Back
Poster Session A - Sunday Afternoon
A0207 - A Unique Endoscopic Finding in an HIV/AIDS Patient With Dysphagia
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Andrew W. Zarker, BS
McGovern Medical School at UTHealth
Houston, TX
Presenting Author(s)
Andrew W. Zarker, BS, Kavya Kelagere Mayigegowda, MD, Tanima Jana, MD
McGovern Medical School at UTHealth, Houston, TX
Introduction: There are many etiologies of dysphagia in patients with HIV/AIDS, including infection, structural issues, or medications. A broad differential is needed to properly diagnose and treat these patients. Here, we present a case of dysphagia in an HIV/AIDS patient related to esophageal intramural pseudodiverticulosis (EIPD).
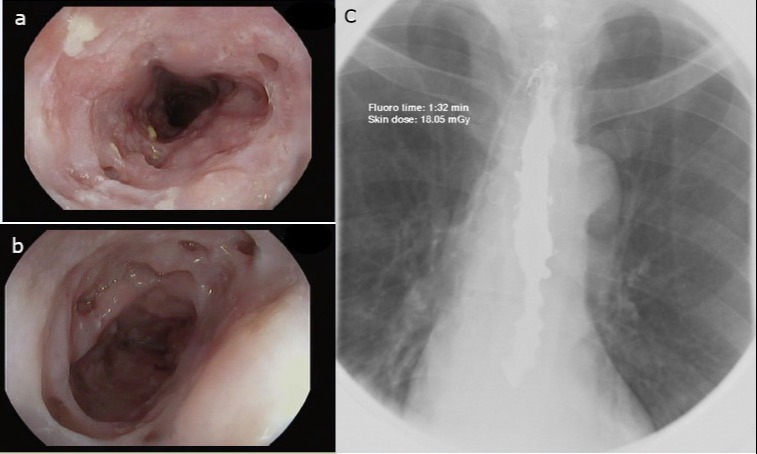
Case Description/Methods: A 58-year-old man with HIV/AIDS presented with a 2-week history of dysphagia. He had been non-compliant with highly active antiretroviral therapy (HAART), and his CD4 count at presentation was noted to be < 20. His past medical history was notable for hypertension, chronic kidney disease, Candida esophagitis, and Mallory-Weiss syndrome. He underwent an esophagogastroduodenoscopy (EGD), which revealed numerous outpouchings and white plaques in the mid esophagus (Figures 1a and b). Esophageal brushings confirmed Candida infection, and biopsies were positive for cytomegalovirus (CMV). A barium esophagram showed outpouchings throughout the esophagus, without any evidence of perforation (Figure 1c). No stricture was evident on EGD or barium esophagram. The patient was diagnosed with EIPD and treated with fluconazole, a proton pump inhibitor, and valganciclovir, with improvement in symptoms.
Discussion: EIPD is characterized by the development of multiple small flask-shaped outpouchings in the esophagus. Patients with reflux esophagitis, Candida esophagitis, diabetes mellitus, HIV, and eosinophilic esophagitis are at higher risk for developing EIPD. There are approximately 250 published cases of EIPD in the literature, and the prevalence of EIPD is estimated to be 5-50 per 100,000 cases. Development of pseudodiverticula in the esophagus is suggested to be secondary to chronic inflammation, obstruction of the submucosal glands due to debris, or increased intraluminal pressure proximal to a luminal obstruction. The diagnosis is primarily made with EGD, barium esophagram, or computerized tomography. The treatment for EIPD includes treatment of underlying conditions and endoscopic dilation of strictures when they are present [1]. Our patient had several risk factors for development of EIPD such as Candida esophagitis, Mallory-Weiss syndrome, and HIV. However, a prior association between EIPD and CMV esophagitis has not been reported. Here, we highlight CMV esophagitis as a potential risk factor for development of EIPD.
1. Hentschel F, Lüth S. Clinical and endoscopic characteristics of diffuse esophageal intramural pseudo-diverticulosis. Oct 2020;17(4):492-501.
Disclosures:
Andrew W. Zarker, BS, Kavya Kelagere Mayigegowda, MD, Tanima Jana, MD. A0207 - A Unique Endoscopic Finding in an HIV/AIDS Patient With Dysphagia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
McGovern Medical School at UTHealth, Houston, TX
Introduction: There are many etiologies of dysphagia in patients with HIV/AIDS, including infection, structural issues, or medications. A broad differential is needed to properly diagnose and treat these patients. Here, we present a case of dysphagia in an HIV/AIDS patient related to esophageal intramural pseudodiverticulosis (EIPD).
Case Description/Methods: A 58-year-old man with HIV/AIDS presented with a 2-week history of dysphagia. He had been non-compliant with highly active antiretroviral therapy (HAART), and his CD4 count at presentation was noted to be < 20. His past medical history was notable for hypertension, chronic kidney disease, Candida esophagitis, and Mallory-Weiss syndrome. He underwent an esophagogastroduodenoscopy (EGD), which revealed numerous outpouchings and white plaques in the mid esophagus (Figures 1a and b). Esophageal brushings confirmed Candida infection, and biopsies were positive for cytomegalovirus (CMV). A barium esophagram showed outpouchings throughout the esophagus, without any evidence of perforation (Figure 1c). No stricture was evident on EGD or barium esophagram. The patient was diagnosed with EIPD and treated with fluconazole, a proton pump inhibitor, and valganciclovir, with improvement in symptoms.
Discussion: EIPD is characterized by the development of multiple small flask-shaped outpouchings in the esophagus. Patients with reflux esophagitis, Candida esophagitis, diabetes mellitus, HIV, and eosinophilic esophagitis are at higher risk for developing EIPD. There are approximately 250 published cases of EIPD in the literature, and the prevalence of EIPD is estimated to be 5-50 per 100,000 cases. Development of pseudodiverticula in the esophagus is suggested to be secondary to chronic inflammation, obstruction of the submucosal glands due to debris, or increased intraluminal pressure proximal to a luminal obstruction. The diagnosis is primarily made with EGD, barium esophagram, or computerized tomography. The treatment for EIPD includes treatment of underlying conditions and endoscopic dilation of strictures when they are present [1]. Our patient had several risk factors for development of EIPD such as Candida esophagitis, Mallory-Weiss syndrome, and HIV. However, a prior association between EIPD and CMV esophagitis has not been reported. Here, we highlight CMV esophagitis as a potential risk factor for development of EIPD.
1. Hentschel F, Lüth S. Clinical and endoscopic characteristics of diffuse esophageal intramural pseudo-diverticulosis. Oct 2020;17(4):492-501.
Figure: EGD (a and b) and barium esophagram (c) findings.
Disclosures:
Andrew Zarker indicated no relevant financial relationships.
Kavya Kelagere Mayigegowda indicated no relevant financial relationships.
Tanima Jana indicated no relevant financial relationships.
Andrew W. Zarker, BS, Kavya Kelagere Mayigegowda, MD, Tanima Jana, MD. A0207 - A Unique Endoscopic Finding in an HIV/AIDS Patient With Dysphagia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
