Back
Poster Session C - Monday Afternoon
C0234 - A Case of Esophago-Pulmonary Fistula From Esophageal Candidiasis Diagnosed on Endoscopy
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Astin Worden, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Astin Worden, MD, Rawan Aljaras, MD, Mohsin Mukhtar, MD, MBA, Umer A. Bhatti, MBBS, Hala Fatima, MD
Indiana University School of Medicine, Indianapolis, IN
Introduction: Esophago-pulmonary fistulas (EPFs) are abnormal connections between the esophagus and lungs that are rarely seen despite the proximity of the two structures. They are associated with high morbidity and mortality. Fistulization between the esophagus and lungs is a known complication of pneumonectomy procedures, but other causes include malignancies and infection.
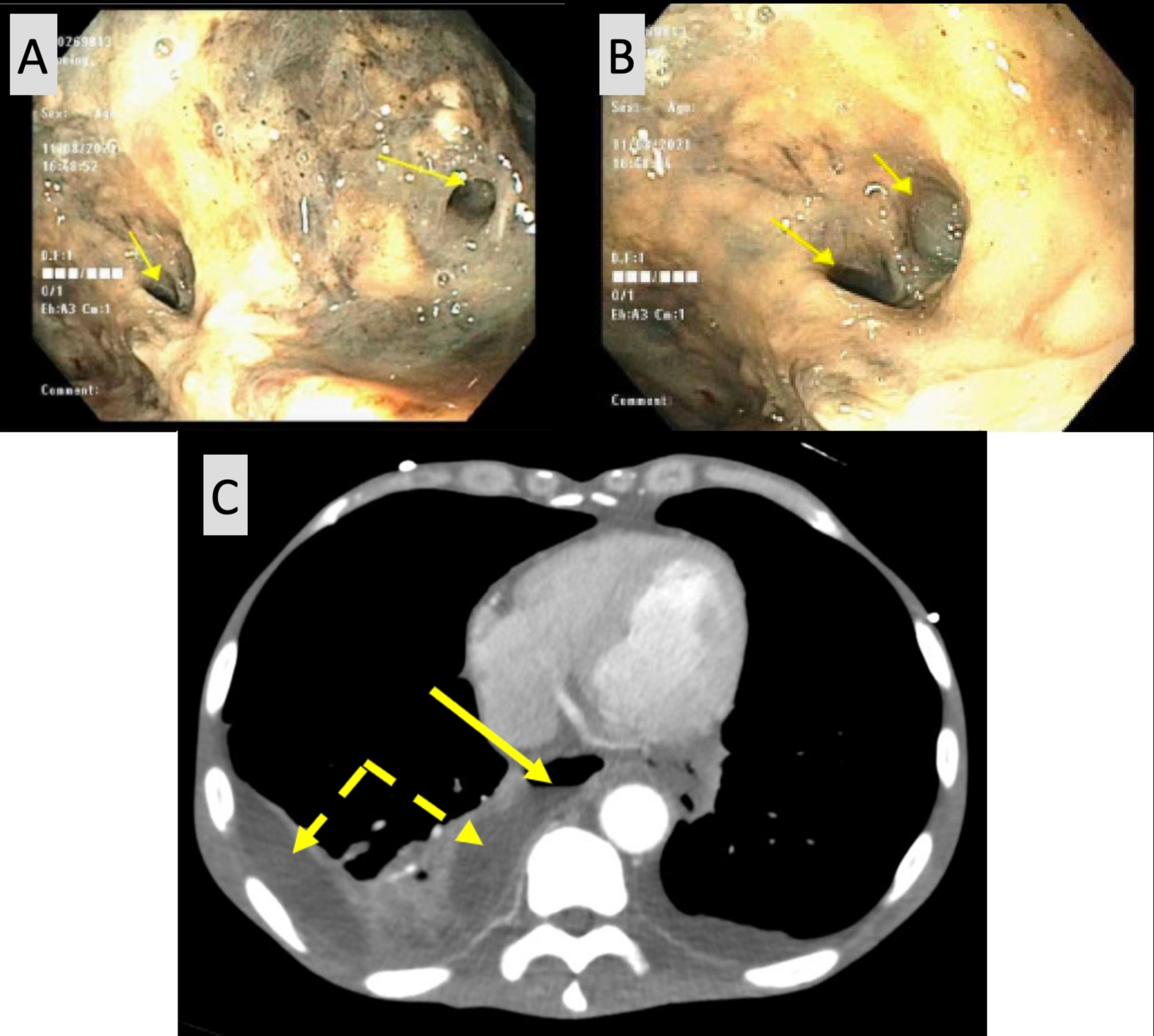
Case Description/Methods: A 61-year-old male with a history of tobacco and alcohol use disorder, diabetes mellitus, and esophageal candidiasis, with both Candida Glabrata (C.Glabrata) and Candida Albicans (C.Albicans) isolated on biopsies from an otherwise normal endoscopy 4 months prior presented with presumed septic shock and melena. Blood cultures were positive for C. Glabrata. Esophagogastroduodenoscopy (EGD) was done and revealed a fistulous tract leading to a bronchial bifurcation consistent with an esophago-pulmonary fistula with necrotic and friable tissue surrounding it (image A and B), in addition to grade D esophagitis. Subsequent CT chest showed definite right and possible left esophago-pleural fistulization with associated right loculated pleural effusion and small left pleural effusion (image C). No evidence of pulmonary malignancy or pulmonary tuberculosis was noted on imaging. Serum interferon gamma release assay and 3 sets of sputum acid fast bacillus testing for tuberculosis testing were negative. Thoracic Surgery were consulted but the procedure offered was multistage and did not align with patient's goals of care. The patient continued to decline despite antifungal and antibiotic treatment and was ultimately transitioned to hospice care.
Discussion: While formal tissue diagnosis was not obtained in this case due to patient’s tenuous condition, the etiology of EPF was presumed to be invasive esophageal candidiasis infection, especially in the absence of malignancy on imaging and recent EGD. Interestingly, fistulas related to empyema were commonly reported in the pre-antibiotic era. A CT scan of the chest is useful for early diagnosis of EPF. While different modalities help establish the diagnosis of EPF, clinical suspicion remains key in initiating appropriate investigation.
Disclosures:
Astin Worden, MD, Rawan Aljaras, MD, Mohsin Mukhtar, MD, MBA, Umer A. Bhatti, MBBS, Hala Fatima, MD. C0234 - A Case of Esophago-Pulmonary Fistula From Esophageal Candidiasis Diagnosed on Endoscopy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Indiana University School of Medicine, Indianapolis, IN
Introduction: Esophago-pulmonary fistulas (EPFs) are abnormal connections between the esophagus and lungs that are rarely seen despite the proximity of the two structures. They are associated with high morbidity and mortality. Fistulization between the esophagus and lungs is a known complication of pneumonectomy procedures, but other causes include malignancies and infection.
Case Description/Methods: A 61-year-old male with a history of tobacco and alcohol use disorder, diabetes mellitus, and esophageal candidiasis, with both Candida Glabrata (C.Glabrata) and Candida Albicans (C.Albicans) isolated on biopsies from an otherwise normal endoscopy 4 months prior presented with presumed septic shock and melena. Blood cultures were positive for C. Glabrata. Esophagogastroduodenoscopy (EGD) was done and revealed a fistulous tract leading to a bronchial bifurcation consistent with an esophago-pulmonary fistula with necrotic and friable tissue surrounding it (image A and B), in addition to grade D esophagitis. Subsequent CT chest showed definite right and possible left esophago-pleural fistulization with associated right loculated pleural effusion and small left pleural effusion (image C). No evidence of pulmonary malignancy or pulmonary tuberculosis was noted on imaging. Serum interferon gamma release assay and 3 sets of sputum acid fast bacillus testing for tuberculosis testing were negative. Thoracic Surgery were consulted but the procedure offered was multistage and did not align with patient's goals of care. The patient continued to decline despite antifungal and antibiotic treatment and was ultimately transitioned to hospice care.
Discussion: While formal tissue diagnosis was not obtained in this case due to patient’s tenuous condition, the etiology of EPF was presumed to be invasive esophageal candidiasis infection, especially in the absence of malignancy on imaging and recent EGD. Interestingly, fistulas related to empyema were commonly reported in the pre-antibiotic era. A CT scan of the chest is useful for early diagnosis of EPF. While different modalities help establish the diagnosis of EPF, clinical suspicion remains key in initiating appropriate investigation.
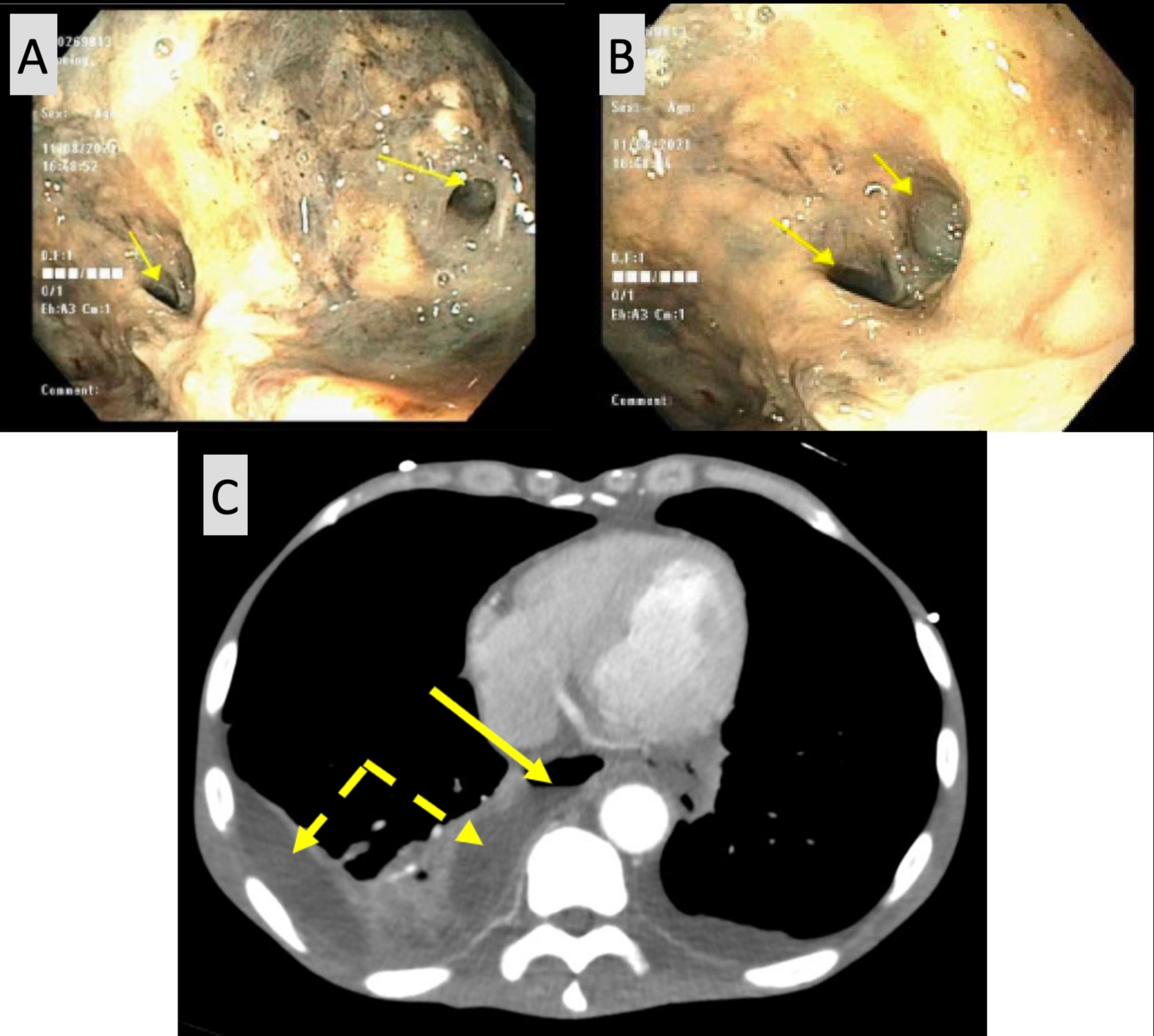
Figure: Images A and B: Lower third of esophagus with necrotic tissue surrounding esophago-pleural fistula (arrows). Image C: (Axial CT showing an air-fluid level within the distal esophagus with loss of the fat plane between the esophagus (arrow) and the loculated right pleural effusion (dashed arrows), compatible with an esophago-pleural fistula).
Disclosures:
Astin Worden indicated no relevant financial relationships.
Rawan Aljaras indicated no relevant financial relationships.
Mohsin Mukhtar indicated no relevant financial relationships.
Umer Bhatti indicated no relevant financial relationships.
Hala Fatima indicated no relevant financial relationships.
Astin Worden, MD, Rawan Aljaras, MD, Mohsin Mukhtar, MD, MBA, Umer A. Bhatti, MBBS, Hala Fatima, MD. C0234 - A Case of Esophago-Pulmonary Fistula From Esophageal Candidiasis Diagnosed on Endoscopy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
