Back
Poster Session C - Monday Afternoon
C0213 - Safety and Efficacy of Esoflip for Achalasia: A Systematic Review and Meta-Analysis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Christopher Picking, MD
Creighton University
Omaha, NE
Presenting Author(s)
Syed Mohsin Saghir, MD1, Anand Kumar, MD2, Christopher Picking, MD3, Haris Chaudhry, MD3, Yazan Addasi, MD3, Yassin Naga, MD4, Zahra Dossaji, DO4, Banreet S. Dhindsa, MD5, Rajani Rangray, MBBS1, Saurabh Chandan, MD6, Douglas G. Adler, MD, FACG7
1CHI Creighton University Medical Center, Omaha, NE; 2Northwell Health - Lenox Hill Hospital, New York, NY; 3Creighton University, Omaha, NE; 4Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 5University of Nebraska Medical Center, Omaha, NE; 6CHI Health Creighton School of Medicine, Omaha, NE; 7Centura Health-Porter Adventist Hospital, Salt Lake City, UT
Introduction:
Achalasia is a rare esophageal motility disorder due to degeneration of ganglion cells in the myenteric plexus leading to failure of relaxation of the distal esophageal sphincter. Current treatment options include pneumatic dilation, laparoscopic heller myotomy, and peroral endoscopic myotomy. Esophageal functional luminal imaging probe (EsoFLIP, Medtronic, Minneapolis, MN) is an emerging therapeutic modality for management of achalasia, however, data is limited. This device utilizes high resolution impedance planimetry that provides a real-time graphical depiction of the esophageal lumen without the need for fluoroscopy followed by hydraulic dilation. This is the first systematic review and meta-analysis to evaluate safety and efficacy of EsoFLIP for the management of achalasia.
Methods:
Several electronic databases and conference proceedings such as PubMed, Google Scholar, Web of Science, EMBASE, CINAHL (from inception through May 2021) were reviewed to identify studies reporting the use of EsoFLIP for achalasia. The primary outcomes assessed were technical and clinical success of EsoFLIP in management for achalasia. Technical success was defined as the ability to successfully dilate the esophagus up to 30 mm with the EsoFLIP balloon. Clinical success was defined as the ability to achieve a post-dilation Eckardt score (ES) < 4. The secondary outcomes assessed were total and individual adverse event (AE) rates secondary to the procedure and recurrence of dysphagia post procedure.
Results:
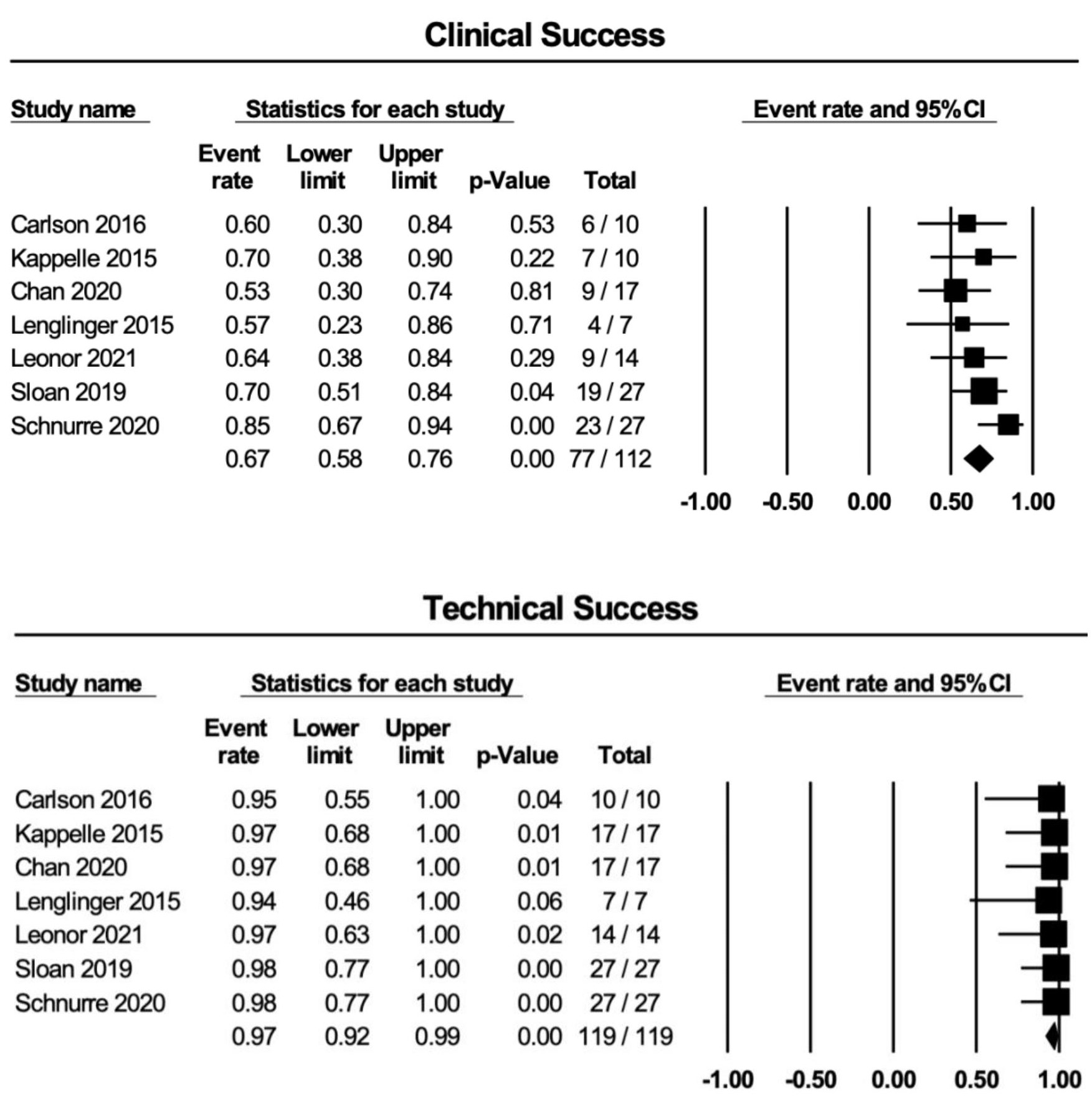
7 studies reporting on 112 patients with a median age of 49.5 years were included in our final analysis. About half the patients were treatment naive. Mean pre-dilation ES was 7. Technical and clinical success rate was 97% (95% CI 92%,99%; I2=0) and 67% (95% CI 58%, 76%; I2=0), respectively. AE rate was 6% (95% CI 2.6%, 13%; I2=0) with perforation being the most common AE. Recurrence rate was 13% (95% CI 6%, 26%; I2=2). Post-dilation reflux was reported in 4 studies in 22 patients. Mean follow up was 2.1 months. Meta-analysis was conducted with Der Simonian and Laird random effects model using CMA software version 3.
Discussion:
Our study demonstrated high technical success but lower clinical success as compared to other modalities. However, EsoFLIP has the advantage of having a diagnositic procedure (EndoFLIP) performed at the same time. While further studies are needed to validate our findings, this technology is a promising addition to the armamentarium for management of achalasia.
Disclosures:
Syed Mohsin Saghir, MD1, Anand Kumar, MD2, Christopher Picking, MD3, Haris Chaudhry, MD3, Yazan Addasi, MD3, Yassin Naga, MD4, Zahra Dossaji, DO4, Banreet S. Dhindsa, MD5, Rajani Rangray, MBBS1, Saurabh Chandan, MD6, Douglas G. Adler, MD, FACG7. C0213 - Safety and Efficacy of Esoflip for Achalasia: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1CHI Creighton University Medical Center, Omaha, NE; 2Northwell Health - Lenox Hill Hospital, New York, NY; 3Creighton University, Omaha, NE; 4Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 5University of Nebraska Medical Center, Omaha, NE; 6CHI Health Creighton School of Medicine, Omaha, NE; 7Centura Health-Porter Adventist Hospital, Salt Lake City, UT
Introduction:
Achalasia is a rare esophageal motility disorder due to degeneration of ganglion cells in the myenteric plexus leading to failure of relaxation of the distal esophageal sphincter. Current treatment options include pneumatic dilation, laparoscopic heller myotomy, and peroral endoscopic myotomy. Esophageal functional luminal imaging probe (EsoFLIP, Medtronic, Minneapolis, MN) is an emerging therapeutic modality for management of achalasia, however, data is limited. This device utilizes high resolution impedance planimetry that provides a real-time graphical depiction of the esophageal lumen without the need for fluoroscopy followed by hydraulic dilation. This is the first systematic review and meta-analysis to evaluate safety and efficacy of EsoFLIP for the management of achalasia.
Methods:
Several electronic databases and conference proceedings such as PubMed, Google Scholar, Web of Science, EMBASE, CINAHL (from inception through May 2021) were reviewed to identify studies reporting the use of EsoFLIP for achalasia. The primary outcomes assessed were technical and clinical success of EsoFLIP in management for achalasia. Technical success was defined as the ability to successfully dilate the esophagus up to 30 mm with the EsoFLIP balloon. Clinical success was defined as the ability to achieve a post-dilation Eckardt score (ES) < 4. The secondary outcomes assessed were total and individual adverse event (AE) rates secondary to the procedure and recurrence of dysphagia post procedure.
Results:
7 studies reporting on 112 patients with a median age of 49.5 years were included in our final analysis. About half the patients were treatment naive. Mean pre-dilation ES was 7. Technical and clinical success rate was 97% (95% CI 92%,99%; I2=0) and 67% (95% CI 58%, 76%; I2=0), respectively. AE rate was 6% (95% CI 2.6%, 13%; I2=0) with perforation being the most common AE. Recurrence rate was 13% (95% CI 6%, 26%; I2=2). Post-dilation reflux was reported in 4 studies in 22 patients. Mean follow up was 2.1 months. Meta-analysis was conducted with Der Simonian and Laird random effects model using CMA software version 3.
Discussion:
Our study demonstrated high technical success but lower clinical success as compared to other modalities. However, EsoFLIP has the advantage of having a diagnositic procedure (EndoFLIP) performed at the same time. While further studies are needed to validate our findings, this technology is a promising addition to the armamentarium for management of achalasia.
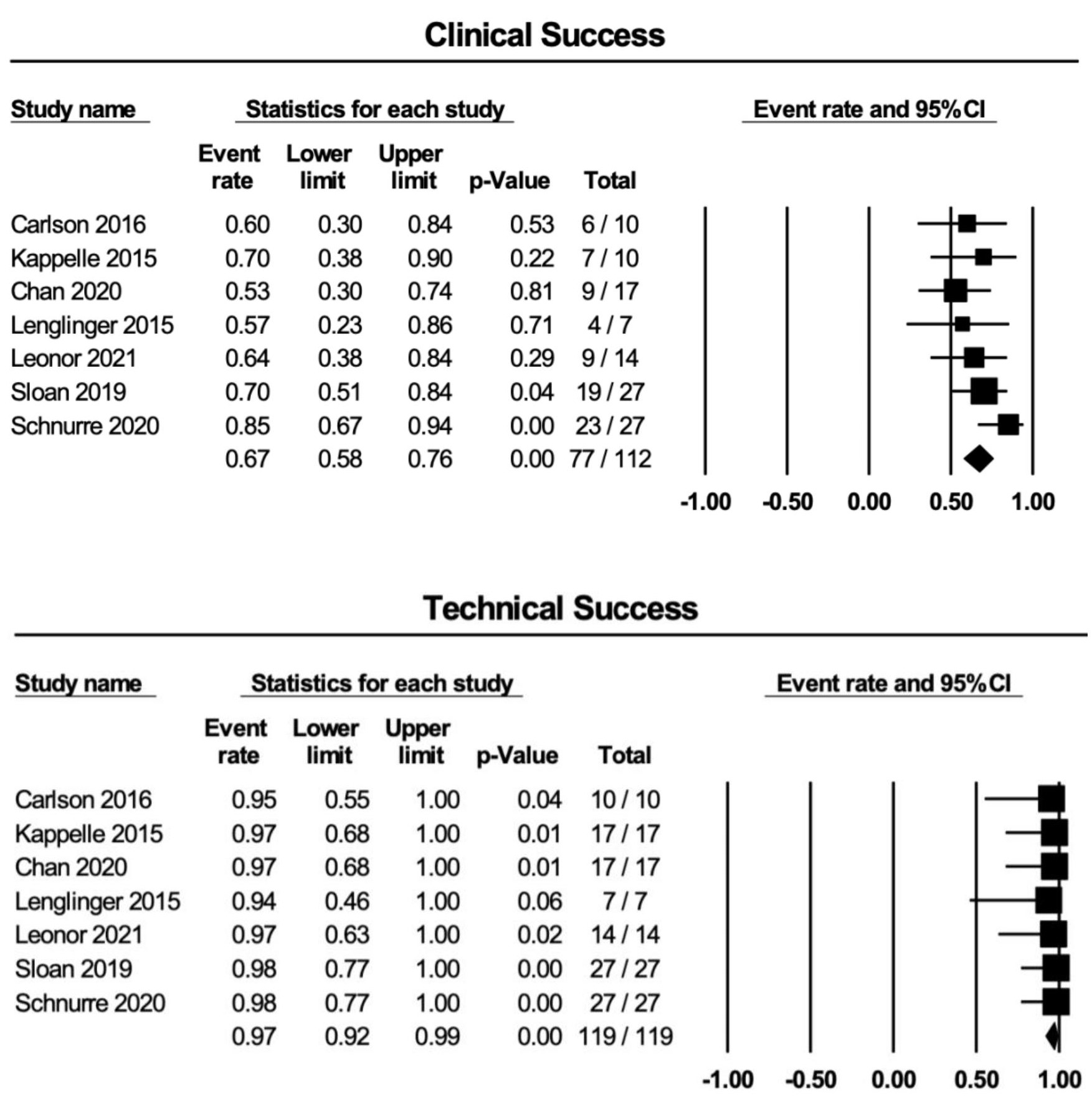
Figure: Top: Forest plots displaying the clinical success rates for ESOFLIP
Bottom: Forest plots displaying the technical success rates for ESOFLIP
Bottom: Forest plots displaying the technical success rates for ESOFLIP
Disclosures:
Syed Mohsin Saghir indicated no relevant financial relationships.
Anand Kumar indicated no relevant financial relationships.
Christopher Picking indicated no relevant financial relationships.
Haris Chaudhry indicated no relevant financial relationships.
Yazan Addasi indicated no relevant financial relationships.
Yassin Naga indicated no relevant financial relationships.
Zahra Dossaji indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Rajani Rangray indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Douglas Adler: Boston Scientific – Consultant.
Syed Mohsin Saghir, MD1, Anand Kumar, MD2, Christopher Picking, MD3, Haris Chaudhry, MD3, Yazan Addasi, MD3, Yassin Naga, MD4, Zahra Dossaji, DO4, Banreet S. Dhindsa, MD5, Rajani Rangray, MBBS1, Saurabh Chandan, MD6, Douglas G. Adler, MD, FACG7. C0213 - Safety and Efficacy of Esoflip for Achalasia: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
