Back
Poster Session E - Tuesday Afternoon
E0204 - Variations in Barrett’s Esophagus Screening, Diagnosis, and Management Among Experts: Myth or Reality?
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Allon Kahn, MD
Mayo Clinic
Scottsdale, AZ
Presenting Author(s)
Allon Kahn, MD1, Prasad G. Iyer, MD, FACG2, John O. Clarke, MD3, Afrin N. Kamal, MD, MS3
1Mayo Clinic, Scottsdale, AZ; 2Mayo Clinic, Rochester, MN; 3Stanford University, Redwood City, CA
Introduction: Barrett’s esophagus (BE) is the only known precursor to esophageal adenocarcinoma (EAC). Although clinical practice guidelines provide an evidence-based framework for BE diagnosis and management, lack of evidence in some areas may preclude definitive recommendations and controversies remain. BE experts are best positioned to provide guidance in these areas, but uniformity of their perspectives has not been assessed. We aimed to assess practice patterns specific to BE screening, diagnosis and management among recognized BE expert gastroenterologists.
Methods: We surveyed BE expert gastroenterologists (N= 38) throughout the United States. The investigator-developed online survey assessed expert beliefs and practice patterns specific to screening, diagnosis, and management of BE. We hypothesized practice patterns would vary, particularly in the category of management.
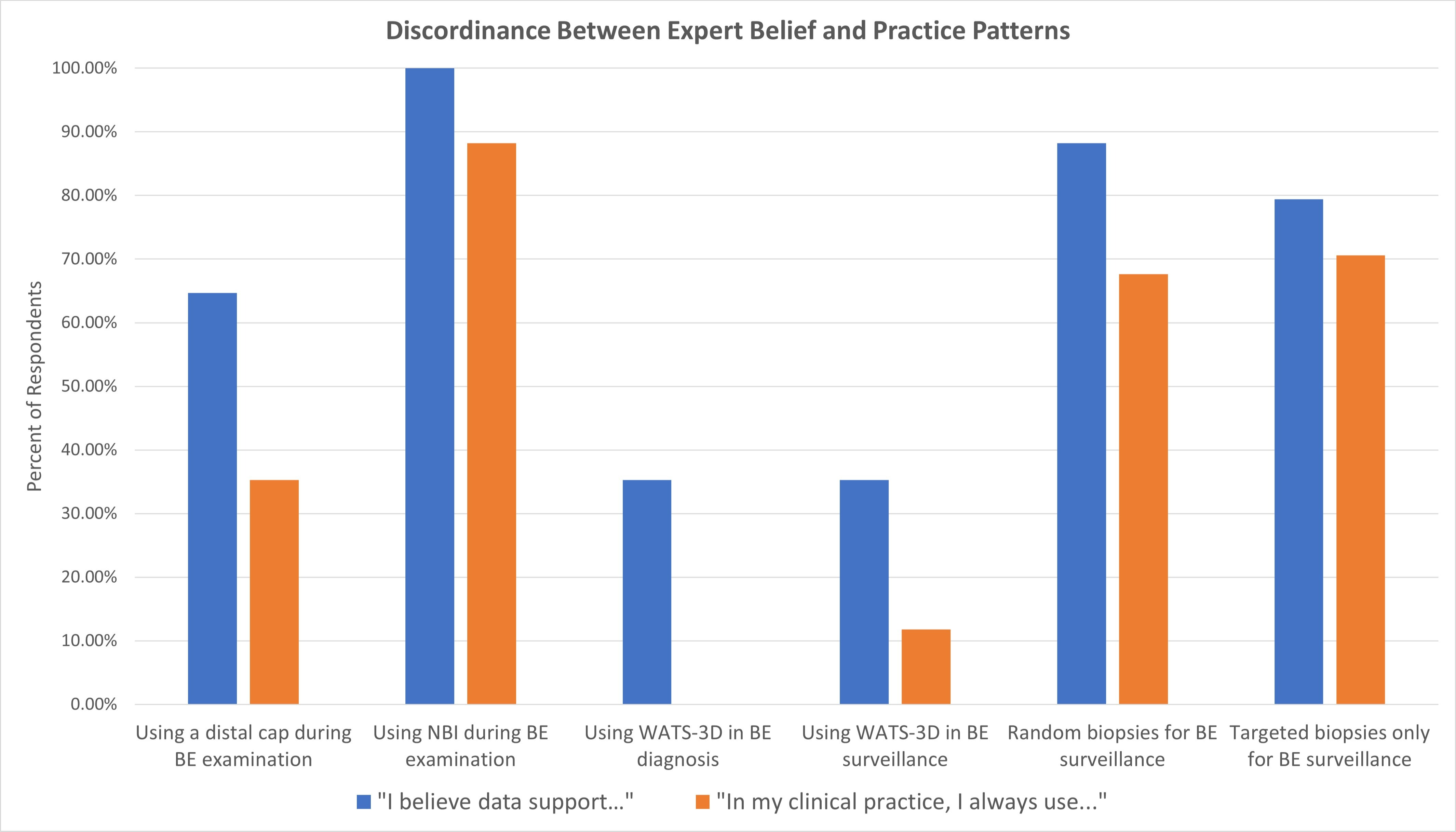
Results: Thirty-four experts responded to the survey (89%), of whom a majority were male (85%), focused their career on Barrett’s esophagus (53%), and practiced in an academic tertiary hospital (82%). Only 19 (55.9%) were confident when BE was diagnosed in a community practice. Discordance between beliefs and clinical practice was common (Figure 1). Despite guideline recommendations to avoid sampling an irregular z-line or ablating non-dysplastic BE (NDBE), only 7 (20.6%) and 16 (47%) adhered strictly to these principles, respectively. All experts agreed that BE indefinite for dysplasia did not merit endoscopic therapy and should prompt repeat EGD after medical GERD optimization. Twenty-nine (85.3%) experts often or always recommended ablation for low-grade dysplasia (LGD). The use of wide-area transepithelial sampling (WATS-3D) was variable, with 22 (64.7%) never utilizing it and 7 (20.6%) saying they used it in most cases, regardless of BE length. Cryotherapy was the most utilized (67.6%) second-line ablative modality, followed by endoscopic resection (17.7%). Surveillance and management of recurrence after complete eradication of intestinal metaplasia (CEIM) was highly variable.
Discussion: Despite available clinical practice guidelines, BE experts exhibit substantial variability in practice, particularly with respect to the use of WATS-3D, NDBE ablation, and post-CEIM management. These results shed light on continued controversies in BE management and emphasize the need for further research to better define management in these areas.
Disclosures:
Allon Kahn, MD1, Prasad G. Iyer, MD, FACG2, John O. Clarke, MD3, Afrin N. Kamal, MD, MS3. E0204 - Variations in Barrett’s Esophagus Screening, Diagnosis, and Management Among Experts: Myth or Reality?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mayo Clinic, Scottsdale, AZ; 2Mayo Clinic, Rochester, MN; 3Stanford University, Redwood City, CA
Introduction: Barrett’s esophagus (BE) is the only known precursor to esophageal adenocarcinoma (EAC). Although clinical practice guidelines provide an evidence-based framework for BE diagnosis and management, lack of evidence in some areas may preclude definitive recommendations and controversies remain. BE experts are best positioned to provide guidance in these areas, but uniformity of their perspectives has not been assessed. We aimed to assess practice patterns specific to BE screening, diagnosis and management among recognized BE expert gastroenterologists.
Methods: We surveyed BE expert gastroenterologists (N= 38) throughout the United States. The investigator-developed online survey assessed expert beliefs and practice patterns specific to screening, diagnosis, and management of BE. We hypothesized practice patterns would vary, particularly in the category of management.
Results: Thirty-four experts responded to the survey (89%), of whom a majority were male (85%), focused their career on Barrett’s esophagus (53%), and practiced in an academic tertiary hospital (82%). Only 19 (55.9%) were confident when BE was diagnosed in a community practice. Discordance between beliefs and clinical practice was common (Figure 1). Despite guideline recommendations to avoid sampling an irregular z-line or ablating non-dysplastic BE (NDBE), only 7 (20.6%) and 16 (47%) adhered strictly to these principles, respectively. All experts agreed that BE indefinite for dysplasia did not merit endoscopic therapy and should prompt repeat EGD after medical GERD optimization. Twenty-nine (85.3%) experts often or always recommended ablation for low-grade dysplasia (LGD). The use of wide-area transepithelial sampling (WATS-3D) was variable, with 22 (64.7%) never utilizing it and 7 (20.6%) saying they used it in most cases, regardless of BE length. Cryotherapy was the most utilized (67.6%) second-line ablative modality, followed by endoscopic resection (17.7%). Surveillance and management of recurrence after complete eradication of intestinal metaplasia (CEIM) was highly variable.
Discussion: Despite available clinical practice guidelines, BE experts exhibit substantial variability in practice, particularly with respect to the use of WATS-3D, NDBE ablation, and post-CEIM management. These results shed light on continued controversies in BE management and emphasize the need for further research to better define management in these areas.
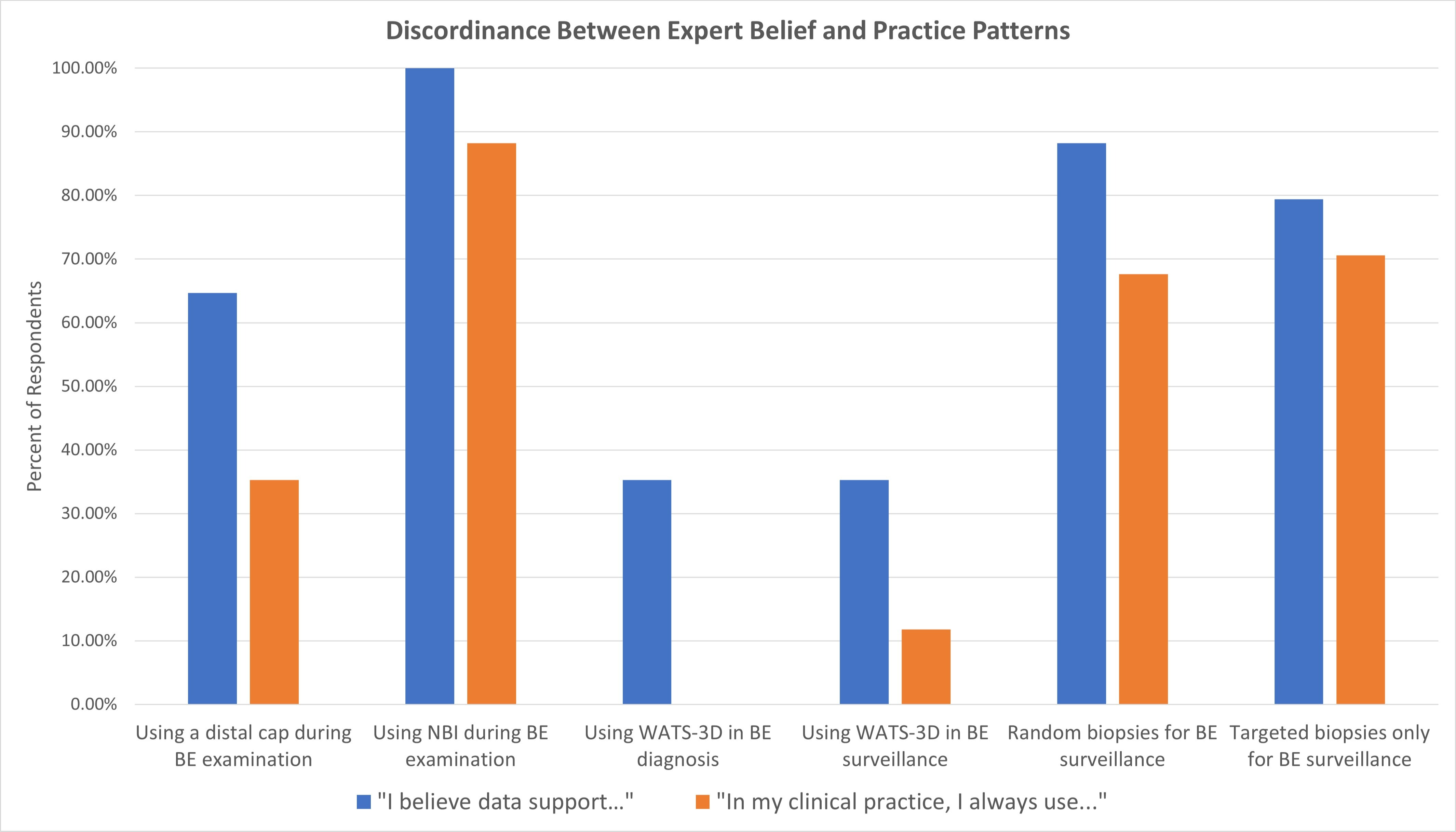
Figure: Figure 1
Disclosures:
Allon Kahn: MiMedx – Consultant.
Prasad Iyer: CDX Medical – Consultant, Grant/Research Support. Cernostics – Consultant, Grant/Research Support. Exact Sciences – Consultant, Grant/Research Support, Intellectual Property/Patents. Medtronic – Consultant. Pentax Medical – Consultant, Grant/Research Support.
John Clarke: Alnylam – Advisory Committee/Board Member. Castle Biosciences – Advisory Committee/Board Member. Isothrive – Advisory Committee/Board Member. Medtronic – Advisory Committee/Board Member. Regeneron – Advisory Committee/Board Member. Sanofi – Advisory Committee/Board Member.
Afrin Kamal indicated no relevant financial relationships.
Allon Kahn, MD1, Prasad G. Iyer, MD, FACG2, John O. Clarke, MD3, Afrin N. Kamal, MD, MS3. E0204 - Variations in Barrett’s Esophagus Screening, Diagnosis, and Management Among Experts: Myth or Reality?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
