Back
Poster Session A - Sunday Afternoon
A0311 - Diffuse Intestinal Amyloidosis Complicated by Pancreatic NET, Splenic Vein Thrombosis With Gastrosplenic Shunt Formation and Bleeding Angioectasias Requiring Total Colectomy
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Pranay Reddy, MD, MPH
Jefferson Health Northeast
Philadelphia, PA
Presenting Author(s)
Pranay Reddy, MD, MPH1, Tuba Esfandyari, MD, MSc2, Shruti Khurana, MD2, Rashna Madan, MBBS2
1Jefferson Health Northeast, Philadelphia, PA; 2Kansas University Medical Center, Kansas City, KS
Introduction: Pancreatic Neuroendocrine tumors (pNETs) are endocrine tumors arising from the pancreas and are one of the most common NETs. Splenic vein thrombosis with resulting sinistral hypertension is a rare complication of pNETs causing isolated gastric varices and less commonly portal hypertensive colopathy if portal vein becomes involved. In this case, we present a 78-year-old male with intestinal amyloidosis complicated by pancreatic neuroendocrine tumor (NET), splenic vein occlusion with gastrosplenic shunt formation and gastrointestinal hemorrhage secondary to diffuse colonic angioectasias.
Case Description/Methods: A 78-year-old male with history of ADPKD, CAD, and HTN was initially found to have colonic mass on screening colonoscopy. Biopsies at that time illustrated congo red staining positivity for light chain (AL) amyloidosis. He was maintained on daratumumab in the outpatient setting and remained complication free for nearly two decades. Following a cardiac catheterization with stent placement, patient was started on dual antiplatelet therapy and had resulting hematochezia requiring admission. Colonoscopy showed friable mucosa with ulceration from rectum to cecum as well as ulcerated polypoid lesions. The following year patient was found to have pancreatic tail mass on CT and subsequently underwent EUS with FNA revealing pNET. Clinical course was further complicated by splenic vein thrombosis, large gastrosplenic shunt formation and type II isolated bleeding varices. He ultimately underwent coil embolization with IR and was started on lanreotide injections for pNET. The patient now presented with melenic stools of two days duration. EGD redemonstrated nonbleeding type I isolated gastric varices and colonoscopy revealed numerous actively bleeding colonic angioectasias treated with ablation. Due to persistent hematochezia, CT venogram was performed which demonstrated pneumoperitoneum concerning for perforated viscus. He was seen by colorectal surgery, underwent total colectomy with ileostomy and was eventually discharged to rehab in stable condition.
Discussion: Splenic vein thrombosis is a rare complication of pNETs which can cause isolated gastric varices and is recognized as an important cause of upper GI bleeding. This case highlights a rare complication of pNET whereby a splenic vein occlusion and large gastrospenic shunt eventually involved the portal vein causing true right sided portal hypertension with development of portal hypertensive colopathy characterized by bleeding angioectasias.
Disclosures:
Pranay Reddy, MD, MPH1, Tuba Esfandyari, MD, MSc2, Shruti Khurana, MD2, Rashna Madan, MBBS2. A0311 - Diffuse Intestinal Amyloidosis Complicated by Pancreatic NET, Splenic Vein Thrombosis With Gastrosplenic Shunt Formation and Bleeding Angioectasias Requiring Total Colectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Jefferson Health Northeast, Philadelphia, PA; 2Kansas University Medical Center, Kansas City, KS
Introduction: Pancreatic Neuroendocrine tumors (pNETs) are endocrine tumors arising from the pancreas and are one of the most common NETs. Splenic vein thrombosis with resulting sinistral hypertension is a rare complication of pNETs causing isolated gastric varices and less commonly portal hypertensive colopathy if portal vein becomes involved. In this case, we present a 78-year-old male with intestinal amyloidosis complicated by pancreatic neuroendocrine tumor (NET), splenic vein occlusion with gastrosplenic shunt formation and gastrointestinal hemorrhage secondary to diffuse colonic angioectasias.
Case Description/Methods: A 78-year-old male with history of ADPKD, CAD, and HTN was initially found to have colonic mass on screening colonoscopy. Biopsies at that time illustrated congo red staining positivity for light chain (AL) amyloidosis. He was maintained on daratumumab in the outpatient setting and remained complication free for nearly two decades. Following a cardiac catheterization with stent placement, patient was started on dual antiplatelet therapy and had resulting hematochezia requiring admission. Colonoscopy showed friable mucosa with ulceration from rectum to cecum as well as ulcerated polypoid lesions. The following year patient was found to have pancreatic tail mass on CT and subsequently underwent EUS with FNA revealing pNET. Clinical course was further complicated by splenic vein thrombosis, large gastrosplenic shunt formation and type II isolated bleeding varices. He ultimately underwent coil embolization with IR and was started on lanreotide injections for pNET. The patient now presented with melenic stools of two days duration. EGD redemonstrated nonbleeding type I isolated gastric varices and colonoscopy revealed numerous actively bleeding colonic angioectasias treated with ablation. Due to persistent hematochezia, CT venogram was performed which demonstrated pneumoperitoneum concerning for perforated viscus. He was seen by colorectal surgery, underwent total colectomy with ileostomy and was eventually discharged to rehab in stable condition.
Discussion: Splenic vein thrombosis is a rare complication of pNETs which can cause isolated gastric varices and is recognized as an important cause of upper GI bleeding. This case highlights a rare complication of pNET whereby a splenic vein occlusion and large gastrospenic shunt eventually involved the portal vein causing true right sided portal hypertension with development of portal hypertensive colopathy characterized by bleeding angioectasias.
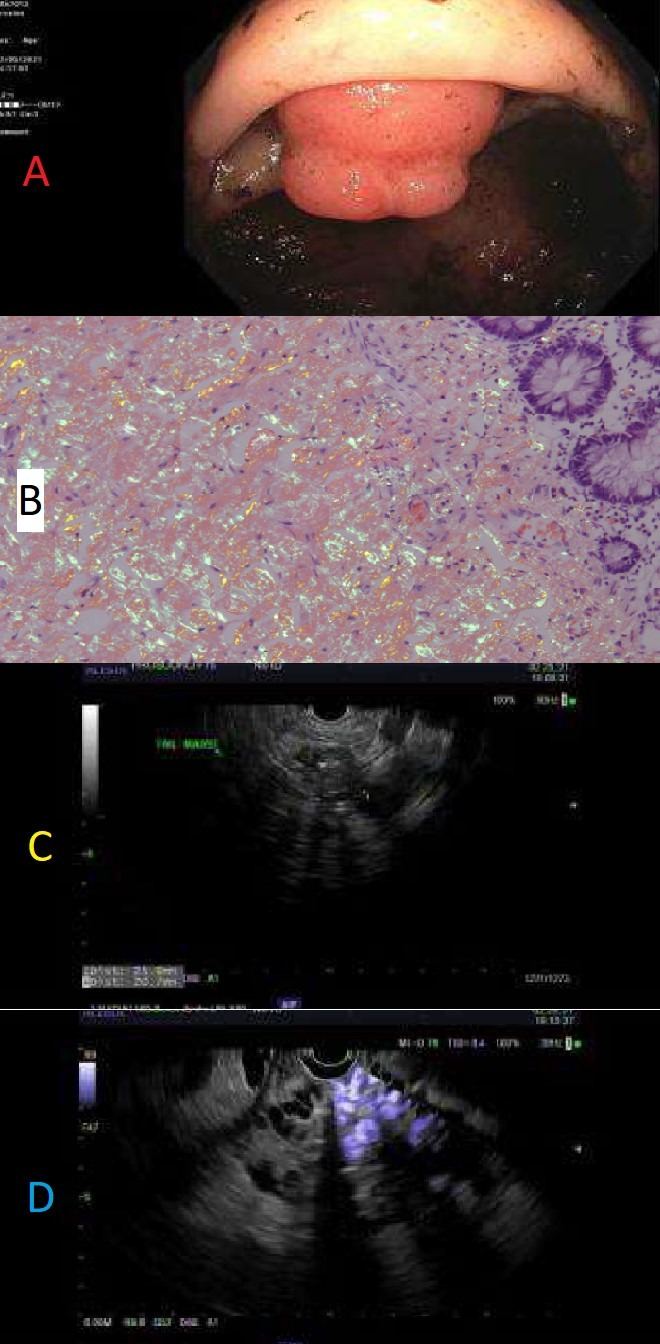
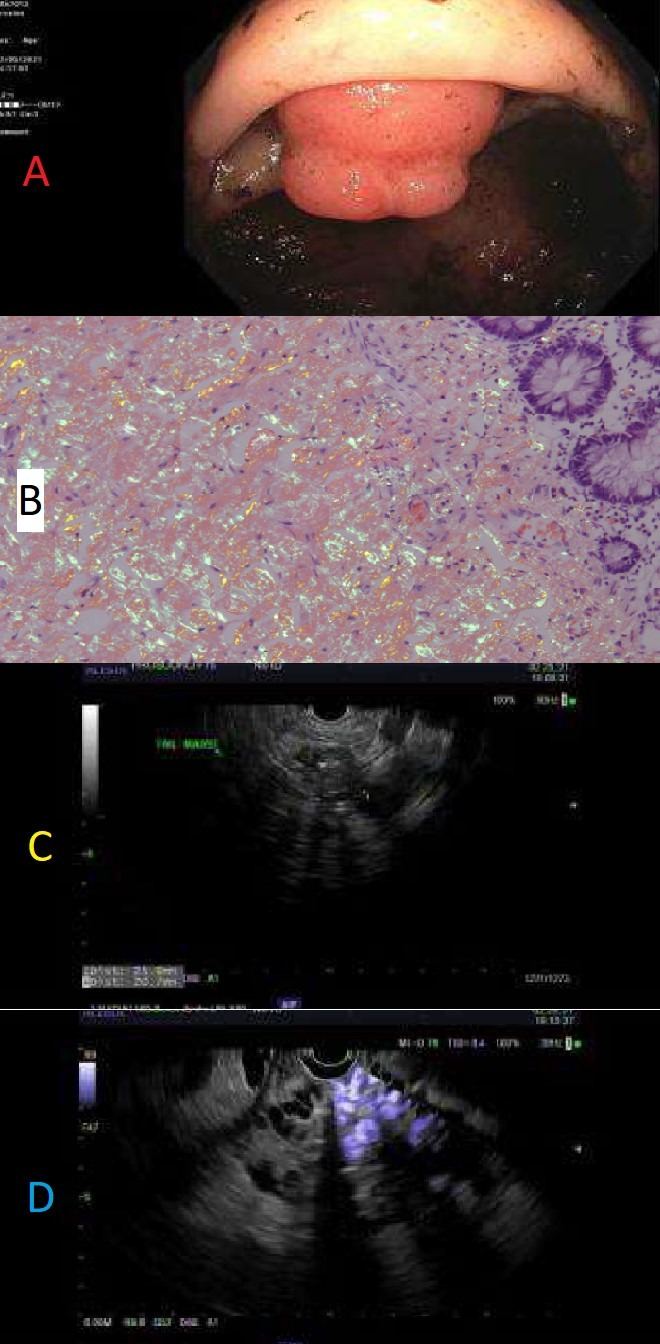
Figure: A) Large amyloidoma extruding from terminal ileum
B) Cecum histopathology: Positive congo red stain with apple-green birefringence under polarized light
C) EUS showing 25mm x 21mm hypoechoic lesion in pancreatic tail with few calcifications
D) Hypoechoic pancreatic tail lesion with intervening fundal varices preventing biopsy
B) Cecum histopathology: Positive congo red stain with apple-green birefringence under polarized light
C) EUS showing 25mm x 21mm hypoechoic lesion in pancreatic tail with few calcifications
D) Hypoechoic pancreatic tail lesion with intervening fundal varices preventing biopsy
Disclosures:
Pranay Reddy indicated no relevant financial relationships.
Tuba Esfandyari indicated no relevant financial relationships.
Shruti Khurana indicated no relevant financial relationships.
Rashna Madan indicated no relevant financial relationships.
Pranay Reddy, MD, MPH1, Tuba Esfandyari, MD, MSc2, Shruti Khurana, MD2, Rashna Madan, MBBS2. A0311 - Diffuse Intestinal Amyloidosis Complicated by Pancreatic NET, Splenic Vein Thrombosis With Gastrosplenic Shunt Formation and Bleeding Angioectasias Requiring Total Colectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
