Back
Poster Session E - Tuesday Afternoon
E0297 - Outcomes of Patients With History of Stroke, Pulmonary Embolism, Deep Vein Thrombosis, Atrial Fibrillation, and Myocardial Infarction Who Present With a Diverticular Bleed
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Alexander Le, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Alexander Le, MD, Anmol Mittal, MD, Aaron Kahlam, MD, Sushil Ahlawat, MD
Rutgers New Jersey Medical School, Newark, NJ
Introduction: 3-15% of individuals with diverticular disease will have acute bleeding. One well documented risk factor is the use of anticoagulation medication. Most patients who have a history of vascular diseases such as stroke, pulmonary embolism (PE), deep vein thrombosis (DVT), atrial fibrillation/flutter, and myocardial infarction (MI) are on prolonged courses of anticoagulation. However, the outcome of this population presenting with diverticular bleeding remains poorly understood. Our research aims to look at this population’s mortality, length of stay (LOS), and the rate of therapeutic colonoscopy when presenting with diverticular bleeding.
Methods: The Nationwide Inpatient Sample (NIS) 2001-2013 database was queried for patients with a primary diagnosis of diverticulitis and diverticulosis with hemorrhage using International Classification of Diseases, Ninth Revision (ICD-9) codes. Patients with a history of stroke, DVT, PE, atrial fibrillation/flutter, and MI were identified using ICD-9 codes. A logistic regression analysis with data adjusted for demographics was performed on the comorbidities, with a< 0.005.
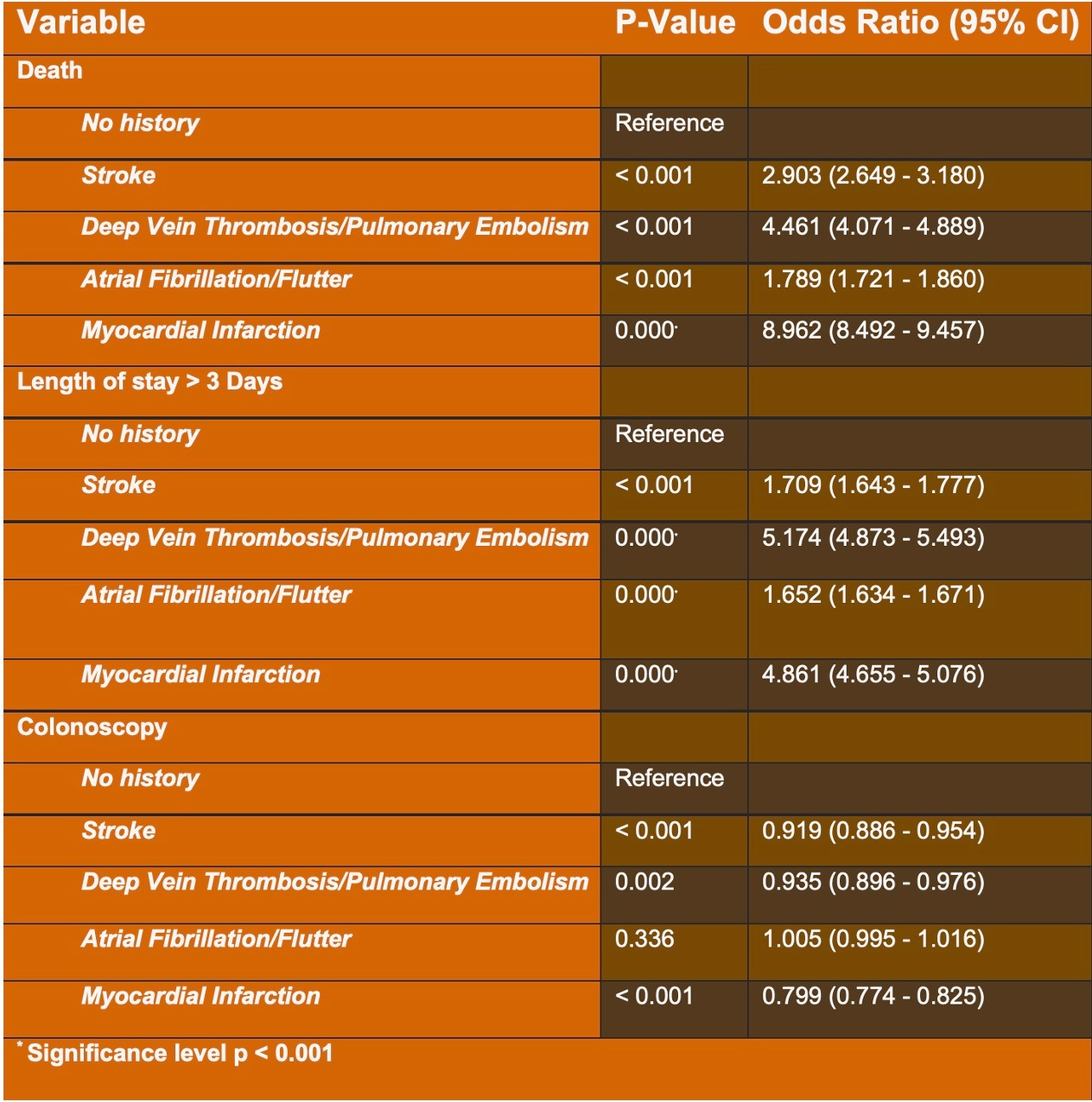
Results: Patients with a history of MI had the highest odds ratio (OR) of death at 8.962, while those with stroke had the lowest OR at 2.903. Patients with a history of DVT or PE had the highest OR of 4.873 for LOS greater than 3 days, while those with atrial fibrillation/flutter had the lowest OR of 1.634. Finally, stroke, DVT/PE, atrial fibrillation/flutter, and myocardial infarction all had a lower OR of undergoing colonoscopy.
Discussion: Having a vascular-related comorbidity increased the average LOS and mortality when presenting with diverticular bleeding. Additionally, these comorbidities also decrease the likelihood of undergoing colonoscopy during a diverticular bleeding event. This may be due to the increased volume and prolonged time of hemorrhage secondary to anticoagulation use, leading to the need for interventional radiology embolization. Future studies should investigate diverticular bleeding outcomes of this population based on different anticoagulation therapy.
Disclosures:
Alexander Le, MD, Anmol Mittal, MD, Aaron Kahlam, MD, Sushil Ahlawat, MD. E0297 - Outcomes of Patients With History of Stroke, Pulmonary Embolism, Deep Vein Thrombosis, Atrial Fibrillation, and Myocardial Infarction Who Present With a Diverticular Bleed, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Rutgers New Jersey Medical School, Newark, NJ
Introduction: 3-15% of individuals with diverticular disease will have acute bleeding. One well documented risk factor is the use of anticoagulation medication. Most patients who have a history of vascular diseases such as stroke, pulmonary embolism (PE), deep vein thrombosis (DVT), atrial fibrillation/flutter, and myocardial infarction (MI) are on prolonged courses of anticoagulation. However, the outcome of this population presenting with diverticular bleeding remains poorly understood. Our research aims to look at this population’s mortality, length of stay (LOS), and the rate of therapeutic colonoscopy when presenting with diverticular bleeding.
Methods: The Nationwide Inpatient Sample (NIS) 2001-2013 database was queried for patients with a primary diagnosis of diverticulitis and diverticulosis with hemorrhage using International Classification of Diseases, Ninth Revision (ICD-9) codes. Patients with a history of stroke, DVT, PE, atrial fibrillation/flutter, and MI were identified using ICD-9 codes. A logistic regression analysis with data adjusted for demographics was performed on the comorbidities, with a< 0.005.
Results: Patients with a history of MI had the highest odds ratio (OR) of death at 8.962, while those with stroke had the lowest OR at 2.903. Patients with a history of DVT or PE had the highest OR of 4.873 for LOS greater than 3 days, while those with atrial fibrillation/flutter had the lowest OR of 1.634. Finally, stroke, DVT/PE, atrial fibrillation/flutter, and myocardial infarction all had a lower OR of undergoing colonoscopy.
Discussion: Having a vascular-related comorbidity increased the average LOS and mortality when presenting with diverticular bleeding. Additionally, these comorbidities also decrease the likelihood of undergoing colonoscopy during a diverticular bleeding event. This may be due to the increased volume and prolonged time of hemorrhage secondary to anticoagulation use, leading to the need for interventional radiology embolization. Future studies should investigate diverticular bleeding outcomes of this population based on different anticoagulation therapy.
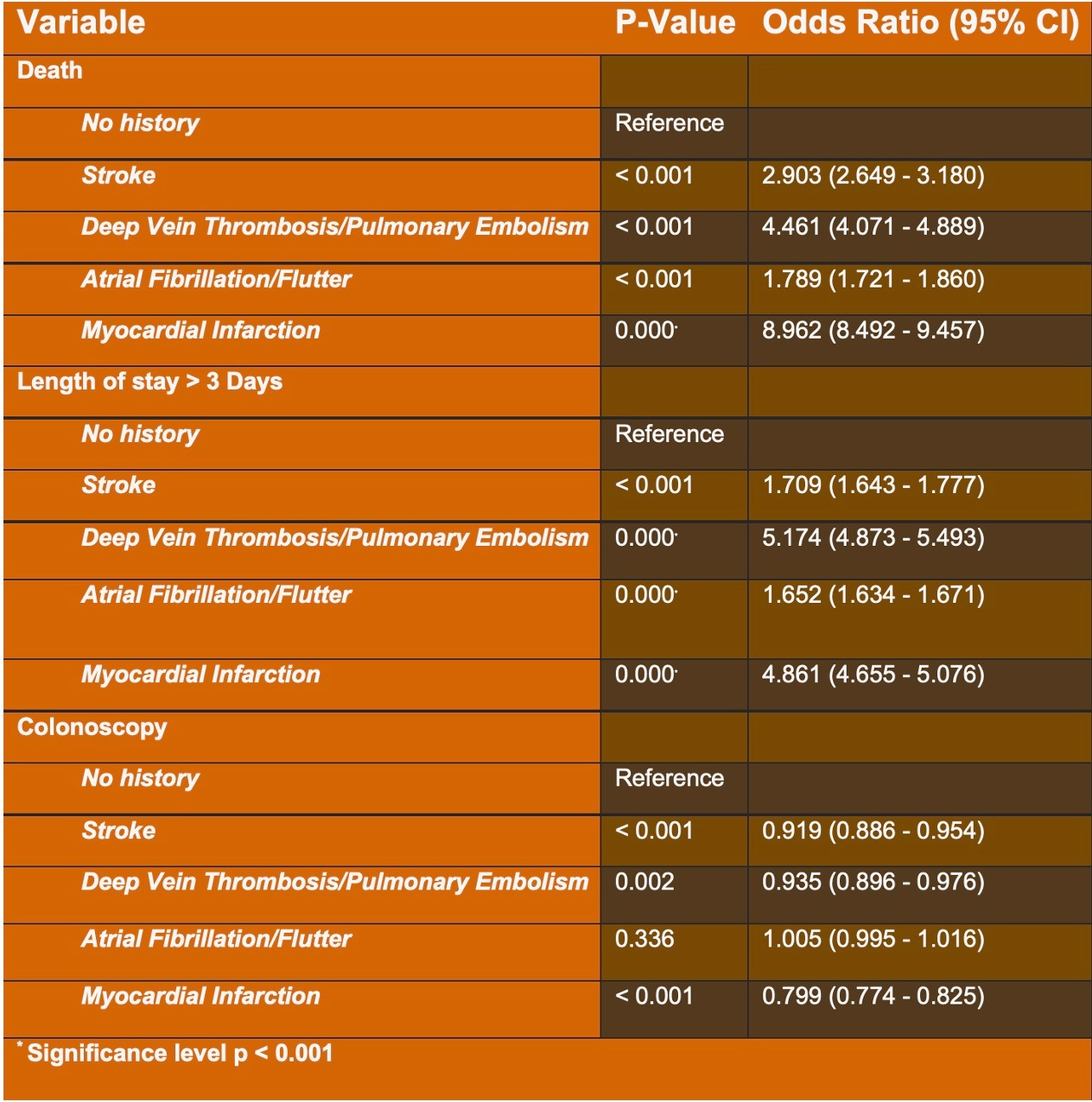
Figure: Table 1. Outcomes in patients with stroke, pulmonary embolism, deep vein thrombosis, atrial fibrillation/flutter, and myocardial infarction who present with diverticular bleed
Disclosures:
Alexander Le indicated no relevant financial relationships.
Anmol Mittal indicated no relevant financial relationships.
Aaron Kahlam indicated no relevant financial relationships.
Sushil Ahlawat indicated no relevant financial relationships.
Alexander Le, MD, Anmol Mittal, MD, Aaron Kahlam, MD, Sushil Ahlawat, MD. E0297 - Outcomes of Patients With History of Stroke, Pulmonary Embolism, Deep Vein Thrombosis, Atrial Fibrillation, and Myocardial Infarction Who Present With a Diverticular Bleed, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
