Back
Poster Session E - Tuesday Afternoon
E0244 - When Chronic Medical Conditions Mask Acute Symptoms: A Case of Esophageal Perforation With Neck Pain
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Jeremy Polman, DO, MS, MBA
Baton Rouge General Medical Center
Baton Rouge, LA
Presenting Author(s)
Jeremy Polman, DO, MS, MBA1, Rameela Mahat, MD2, Jobin Philipose, MD3
1Baton Rouge General Medical Center, Baton Rouge, LA; 2Baton Rouge General Internal Medicine Residency Program, Baton Rouge, LA; 3Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Esophageal perforation is a rare and potentially life threatening condition, with mortality greater than 20%. Classic symptoms include chest pain, vomiting, and subcutaneous emphysema, known as the Mackler triad. However, patients can present with a variety of symptoms including neck pain, epigastric pain, hoarse voice, dysphagia, tachycardia, and dyspnea. Early clinical suspicion, diagnosis, and treatment are necessary to decrease chances of a poor outcome. Here, we present a patient whose symptoms were masked by his chronic medical conditions.
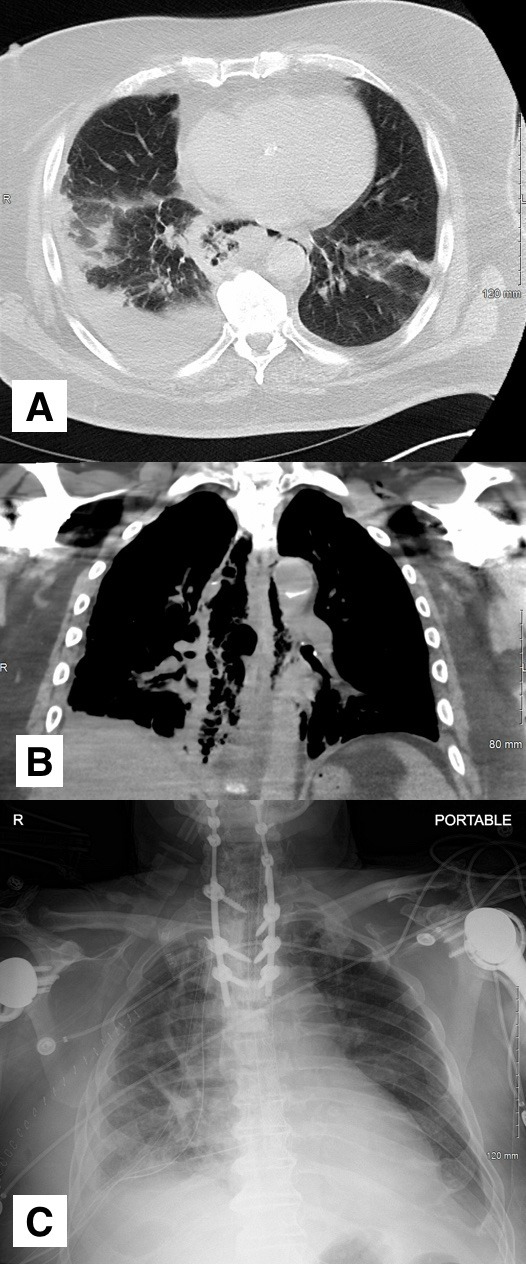
Case Description/Methods: This is an 81 year old Caucasian male with a past medical history of cervical and upper thoracic spinal fusion secondary to advanced arthritis who presented to the emergency department after a low velocity motor vehicle collision (MCV). His only complaint at that time was neck pain, which he describes as chronic, for which he takes daily opioid medication. He became frustrated and left the emergency department against medical advice after initial chest x-ray was obtained, which did not reveal acute findings. He represented to the emergency department after 48 hours, stating that he had run out of his opioid medications and is having continued neck pain. He described episodes of coughing while eating and drinking at home. He was found to have an oxygen saturation of 98% on room air. Knowing that the patient was recently in an MCV, a CT chest without contrast was ordered, demonstrating extensive pneumomediastinum centered around a thick walled esophagus, raising concern for esophageal perforation [A, B]. A Gastrografin esophagram was then completed, which revealed visualization of extraluminal contrast. The patient was initiated on broad spectrum antibiotics with vancomycin and piperacillin-tazobactam. He then underwent thoracotomy with washout, decortication, and esophageal repair [C]. Unfortunately, the patient had a complicated 60 day hospital stay, where he had to undergo multiple surgical procedures for complications related to the esophageal perforation. He was ultimately discharged to an inpatient skilled nursing and rehabilitation facility, where he stayed for an additional 60 days. At the time of discharge, the patient was fully independent for most activities of daily living and was able to ambulate without assistive devices.
Discussion: This case demonstrates the importance of maintaining a high index of suspicion for esophageal perforation in patients involved in trauma, even in the absence of classical symptoms.
Disclosures:
Jeremy Polman, DO, MS, MBA1, Rameela Mahat, MD2, Jobin Philipose, MD3. E0244 - When Chronic Medical Conditions Mask Acute Symptoms: A Case of Esophageal Perforation With Neck Pain, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Baton Rouge General Medical Center, Baton Rouge, LA; 2Baton Rouge General Internal Medicine Residency Program, Baton Rouge, LA; 3Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Esophageal perforation is a rare and potentially life threatening condition, with mortality greater than 20%. Classic symptoms include chest pain, vomiting, and subcutaneous emphysema, known as the Mackler triad. However, patients can present with a variety of symptoms including neck pain, epigastric pain, hoarse voice, dysphagia, tachycardia, and dyspnea. Early clinical suspicion, diagnosis, and treatment are necessary to decrease chances of a poor outcome. Here, we present a patient whose symptoms were masked by his chronic medical conditions.
Case Description/Methods: This is an 81 year old Caucasian male with a past medical history of cervical and upper thoracic spinal fusion secondary to advanced arthritis who presented to the emergency department after a low velocity motor vehicle collision (MCV). His only complaint at that time was neck pain, which he describes as chronic, for which he takes daily opioid medication. He became frustrated and left the emergency department against medical advice after initial chest x-ray was obtained, which did not reveal acute findings. He represented to the emergency department after 48 hours, stating that he had run out of his opioid medications and is having continued neck pain. He described episodes of coughing while eating and drinking at home. He was found to have an oxygen saturation of 98% on room air. Knowing that the patient was recently in an MCV, a CT chest without contrast was ordered, demonstrating extensive pneumomediastinum centered around a thick walled esophagus, raising concern for esophageal perforation [A, B]. A Gastrografin esophagram was then completed, which revealed visualization of extraluminal contrast. The patient was initiated on broad spectrum antibiotics with vancomycin and piperacillin-tazobactam. He then underwent thoracotomy with washout, decortication, and esophageal repair [C]. Unfortunately, the patient had a complicated 60 day hospital stay, where he had to undergo multiple surgical procedures for complications related to the esophageal perforation. He was ultimately discharged to an inpatient skilled nursing and rehabilitation facility, where he stayed for an additional 60 days. At the time of discharge, the patient was fully independent for most activities of daily living and was able to ambulate without assistive devices.
Discussion: This case demonstrates the importance of maintaining a high index of suspicion for esophageal perforation in patients involved in trauma, even in the absence of classical symptoms.
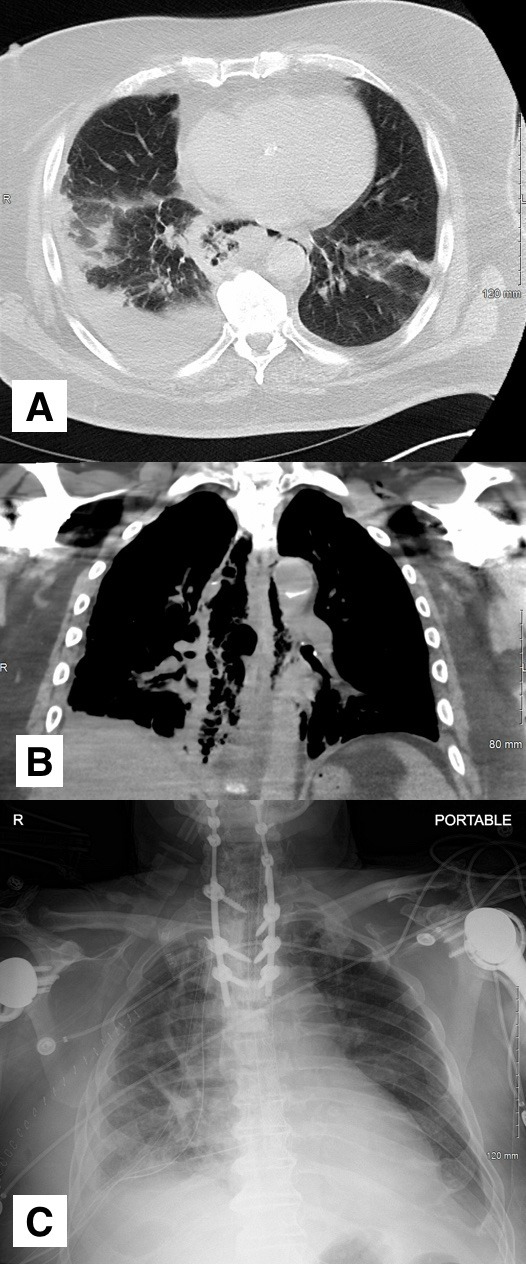
Figure: A) Transverse slice of CT chest demonstrating esophageal perforation with right sided pleural effusion.
B) Coronal slice of CT chest demonstrating esophageal perforation.
C) Portable chest x-ray demonstrating post-operative changes, with esophageal stent in place.
B) Coronal slice of CT chest demonstrating esophageal perforation.
C) Portable chest x-ray demonstrating post-operative changes, with esophageal stent in place.
Disclosures:
Jeremy Polman indicated no relevant financial relationships.
Rameela Mahat indicated no relevant financial relationships.
Jobin Philipose indicated no relevant financial relationships.
Jeremy Polman, DO, MS, MBA1, Rameela Mahat, MD2, Jobin Philipose, MD3. E0244 - When Chronic Medical Conditions Mask Acute Symptoms: A Case of Esophageal Perforation With Neck Pain, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
