Back
Poster Session C - Monday Afternoon
C0326 - Ischemic Gastropathy vs. Severe H. pylori Gastritis in a Patient With Extensive Vascular Disease
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Nicole B. Salvi, BA
NYU Grossman School of Medicine
New York, NY
Presenting Author(s)
Nicole B. Salvi, BA1, Joshua D. Kirschenbaum, BS1, Barathi Sivasailam, MD2, Renee L. Williams, MD, MHPE, FACG1
1NYU Grossman School of Medicine, New York, NY; 2New York University Langone Medical Center, New York, NY
Introduction: Approximately half of gastric ulcers are associated with H. pylori. Conversely, gastric ulceration secondary to ischemia is rare due to the stomach’s abundant vascular supply from all three branches of the celiac artery. Here we present a case of a patient with upper gastrointestinal bleeding and concern for gastric ischemia who was diagnosed with H. pylori associated gastritis.
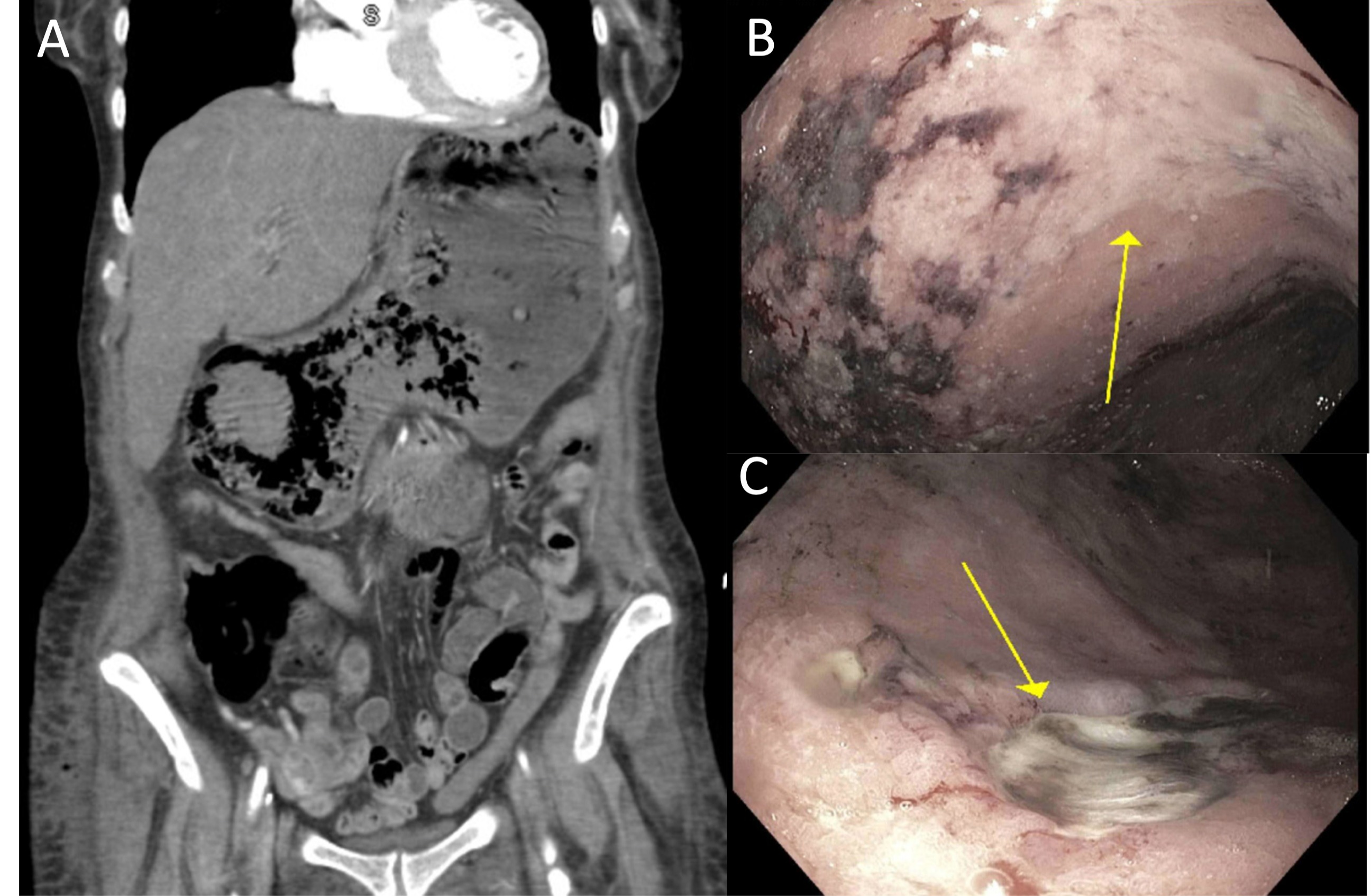
Case Description/Methods: A 70-year-old female with severe peripheral artery disease, abdominal aortic aneurysm status post endovascular repair, hypertension, HIV, chronic kidney disease and B-cell lymphoma was admitted for pathologic right hip fracture and underwent open reduction and internal fixation. The procedure was complicated by lactic acidosis, an elevated troponin, and transaminitis in the setting of intraoperative hypotension. Six days later the patient had coffee ground emesis and melena with a lactate of 9.8 mmol/L and a hemoglobin of 6.4 g/dL, from 8.9 g/dL one day prior. 2 units of packed red blood cells were administered, anticoagulation was stopped, and a proton pump inhibitor was given. CT angiography of the abdomen and pelvis demonstrated splenic infarction, marked attenuation of multiple mesenteric vessels including the celiac artery, concern for ischemia of the stomach and cecum, and significant distention of the stomach (Figure, A). Upper endoscopy demonstrated severe gastric mucosal pallor and decreased vascular pattern, diffuse linear erosions throughout the gastric fundus and body, and multiple large superficial ulcerations without active bleeding (Figure, B and C). Given the appearance of the mucosa and overall clinical picture, there was concern for ischemic gastritis and biopsies were taken. Histology later revealed erosive gastritis, regenerative change and H. pylori without evidence of microthrombi or changes consistent with ischemia and the patient was started on quadruple therapy for H. pylori gastritis. She had one further episode of melena and received an additional blood transfusion before she was discharged one week later.
Discussion: Our patient had extensive vascular disease and systemic hypotension with endoscopic findings highly suspicious for ischemic injury but with biopsies consistent with severe H. pylori gastritis. Although ischemic gastropathy should be considered in cases of an upper GI bleed in patients with vascular risk factors, careful histopathologic review is important for accurate diagnosis, and severe presentations of more routine diagnoses should also be considered.
Disclosures:
Nicole B. Salvi, BA1, Joshua D. Kirschenbaum, BS1, Barathi Sivasailam, MD2, Renee L. Williams, MD, MHPE, FACG1. C0326 - Ischemic Gastropathy vs. Severe H. pylori Gastritis in a Patient With Extensive Vascular Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1NYU Grossman School of Medicine, New York, NY; 2New York University Langone Medical Center, New York, NY
Introduction: Approximately half of gastric ulcers are associated with H. pylori. Conversely, gastric ulceration secondary to ischemia is rare due to the stomach’s abundant vascular supply from all three branches of the celiac artery. Here we present a case of a patient with upper gastrointestinal bleeding and concern for gastric ischemia who was diagnosed with H. pylori associated gastritis.
Case Description/Methods: A 70-year-old female with severe peripheral artery disease, abdominal aortic aneurysm status post endovascular repair, hypertension, HIV, chronic kidney disease and B-cell lymphoma was admitted for pathologic right hip fracture and underwent open reduction and internal fixation. The procedure was complicated by lactic acidosis, an elevated troponin, and transaminitis in the setting of intraoperative hypotension. Six days later the patient had coffee ground emesis and melena with a lactate of 9.8 mmol/L and a hemoglobin of 6.4 g/dL, from 8.9 g/dL one day prior. 2 units of packed red blood cells were administered, anticoagulation was stopped, and a proton pump inhibitor was given. CT angiography of the abdomen and pelvis demonstrated splenic infarction, marked attenuation of multiple mesenteric vessels including the celiac artery, concern for ischemia of the stomach and cecum, and significant distention of the stomach (Figure, A). Upper endoscopy demonstrated severe gastric mucosal pallor and decreased vascular pattern, diffuse linear erosions throughout the gastric fundus and body, and multiple large superficial ulcerations without active bleeding (Figure, B and C). Given the appearance of the mucosa and overall clinical picture, there was concern for ischemic gastritis and biopsies were taken. Histology later revealed erosive gastritis, regenerative change and H. pylori without evidence of microthrombi or changes consistent with ischemia and the patient was started on quadruple therapy for H. pylori gastritis. She had one further episode of melena and received an additional blood transfusion before she was discharged one week later.
Discussion: Our patient had extensive vascular disease and systemic hypotension with endoscopic findings highly suspicious for ischemic injury but with biopsies consistent with severe H. pylori gastritis. Although ischemic gastropathy should be considered in cases of an upper GI bleed in patients with vascular risk factors, careful histopathologic review is important for accurate diagnosis, and severe presentations of more routine diagnoses should also be considered.
Figure: Figure. A) CT angiography of the abdomen and pelvis demonstrating significant gastric distention. B) Esophagogastroduodenoscopy demonstrating mucosal pallor and C) large ulcerations within the gastric body
Disclosures:
Nicole Salvi indicated no relevant financial relationships.
Joshua Kirschenbaum indicated no relevant financial relationships.
Barathi Sivasailam indicated no relevant financial relationships.
Renee Williams: Boston Scientific – Stock-publicly held company(excluding mutual/index funds).
Nicole B. Salvi, BA1, Joshua D. Kirschenbaum, BS1, Barathi Sivasailam, MD2, Renee L. Williams, MD, MHPE, FACG1. C0326 - Ischemic Gastropathy vs. Severe H. pylori Gastritis in a Patient With Extensive Vascular Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
