Back
Poster Session E - Tuesday Afternoon
E0222 - A Rare Presentation of Esophageal Lichen Planus in a Patient With Collagenous Gastritis and Duodenitis: A Case Study
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
.jpg)
Marlee Hill, BS
University of Oklahoma College of Medicine
Oklahoma City, OK
Presenting Author(s)
Marlee Hill, BS1, Fatima Hassan, MD2, Beth Gillies, MD3, Ijlal Akbar Ali, MD3
1University of Oklahoma College of Medicine, Oklahoma City, OK; 2LSU Health Shreveport, Shreveport, LA; 3University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Lichen planus (LP) is an idiopathic, immune-mediated, chronic inflammatory condition that can involve the skin, hair, nails and mucus membranes. Cutaneous and oral LP are relatively common and present with violaceous pruritic papules or white reticulated striae. Esophageal lichen planus (ELP) is an atypical and underdiagnosed cause of esophagitis and stricture, most common in middle to elderly aged women. We report a case of isolated ELP with concomitant collagenous gastritis (CG) and duodenitis (CD). This case supplements the literature on ELP and details an uncommon constellation of diseases that may support further evaluation in ELP patients to investigate the presence of other associated conditions.
Case Description/Methods: An 80-year-old Caucasian female was referred for further evaluation after having multiple endoscopies with dilation and a gastrostomy tube placement for a refractory esophageal stenosis that led to significant dysphagia, loss of appetite and a 30-pound weight loss. She denied altered bowel habits or skin lesions. Endoscopy revealed sloughing mucosa lining a narrowed esophagus with healthy mucosa in the distal third. The stomach and small bowel mucosa appeared atrophic and pale. Biopsies of the esophagus were suggestive of ELP and the duodenum and stomach biopsies revealed CG and CD. A swallowed budesonide slurry markedly improved her dysphagia and helped regain weight.
Discussion: There should be a high index of suspicion for ELP in patients with the correct demographics presenting with dysphagia, proton pump inhibitor (PPI) refractory esophagitis and stenosis. Endoscopic evaluation should be considered in LP patients to define disease extent. Additional evaluation and biopsies should also be considered if refractory symptoms or those consistent with another disease process are present. Our patient, in addition to ELP, was diagnosed with isolated CG and CD, a rarity when presenting without colonic involvement. Proximal collagenous gastroenteritides–which also show a slight female predominance and autoimmune association–are diagnosed endoscopically and histologically by subepithelial collagen deposition, nodular changes and inflammatory infiltrate.1 The lack of literature and scant incidence of both conditions suggests that further analysis of ELP patients should be considered to determine if there is an association with CG or CD, as this may also shed light on their pathogenesis.
1. Kamimura K, et al. World Journal of Gastrointestinal Endoscopy. 2015;7(3):265-273.
Disclosures:
Marlee Hill, BS1, Fatima Hassan, MD2, Beth Gillies, MD3, Ijlal Akbar Ali, MD3. E0222 - A Rare Presentation of Esophageal Lichen Planus in a Patient With Collagenous Gastritis and Duodenitis: A Case Study, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Oklahoma College of Medicine, Oklahoma City, OK; 2LSU Health Shreveport, Shreveport, LA; 3University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Lichen planus (LP) is an idiopathic, immune-mediated, chronic inflammatory condition that can involve the skin, hair, nails and mucus membranes. Cutaneous and oral LP are relatively common and present with violaceous pruritic papules or white reticulated striae. Esophageal lichen planus (ELP) is an atypical and underdiagnosed cause of esophagitis and stricture, most common in middle to elderly aged women. We report a case of isolated ELP with concomitant collagenous gastritis (CG) and duodenitis (CD). This case supplements the literature on ELP and details an uncommon constellation of diseases that may support further evaluation in ELP patients to investigate the presence of other associated conditions.
Case Description/Methods: An 80-year-old Caucasian female was referred for further evaluation after having multiple endoscopies with dilation and a gastrostomy tube placement for a refractory esophageal stenosis that led to significant dysphagia, loss of appetite and a 30-pound weight loss. She denied altered bowel habits or skin lesions. Endoscopy revealed sloughing mucosa lining a narrowed esophagus with healthy mucosa in the distal third. The stomach and small bowel mucosa appeared atrophic and pale. Biopsies of the esophagus were suggestive of ELP and the duodenum and stomach biopsies revealed CG and CD. A swallowed budesonide slurry markedly improved her dysphagia and helped regain weight.
Discussion: There should be a high index of suspicion for ELP in patients with the correct demographics presenting with dysphagia, proton pump inhibitor (PPI) refractory esophagitis and stenosis. Endoscopic evaluation should be considered in LP patients to define disease extent. Additional evaluation and biopsies should also be considered if refractory symptoms or those consistent with another disease process are present. Our patient, in addition to ELP, was diagnosed with isolated CG and CD, a rarity when presenting without colonic involvement. Proximal collagenous gastroenteritides–which also show a slight female predominance and autoimmune association–are diagnosed endoscopically and histologically by subepithelial collagen deposition, nodular changes and inflammatory infiltrate.1 The lack of literature and scant incidence of both conditions suggests that further analysis of ELP patients should be considered to determine if there is an association with CG or CD, as this may also shed light on their pathogenesis.
1. Kamimura K, et al. World Journal of Gastrointestinal Endoscopy. 2015;7(3):265-273.
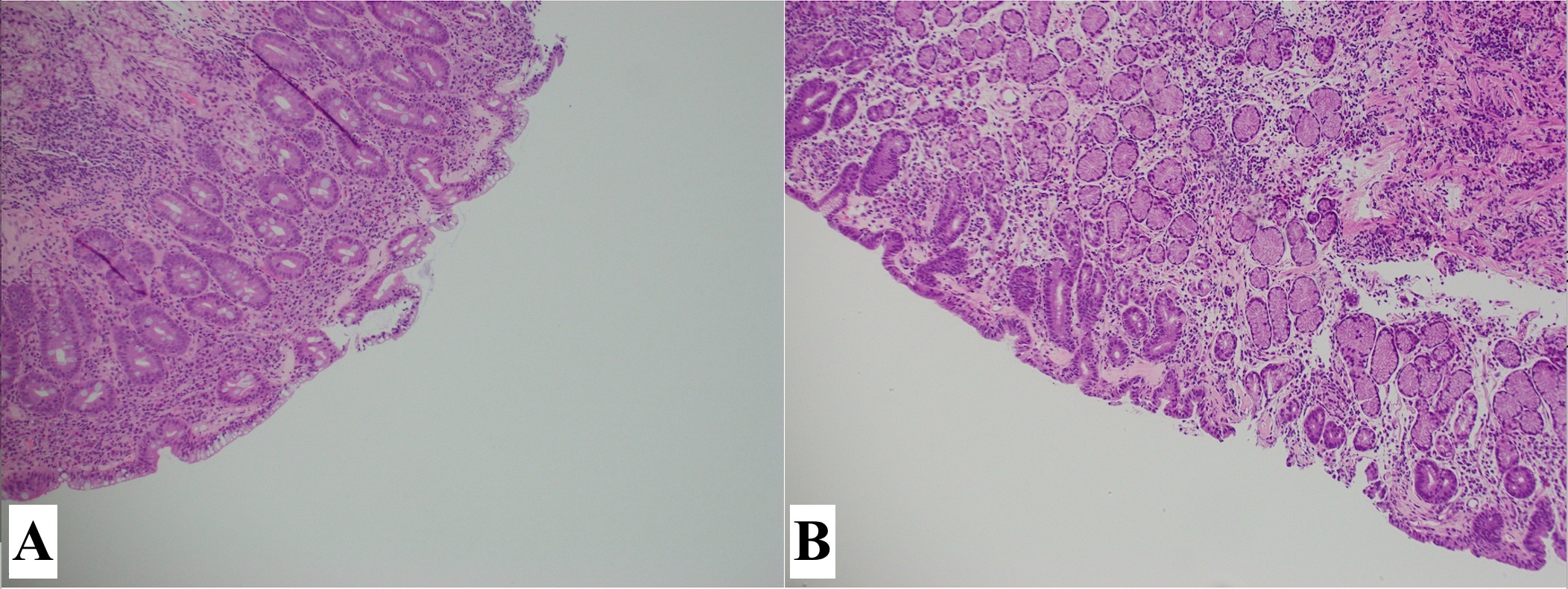
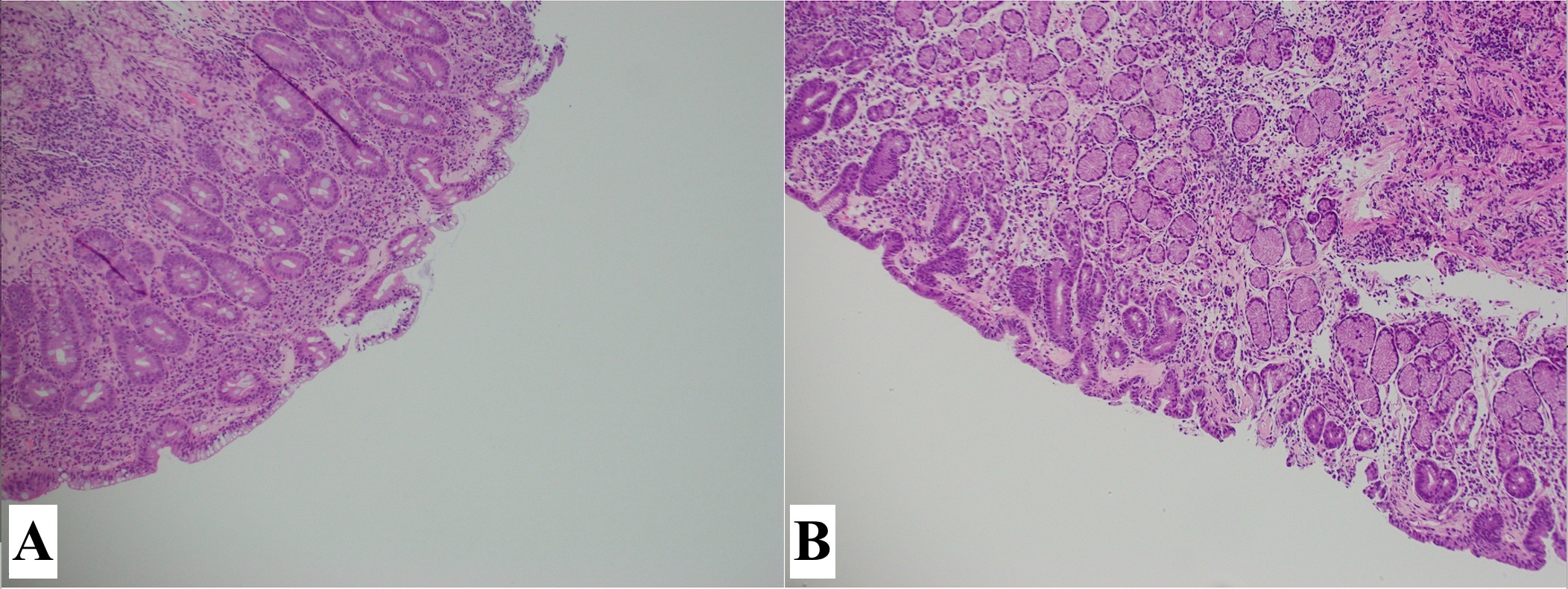
Figure: Figure 1. Histological findings of collagenous gastritis and duodenitis. (A) Duodenum depicting signs of villous atrophy and subepithelial collagen deposition with background chronic inflammation; (B) Gastric antrum depicting subepithelial collagen deposition with background chronic inflammation.
Disclosures:
Marlee Hill indicated no relevant financial relationships.
Fatima Hassan indicated no relevant financial relationships.
Beth Gillies indicated no relevant financial relationships.
Ijlal Akbar Ali indicated no relevant financial relationships.
Marlee Hill, BS1, Fatima Hassan, MD2, Beth Gillies, MD3, Ijlal Akbar Ali, MD3. E0222 - A Rare Presentation of Esophageal Lichen Planus in a Patient With Collagenous Gastritis and Duodenitis: A Case Study, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

