of cases. A bleed in such instances makes localization a clinical challenge without the aid of angiography or endoscopy.
Case Description/Methods: A 78-year-old Caucasian male with a past medical history of coronary artery disease on dual antiplatelet therapy, hyperlipidemia, and type II diabetes mellitus presented to the hospital with two days of large-volume hematochezia. He was in hemorrhagic shock with a blood pressure of 66/34 mmHg, and hemoglobin 6.2 g/dL. He was rapidly resuscitated with 4 units of packed red blood cells and taken for computed tomography angiography (CTA) of the abdomen and pelvis. The scan revealed active contrast extravasation in the area of the gallbladder and hepatic flexure, originating from the cystic artery, with a local 5.6 x 5.1 cm hematoma containing foci of air, suggestive of a communication with the bowel (Figures A and B). The patient underwent successful embolization of the cystic artery by interventional radiology. Hepatobiliary iminodiacetic acid (HIDA) scan revealed cystic duct obstruction. Colonoscopy identified an 8 mm fistula at the hepatic flexure (Figure C). The patient remained hemodynamically stable with no further hematochezia and was discharged with outpatient surgical follow-up for cholecystectomy and right hemicolectomy.
Discussion: We present here a case of massive lower gastrointestinal bleeding due to a cholecysto-colonic fistula. With improved diagnosis and treatment of cholecystitis, complications of advanced gallstone disease are rarely seen today. Cholecysto-colonic or cholecysto-enteric fistulas lack common symptoms and are mainly diagnosed during abdominal surgery. Complications include biliary sepsis and peritonitis. Gastrointestinal bleeding in the setting of fistulizing disease can occur and makes early diagnosis challenging, though angiography, cholangiography and endoscopy prove to be beneficial. Awareness of this entity and early recognition can prevent catastrophic outcomes. No consensus exists regarding optimal treatment. Management ranges from minimally invasive procedures including endoscopic fistula closure to extensive surgery.
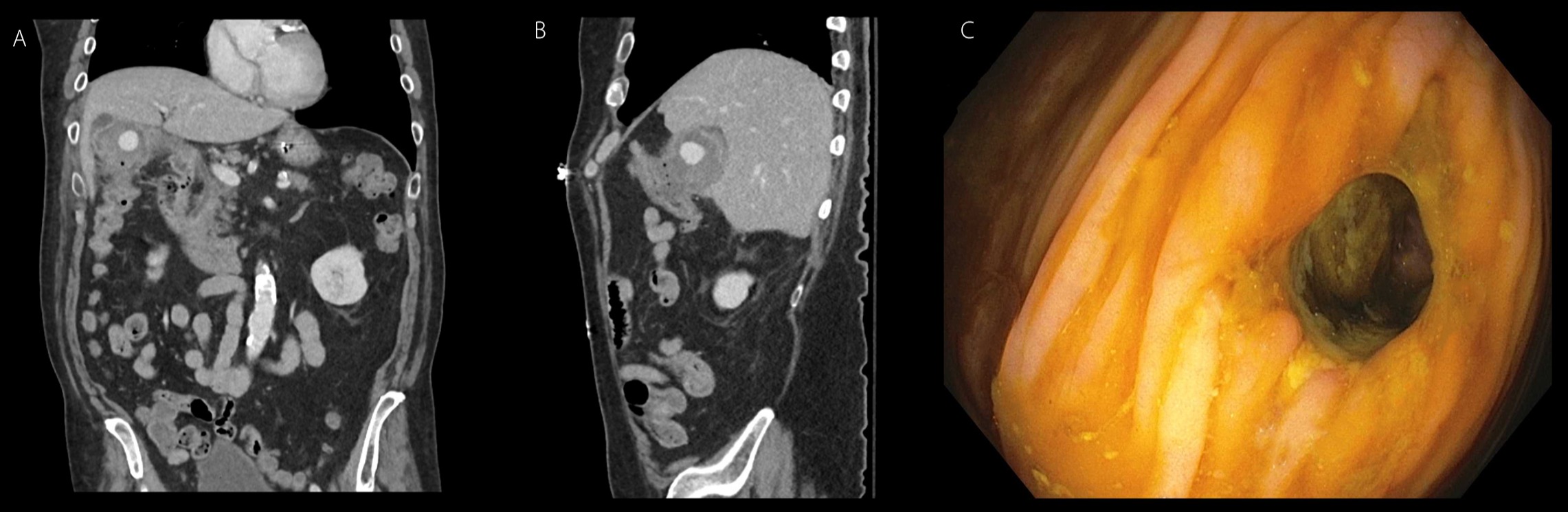
Figure: Figures A and B. Contrast extravasation from the cystic artery. The local hematoma contains foci of air, suggestive of communication with bowel/colon.
Figure C. Fistula at the hepatic flexure as noted on colonoscopy.
Figure C. Fistula at the hepatic flexure as noted on colonoscopy.
Disclosures:
Bryan Wey indicated no relevant financial relationships.
Kapil Gupta indicated no relevant financial relationships.
Keerthana Kesavarapu indicated no relevant financial relationships.
Anish Vinit Patel indicated no relevant financial relationships.
Bryan Wey, MD1, Kapil Gupta, MD2, Keerthana Kesavarapu, DO2, Anish Vinit Patel, MD2. E0339 - Massive Lower Gastrointestinal Bleeding From a Cholecysto-Colonic Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
