Back
Poster Session C - Monday Afternoon
C0237 - Uphill and Downhill Esophageal Varices Secondary to Pulmonary Hypertension
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

William Dungan, MD
Medical University of South Carolina
Charleston, SC
Presenting Author(s)
William Dungan, MD, Jonathan Reichstein, MD, Puja Elias, MD
Medical University of South Carolina, Charleston, SC
Introduction: Proximal downhill esophageal varices (EV) are rare, accounting for 0.5% of EV. They develop from superior vena cava (SVC) obstruction and retrograde blood flow through upper and middle peri-esophageal collaterals. Historically, downhill EV are associated with malignancy, thrombosis, or iatrogenic causes. Few cases of benign obstruction, as in pulmonary hypertension (PH) with tricuspid regurgitation (TR), have been reported.
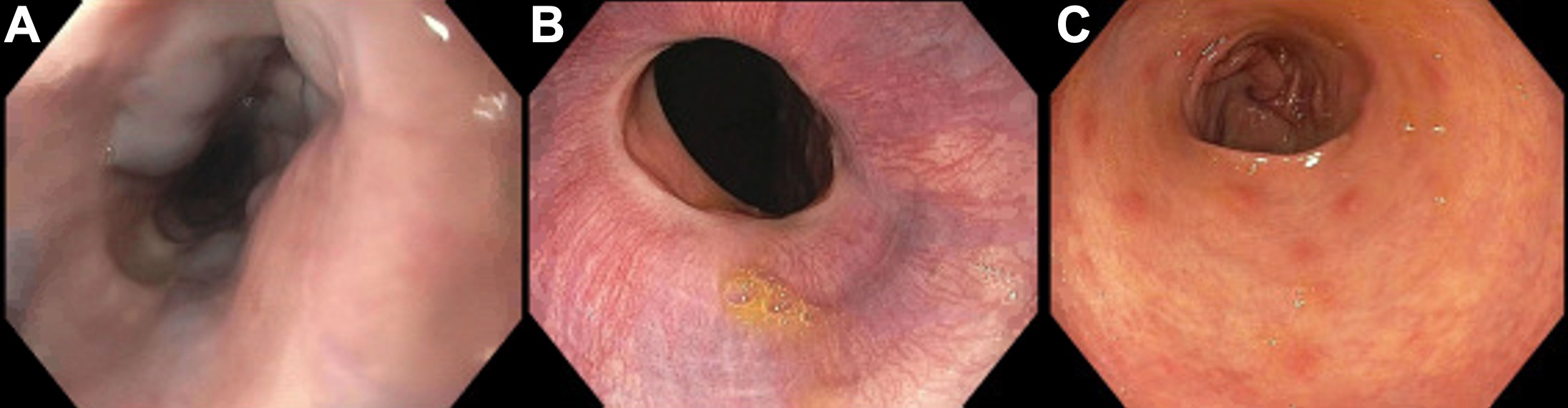
Case Description/Methods: A 67-year-old female with PH and atrial flutter presented with 3-weeks of melena. She denied vomiting, hematochezia, or history of malignancy. Her warfarin dose was stable, and she reported decreased vegetable intake for months. She endorsed chronic alcohol use but no NSAID or tobacco use. She was hemodynamically stable on admission. Physical exam revealed a LLSB holosystolic murmur. Notable labs included hgb 7.5g/dL, iron deficiency and INR 11.3. She received IV vitamin K, IV PPI BID and warfarin was held. EGD revealed large proximal EV, grade 1 distal EV and nodular gastric antral vascular ectasia, but no bleeding. CT chest and abdomen ruled out malignancy or SVC obstruction but revealed cirrhosis and portal hypertension. TTE showed severe TR and PH. She had no further episodes of melena. She was discharged with a MELD-Na of 24 and plans for liver biopsy and right heart catheterization for further workup.
Discussion: Of the few cases of downhill EV due to PH, both TR and PH were present, allowing high filling pressure and SVC congestion. Hemorrhage is infrequent, accounting for 0.1% of EV bleeds, likely from low gastric acid exposure, submucosal location, and lack of coagulopathy in cirrhosis. Studies found higher rates of bleeding in benign obstruction with only 14% related to malignancy. Anticoagulant and antiplatelet agents increase risk. Treatment focuses on correcting the underlying cause. Endoscopic band ligation or sclerotherapy are reserved for emergent bleeding due to risk of esophageal perforation, stricture, or infarction. Studies of repeat EGD 5 years post diagnosis revealed stable size providing evidence against routine surveillance. Our patient’s melena was likely from gastric mucosal oozing due to supratherapeutic INR and vitamin K deficiency. In summary, downhill EV are often incidental and associated with severe comorbidities. Further workup is crucial for ruling out malignancy and preventing hemorrhage. Additional cases are needed to evaluate the safety and efficacy of endoscopic intervention and utility of surveillance screening.
Disclosures:
William Dungan, MD, Jonathan Reichstein, MD, Puja Elias, MD. C0237 - Uphill and Downhill Esophageal Varices Secondary to Pulmonary Hypertension, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Medical University of South Carolina, Charleston, SC
Introduction: Proximal downhill esophageal varices (EV) are rare, accounting for 0.5% of EV. They develop from superior vena cava (SVC) obstruction and retrograde blood flow through upper and middle peri-esophageal collaterals. Historically, downhill EV are associated with malignancy, thrombosis, or iatrogenic causes. Few cases of benign obstruction, as in pulmonary hypertension (PH) with tricuspid regurgitation (TR), have been reported.
Case Description/Methods: A 67-year-old female with PH and atrial flutter presented with 3-weeks of melena. She denied vomiting, hematochezia, or history of malignancy. Her warfarin dose was stable, and she reported decreased vegetable intake for months. She endorsed chronic alcohol use but no NSAID or tobacco use. She was hemodynamically stable on admission. Physical exam revealed a LLSB holosystolic murmur. Notable labs included hgb 7.5g/dL, iron deficiency and INR 11.3. She received IV vitamin K, IV PPI BID and warfarin was held. EGD revealed large proximal EV, grade 1 distal EV and nodular gastric antral vascular ectasia, but no bleeding. CT chest and abdomen ruled out malignancy or SVC obstruction but revealed cirrhosis and portal hypertension. TTE showed severe TR and PH. She had no further episodes of melena. She was discharged with a MELD-Na of 24 and plans for liver biopsy and right heart catheterization for further workup.
Discussion: Of the few cases of downhill EV due to PH, both TR and PH were present, allowing high filling pressure and SVC congestion. Hemorrhage is infrequent, accounting for 0.1% of EV bleeds, likely from low gastric acid exposure, submucosal location, and lack of coagulopathy in cirrhosis. Studies found higher rates of bleeding in benign obstruction with only 14% related to malignancy. Anticoagulant and antiplatelet agents increase risk. Treatment focuses on correcting the underlying cause. Endoscopic band ligation or sclerotherapy are reserved for emergent bleeding due to risk of esophageal perforation, stricture, or infarction. Studies of repeat EGD 5 years post diagnosis revealed stable size providing evidence against routine surveillance. Our patient’s melena was likely from gastric mucosal oozing due to supratherapeutic INR and vitamin K deficiency. In summary, downhill EV are often incidental and associated with severe comorbidities. Further workup is crucial for ruling out malignancy and preventing hemorrhage. Additional cases are needed to evaluate the safety and efficacy of endoscopic intervention and utility of surveillance screening.
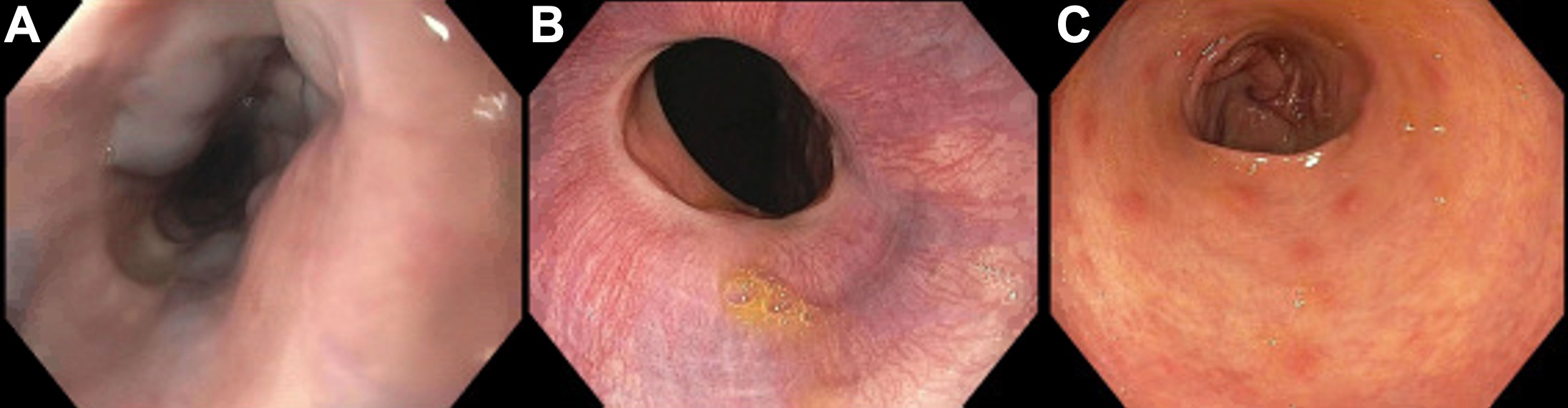
Figure: Figure 1.: EGD revealing both proximal “downhill” and distal "uphill" esophageal varices (EV) and nodular gastric antral vascular ectasia (GAVE). (A) Prominent proximal EV with no stigmata of recent bleeding. (B) Non-bleeding, grade 1 distal EV. (C) Nodular GAVE located in the antrum of the stomach.
Disclosures:
William Dungan indicated no relevant financial relationships.
Jonathan Reichstein indicated no relevant financial relationships.
Puja Elias indicated no relevant financial relationships.
William Dungan, MD, Jonathan Reichstein, MD, Puja Elias, MD. C0237 - Uphill and Downhill Esophageal Varices Secondary to Pulmonary Hypertension, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
